Introduction
Cardiac computed tomography (CCT) is an innovative, cost-effective, and noninvasive method of objectively evaluating the heart from an anatomical standpoint. When discussing CCTs, one must first appreciate the nomenclature, as multiple terms are used synonymously, including "coronary computed tomography," "cardiac computed tomography," "coronary computed tomography angiography (CCTA)," "cardiac computed tomography angiography," and "multidetector computed tomography." This activity differentiates between non–contrast-enhanced CCT, denoted as "CCT," and contrast-enhanced CCT, also called "cardiac (or coronary) computed tomography angiography," denoted as "CCTA." This activity predominantly focuses on CCT while discussing some major aspects of CCTA. More detailed training on the latter can be found separately.[1]
CCT offers a 3-dimensional approach to cardiac diagnostics, helping clinicians assess the severity of coronary arterial disease (CAD) by determining the extent of atherosclerotic plaques. A 64-slice system aligned with the cardiac cycle provides high-quality spatial and temporal resolution images despite cardiac activity.[2] The significance of CCT lies within its prognostic utility as a fast, noninvasive risk stratification tool. This activity discusses the utility of this approach by elaborating on the coronary artery calcification (CAC) score with an emphasis on different risk stratification tools.
Procedures
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Procedures
Image Acquisition for Coronary Artery Calcification Score
A CAC score is obtained using CCT through 3-mm axial slices focused on the cardiac region. The images are synchronized with the electrocardiogram (ECG) R-R interval, typically captured during late or mid-diastole using prospective ECG gating. No heart rate-lowering medication or intravenous cannulation is needed for CAC scoring. Significant calcification is defined as at least 1 mm of hyperattenuation in the coronary artery wall with either 3 or more pixels or greater than 130 Hounsfield units (HU).[3]
The extent of CAC is quantified using the Agatston score, which is calculated by multiplying the area of CAC by its density. The density factor depends on the calcium deposits' density in HU: 1 for 130 to 199 HU, 2 for 200 to 299 HU, 3 for 300 to 399 HU, and 4 for 400 and above HU. These definitions are used to quantify CAC and coronary plaque burden. The CAC score helps stratify patients; a score of 0 indicates no identifiable disease, 1 to 99 indicates mild disease, 100 to 399 signifies moderate disease, and a score greater than 400 implies severe CAD.
Preparation for Coronary Computed Tomography Angiogram
A 64-slice scanner or better is required. The ideal heart rate is at least 60 beats per minute. Intravenous access with an 18-gauge cannula should be established, preferably in the antecubital vein. Proper placement of ECG leads must be ensured. A contrast injection rate of 5 to 7 mL/s is used. A typical biphasic injection protocol involves 80 mL of contrast at a rate of 5 mL/s, followed by 40 mL of saline at the same rate. Prospective gating is preferred, allowing radiation exposure during a prespecified phase of the cardiac cycle, typically lasting 75% of the cardiac cycle.
Indications
CAC scoring may be used for the following indications:
- To help decide about statin therapy in patients with intermediate risk for atherosclerotic cardiovascular disease (ASCVD) when uncertainty exists regarding the need for statin use.
- To serve as a reliable prognostication tool for risk assessment in asymptomatic patients. CAC scoring outperforms other measures, such as high-sensitivity C-reactive protein, carotid intima-media thickness, and Framingham Risk Score. A CAC score of 0 indicates a low-risk profile, irrespective of the presence or absence of traditional risk factors, such as smoking, dyslipidemia, and hypertension.
- To reclassify the Framingham Risk Score.[4]
The following are the indications of CCT and CCTA, as per the Society of Cardiovascular Computed Tomography (SCCT) 2021 Expert Consensus Document:[5]
- Evaluation of patients with stable CAD with typical or atypical symptoms or angina-equivalent symptoms
- Evaluation of patients with stable CAD and a history of prior coronary revascularization, including percutaneous coronary intervention and coronary artery bypass grafting
- Functional assessment of intermediate-grade coronary artery stenosis using fractional flow reserve
- Assessment of CAD in miscellaneous conditions such as valvular heart disease, nonischemic cardiomyopathies, and congenital anomalies
- Assessment of chronic allograft vasculopathy
- Scar assessment in patients who have contraindications to cardiac magnetic resonance imaging (MRI)
- Risk assessment in asymptomatic patients using CAC scoring
- Risk assessment in special groups, including those with diabetes and a family history of CAD
- Accurate evaluation of periprosthetic windows, allowing optimal viewing to rule out a perivalvular thrombus or pannus [6][7]
- Assessment of intracardiac tumors, thrombi, and pericardial diseases
- Assessment of the great thoracic vessels
Normal and Critical Findings
Normal and critical findings include the following (see Image. Computed Tomography Coronary Angiogram):
- Normal plaque attenuation: calcium deposits of less than 130 HU
- Abnormal plaque attenuation:
- Factor 1: calcium deposits of 130 to 199 HU
- Factor 2: calcium deposits of 200 to 299 HU
- Factor 3: calcium deposits of 300 to 399 HU
- Factor 4: calcium deposits of 400 to 499 HU
The CAC score scale is:
- 0: No evidence of CAD
- 1 to 10: Minimal evidence of CAD
- 11 to 100: Mild evidence of CAD
- 101 to 400: Moderate evidence of CAD
- Greater than 400: Severe evidence of CAD [8]
Interfering Factors
The following factors can interfere with image acquisition and interpretation:
- Arrhythmia or heart rate of more than 70 bpm
- Severe asthma, contraindicating β-blocker intake
- Hypotension or phosphodiesterase inhibitor use, contraindicating nitrate administration
- Agitation or claustrophobia
- Failure to follow breath-holding instructions
- Serum creatinine greater than 1.8 mg/dL (in the context of CCTA)
- Acute decompensated heart failure
Patient Safety and Education
Patients are placed supine on the examination table. Electrodes are positioned on the right and left clavicles, as well as below the costal margin. These electrodes enable ECG gating, which enhances image accuracy by synchronizing imaging with the cardiac cycle. An ideal slower heart rate supports this synchronization, which is why preprocedural β-blocker administration is recommended.
The patient will receive instructions to minimize gross body movements and to hold their breath for a few seconds at a time. Failure to comply with these restrictions may impair the adequate delineation of cardiac structures. Additionally, severe agitation or claustrophobia can prevent a patient from undergoing CCT.
Clinical Significance
Cardiac imaging is a robust yet essential part of cardiovascular medicine. The development of magnetic resonance imaging (MRI), plain chest radiography, echocardiography, and CCT provides clinicians with many tools to evaluate cardiac pathology. