Introduction
Osteosarcoma is the most common primary bone malignancy of non-hematopoietic origin. Several subtypes of osteosarcoma have been described on pathological evaluation- conventional, small cell, periosteal, parosteal, high-grade surface, low-grade central, giant cell, and telangiectatic types.[1] Telangiectatic osteosarcoma is a rare, aggressive, high-grade malignant neoplasm, accounting for 2 to 12% of all osteosarcoma cases.[2][1] It is a rare variant of osteosarcoma characterized by distinctive radiographic, gross, and microscopic features. Due to identical radiographic as well as pathological findings, it poses a diagnostic challenge concerning aneurysmal bone cysts and giant cell tumors of bone.[3] Paget first described this variant in 1853. However, Ewing first thought that it was a type of osteosarcoma. Despite more than 150 years of its description, there lacks a consensus regarding the optimal management for these tumors.[4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The exact etiology of telangiectatic osteosarcoma is still unknown, and so are the predisposing factors. It becomes challenging to conduct epidemiological studies and investigate the etiologic factors due to the rare occurrence of the disease. However, some anecdotal reports described genetic components due to the presence of the disease in family members.[5] Telangiectatic osteosarcoma was described in the metaphysis of the distal tibia in an 11-year-old girl and the lamina of the thoracic vertebra in an 8-year-old boy who was a cousin. On histopathological evaluation, dilated and proliferated blood cavities were seen along with anaplastic tumor cells and osteoid production, favoring the diagnosis of telangiectatic osteosarcoma. The clinical outcome was favorable in both cases.[5] Also, three well-documented cases of extraskeletal telangiectatic osteosarcoma of the soft tissues were described; the daughter of one of the cases had died previously of high-grade intramedullary bone osteosarcoma.[6]
Epidemiology
Telangiectatic osteosarcoma is predominantly seen in children, adolescents, and young adults. The mean age at presentation of telangiectatic osteosarcoma is 17.5 years (range from 15 to 20 years) with a male-to-female ratio of 2 to 1.[2] The distal femoral metaphysis is the single most common anatomic site (42%), followed by the proximal tibia (17%), the proximal humerus (9%), and the proximal femur (8%).
Flat bone involvement is relatively rare, with around 8% incidence of non-appendicular non-spinal sites.[7][8] Uncommon sites of telangiectatic osteosarcoma include the scapula, the ribs, the sternum, the innominate bone, the cranial vault, and the mandible. Telangiectatic osteosarcoma of the spine represents 2% of all cases of primary vertebral osteosarcomas.[9] Extra-osseous telangiectatic osteosarcoma is rare, with telangiectatic osteosarcoma arising in the soft tissues of the thigh, the forearm, and the popliteal fossa.[6]
Pathophysiology
Histogenesis
Telangiectatic osteosarcoma is presumed to derive from either transformed osteoblasts or stem cells of mesenchymal origin. Angiosarcomatous features are present in addition to osteoblast-like and fibroblast-like cells at the ultrastructural level. Tight intercellular junctions, Weibel-Palade bodies, and pinocytic vesicles are visible within the cell cytoplasm. These features suggest that telangiectatic osteosarcoma derives from multipotential stem cells of mesenchymal origin.[10][2][11]
Cytogenetics
Only seven cases of telangiectatic osteosarcoma to date have had genetic studies. The cytogenetic analysis identified trisomy 3 in one case, and in three other tumors, more complex chromosomal changes were reported.[12][13] Metaphase CGH identified an average of 2.5 aberrations in two telangiectatic osteosarcomas, and array CGH identified only three regional gains at 1q21-23.2, 1q25.2-31.1, and 7q21.13-21.2 in one tumor.[14] This suggests that telangiectatic tumors are genetically less complex than conventional osteosarcoma.
Histopathology
On gross as well as microscopic appearance, telangiectatic osteosarcoma very closely resembles aneurysmal bone cysts.[4] Therefore, the resected surgical specimens of telangiectatic osteosarcoma must undergo meticulous sampling.[2] Because of the cystic and lytic nature of the tumor, a core-needle biopsy may not provide an adequate and appropriate sample for the diagnosis. Hence, the establishment of the diagnosis often gets delayed leading to delayed treatment with the outcome affected adversely.[15][16][2] The complete face of the bone must be sampled to document the percentages of the viable and necrotic tumors.[2] Yin et al. developed and described a diagnostic model for the differentiation of telangiectatic osteosarcoma from an aneurysmal bone cyst.[17]
Macroscopic Findings
Macroscopic examination reveals a hemorrhagic multicystic lesion filled with blood clots. Telangiectatic osteosarcomas have the classic description as ''a bag of blood.'' They are, by definition, composed of approximately 90% cystic components before treatment.[8] A fleshy sarcomatous component is typically not present. The cystic spaces can vary considerably in size and may occasionally measure several centimeters in diameter. More often, there is a mixture of large cystic and spongy areas. The spongy areas represent tissue honeycombed with smaller cysts measuring up to several millimeters. The borders of the lesion are usually well-demarcated, but often there are features of invasive growth with extensive irregular cortical erosion, complete disruption of cortical continuity, and invasion of soft tissue.
Microscopic Findings
Histologically, telangiectatic osteosarcoma is composed of blood-filled or empty cystic spaces resembling aneurysmal bone cysts. The septa are populated by pleomorphic cells with important nuclear hyperchromasia and also contain osteoclast-like giant cells. Osteoid formation is usually focal and confluent. Because telangiectatic osteosarcoma is sometimes not adequately sampled by core-needle biopsy due to its lytic and cystic nature, cellular atypia and osteoid formation may be absent, which may lead to misdiagnosis.[2] Previously, the osteoid production by the malignant cells was deemed essential for diagnosing telangiectatic osteosarcoma. However, later various cases were reported with a lack of osteoid production.[4] Thickened septa with nodularity, along with the presence of malignant cells with nuclear pleomorphism and cellular atypia, microscopically differentiate telangiectatic osteosarcoma from aneurysmal bone cysts.[17]
Immunochemistry
No immunohistochemical studies are useful in the diagnosis of telangiectatic osteosarcoma.
History and Physical
There is no difference in the clinical presentation of telangiectatic and conventional osteosarcoma. Local pain and/or soft tissue mass are the most common symptoms of telangiectatic osteosarcoma. Sometimes, the patients may present with a pathologic fracture.[18][19] Occasionally, a vascular bruit may be heard over the tumor. As with any other malignant tumor, a thorough general physical and systemic clinical examination is mandatory to look for evidence of any metastases.
Evaluation
Several imaging modalities are available for establishing the diagnosis of telangiectatic osteosarcoma. They include:
- Plain radiographs
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
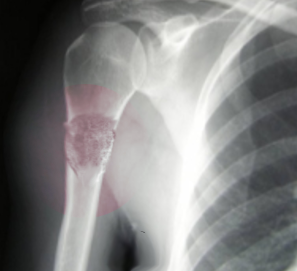
Radiographic Findings
Telangiectatic osteosarcoma is typically a purely lytic lesion with a permeative destructive growth pattern. This rapidly growing tumor often expands the contour of bone and shows features of cortical disruption with minimal or no periosteal new bone formation. The massive expansile growth pattern of telangiectatic osteosarcoma can superficially simulate an aneurysmal bone cyst. Telangiectatic osteosarcoma can have a deceptively innocent radiographic appearance with sharply demarcated margins, simulating a benign bone cyst. Aneurysmal bone cysts generally have type 1A or 1B patterns of geographic bone destruction.[20] Presence of soft tissue mass, Codman triangle, and matrix mineralization point towards the diagnosis of telangiectatic osteosarcoma. MRI best documents the multilocular cystic nature of the lesion and the so-called fluid level sign.[21]
T1-weighted MRI shows heterogeneous low signal intensity, and T2-weighted images show high signal intensity with several cystic foci, fluid levels, and an extra-skeletal extension of the tumor, similar to an aneurysmal cyst, but with irregular walls, septae, and nodular and solid components.[7] Zishan et al. described that presence of fluid-fluid levels in the lesion was the most useful differentiating MRI feature between telangiectatic osteosarcoma and aneurysmal bone cyst. As compared to 74% of the osteosarcomas demonstrating a fluid level, 95% of the bone cysts had the presence of fluid levels. Also, only aneurysmal bone cysts had lesions that were completely filled with a fluid-fluid level.[20]
The criteria for diagnosing telangiectatic osteosarcoma include the following:
- Radiographically, a destructive, osteolytic tumor with little or no matrix mineralization or periosteal new bone formation
- Cystic/cavitary gross specimen with little solid tumor tissue and no areas of a dense bone
- Histologically, a tumor with single or multiple cystic cavities containing blood or necrotic tissue, with thickened septa composed of anaplastic tumor cells[4]
The high alkaline phosphatase level frequently seen in osteosarcoma is not a feature of telangiectatic osteosarcoma. On the other hand, the evaluation of platelet count, white cell count, lactate dehydrogenase, and alkaline phosphatase have been described for differentiating telangiectatic osteosarcoma from aneurysmal bone cysts. The sarcomas had a higher value of platelet count, white cell count, alkaline phosphatase, and lactate dehydrogenase than the aneurysmal bone cysts.[17]
Treatment / Management
Previously, the prognosis and clinical outcome of telangiectatic osteosarcoma were considered to be poor. However, with the advent of chemotherapy, the prognosis has significantly improved, with around a 60% survival rate at ten years, which is similar to that of conventional osteosarcoma.[22] Patients with telangiectatic osteosarcoma receive neo-adjuvant chemotherapy followed by surgical excision, further followed by adjuvant chemotherapy/ radiotherapy. The pre-chemotherapy era required amputation in most cases of telangiectatic osteosarcoma. However, limb-sparing surgery is now possible in most cases, even with pathological fractures.[23][22][24] The extent of surgery depends on the size, location, and response to the neoadjuvant therapy. Adjuvant chemotherapy can offer some advantages if metastatic disease is present.(B2)
Colomina et al. reported the outcome of 8 patients with telangiectatic osteosarcoma with pathologic fractures. They described that the presence of a pathologic fracture did not worsen the outcome and had similar survival and recurrence rates.[24] Similarly, in a retrospective review of 87 cases of telangiectatic osteosarcoma, Angelini et al. reported a survival rate of 60% at ten years. The majority of the patients were cured with neoadjuvant chemotherapy and limb-sparing surgery. They found tumor response to chemotherapy as the only significant prognostic factor affecting survival.[22](B2)
Differential Diagnosis
The most common differential diagnosis is an aneurysmal bone cyst which closely mimics the radiographic, gross as well as microscopic features of telangiectatic osteosarcoma. This often delays the diagnosis leading to the delay in starting optimal treatment. Other differential diagnoses include:
- Giant cell tumor of bone
- Brodie abscess
- Blood clot
- Malignant fibrous histiocytoma
- Fibrosarcoma[4]
Treatment Planning
Chemotherapeutic protocols for telangiectatic osteosarcoma are similar to those of conventional osteosarcoma. Patients will have two to six cycles of chemotherapy administered before surgery. The common chemotherapeutic agents used include cisplatin, carboplatin, methotrexate, doxorubicin, and ifosfamide.[25] Among these, at least two agents need inclusion in a dual-drug therapy regimen. The effect of chemotherapy on telangiectatic osteosarcoma must undergo reassessment. The percentage of tumor necrosis needs to be assessed in the pathological evaluation of the surgical specimen, as <90% necrosis mandates a change in the chemotherapeutic regimen.[4]
Staging
The two common staging systems for telangiectatic osteosarcoma include the Enneking system for malignant bone neoplasms and the American Joint Committee on Cancer (AJCC) system for staging bone sarcomas. The Enneking system includes tumor histological grade, the local extent of the tumor- intracompartmental or extracompartmental and the presence of metastasis. The AJCC system considers tumor histological grade, tumor size, and the presence and location of metastases.[26]
Prognosis
Telangiectatic osteosarcoma usually shows a better response to chemotherapy than conventional osteosarcoma. Survival rates with current chemotherapy protocols are within the range of 65% after five years.[27] The pattern of metastatic spread of telangiectatic osteosarcoma is similar to that seen in conventional osteosarcoma.
Tumor necrosis greater than 95% is considered one of the most important prognostic factors.[28] Additionally, uninvolved neurovascular bundles and soft tissue and bone resection margins are essential for a favorable prognosis.[2] Yin et al. reported that the level of lactate dehydrogenase and tumor volume were predictive prognostic factors, and the presence of a pathologic fracture did not affect the outcome.[17]
Complications
The complications in managing telangiectatic osteosarcoma include local recurrence, metastases, decreased survival, implant failure, infection, and cardiotoxicity due to chemotherapy.[4]
Deterrence and Patient Education
Telangiectatic osteosarcoma is an aggressive and rare variant of osteosarcoma. In contrast to the previous reports, its prognosis is comparable to conventional osteosarcoma. These tumors have a good response to chemotherapy. However, these tumors have a higher incidence of pathologic fracture owing to the cystic nature of the lesion that weakens the bone.[4]
Enhancing Healthcare Team Outcomes
Telangiectatic osteosarcoma is a rare and aggressive variant of osteosarcoma with distinctive radiological and pathological features. It poses diagnostic difficulties, mainly with an aneurysmal bone cyst. Distinguishing between these two entities is vital since their management and prognosis differ significantly. Telangiectatic osteosarcoma is ideally managed by an interprofessional team that consists of orthopedists, oncologists, radiologists, pathologists, pharmacists, and specialty care nurses. Pharmacists review chemotherapeutic regimens, check for drug-drug interactions, and provide patient and family education. Specialty care oncology nurses administer chemotherapy, educate patients and their families, monitor for side effects, and give the team feedback on the patient's condition. All team members must maintain accurate and updated patient documentation so all caregivers can access accurate, up-to-date patient data. Interprofessional patient care will result in improved diagnosis, treatment, and outcomes for patients with telangiectatic osteosarcoma. [Level 5]
Media
(Click Image to Enlarge)
References
Yarmish G,Klein MJ,Landa J,Lefkowitz RA,Hwang S, Imaging characteristics of primary osteosarcoma: nonconventional subtypes. Radiographics : a review publication of the Radiological Society of North America, Inc. 2010 Oct [PubMed PMID: 21071381]
Sangle NA,Layfield LJ, Telangiectatic osteosarcoma. Archives of pathology [PubMed PMID: 22540307]
Turel MK,Joseph V,Singh V,Moses V,Rajshekhar V, Primary telangiectatic osteosarcoma of the cervical spine. Journal of neurosurgery. Spine. 2012 Apr [PubMed PMID: 22225487]
Level 3 (low-level) evidenceLiu JJ,Liu S,Wang JG,Zhu W,Hua YQ,Sun W,Cai ZD, Telangiectatic osteosarcoma: a review of literature. OncoTargets and therapy. 2013 [PubMed PMID: 23745051]
Nishida J,Abe M,Shiraishi H,Shimamura T,Tamura G,Satoh T,Ehara S, Familial occurrence of telangiectatic osteosarcoma: cousin cases. Journal of pediatric orthopedics. 1994 Jan-Feb [PubMed PMID: 8113361]
Level 3 (low-level) evidenceMirra JM,Fain JS,Ward WG,Eckardt JJ,Eilber F,Rosen G, Extraskeletal telangiectatic osteosarcoma. Cancer. 1993 May 15; [PubMed PMID: 8490830]
Level 3 (low-level) evidenceMurphey MD,wan Jaovisidha S,Temple HT,Gannon FH,Jelinek JS,Malawer MM, Telangiectatic osteosarcoma: radiologic-pathologic comparison. Radiology. 2003 Nov [PubMed PMID: 14512511]
Level 2 (mid-level) evidenceHuvos AG,Rosen G,Bretsky SS,Butler A, Telangiectatic osteogenic sarcoma: a clinicopathologic study of 124 patients. Cancer. 1982 Apr 15 [PubMed PMID: 6950802]
Level 2 (mid-level) evidenceIlaslan H,Sundaram M,Unni KK,Shives TC, Primary vertebral osteosarcoma: imaging findings. Radiology. 2004 Mar [PubMed PMID: 14749514]
Level 2 (mid-level) evidenceRoessner A,Hobik HP,Immenkamp M,Grundmann E, Ultrastructure of telangiectatic osteosarcoma. Journal of cancer research and clinical oncology. 1979 Oct [PubMed PMID: 293331]
Level 3 (low-level) evidenceMetcalf DJ,Nightingale TD,Zenner HL,Lui-Roberts WW,Cutler DF, Formation and function of Weibel-Palade bodies. Journal of cell science. 2008 Jan 1 [PubMed PMID: 18096688]
Level 3 (low-level) evidenceFletcher JA,Gebhardt MC,Kozakewich HP, Cytogenetic aberrations in osteosarcomas. Nonrandom deletions, rings, and double-minute chromosomes. Cancer genetics and cytogenetics. 1994 Oct [PubMed PMID: 7923089]
Hoogerwerf WA,Hawkins AL,Perlman EJ,Griffin CA, Chromosome analysis of nine osteosarcomas. Genes, chromosomes & cancer. 1994 Feb [PubMed PMID: 7513549]
Zielenska M,Marrano P,Thorner P,Pei J,Beheshti B,Ho M,Bayani J,Liu Y,Sun BC,Squire JA,Hao XS, High-resolution cDNA microarray CGH mapping of genomic imbalances in osteosarcoma using formalin-fixed paraffin-embedded tissue. Cytogenetic and genome research. 2004 [PubMed PMID: 15305059]
Weiss A,Khoury JD,Hoffer FA,Wu J,Billups CA,Heck RK,Quintana J,Poe D,Rao BN,Daw NC, Telangiectatic osteosarcoma: the St. Jude Children's Research Hospital's experience. Cancer. 2007 Apr 15 [PubMed PMID: 17351949]
Moore DD, Luu HH. Osteosarcoma. Cancer treatment and research. 2014:162():65-92. doi: 10.1007/978-3-319-07323-1_4. Epub [PubMed PMID: 25070231]
Yin JQ,Fu YW,Xie XB,Cheng XY,Yang XY,Liu WH,Tu J,Gao ZH,Shen JN, Telangiectatic osteosarcoma: Outcome analyses and a diagnostic model for differentiation from aneurysmal bone cyst. Journal of bone oncology. 2018 Jun [PubMed PMID: 29892520]
Papagelopoulos PJ,Mavrogenis AF,Savvidou OD,Benetos IS,Galanis EC,Soucacos PN, Pathological fractures in primary bone sarcomas. Injury. 2008 Apr; [PubMed PMID: 18061185]
Kunze B,Bürkle S,Kluba T, Multifocal osteosarcoma in childhood. La Chirurgia degli organi di movimento. 2009 May; [PubMed PMID: 19711159]
Level 3 (low-level) evidenceZishan US,Pressney I,Khoo M,Saifuddin A, The differentiation between aneurysmal bone cyst and telangiectatic osteosarcoma: a clinical, radiographic and MRI study. Skeletal radiology. 2020 Sep; [PubMed PMID: 32248448]
Zeitoun R,Shokry AM,Ahmed Khaleel S,Mogahed SM, Osteosarcoma subtypes: Magnetic resonance and quantitative diffusion weighted imaging criteria. Journal of the Egyptian National Cancer Institute. 2018 Mar; [PubMed PMID: 29429892]
Angelini A,Mavrogenis AF,Trovarelli G,Ferrari S,Picci P,Ruggieri P, Telangiectatic osteosarcoma: a review of 87 cases. Journal of cancer research and clinical oncology. 2016 Oct [PubMed PMID: 27469493]
Level 3 (low-level) evidenceBacci G,Ferrari S,Ruggieri P,Biagini R,Fabbri N,Campanacci L,Bacchini P,Longhi A,Forni C,Bertoni F, Telangiectatic osteosarcoma of the extremity: neoadjuvant chemotherapy in 24 cases. Acta orthopaedica Scandinavica. 2001 Apr; [PubMed PMID: 11372948]
Level 3 (low-level) evidenceColomina J,Peiro A,Trullols L,Garcia I, Telangiectatic osteosarcoma. Journal of orthopaedic surgery (Hong Kong). 2013 Apr [PubMed PMID: 23629998]
Level 2 (mid-level) evidenceBasaran M,Bavbek ES,Saglam S,Eralp L,Sakar B,Atalar AC,Bilgic B,Ozger H,Onat H, A phase II study of cisplatin, ifosfamide and epirubicin combination chemotherapy in adults with nonmetastatic and extremity osteosarcomas. Oncology. 2007 [PubMed PMID: 18185020]
Kundu ZS. Classification, imaging, biopsy and staging of osteosarcoma. Indian journal of orthopaedics. 2014 May:48(3):238-46. doi: 10.4103/0019-5413.132491. Epub [PubMed PMID: 24932027]
Sandberg AA,Bridge JA, Updates on the cytogenetics and molecular genetics of bone and soft tissue tumors: osteosarcoma and related tumors. Cancer genetics and cytogenetics. 2003 Aug; [PubMed PMID: 12885459]
Khuu H,Moore D,Young S,Jaffe KA,Siegal GP, Examination of tumor and tumor-like conditions of bone. Annals of diagnostic pathology. 1999 Dec [PubMed PMID: 10594288]
Level 3 (low-level) evidence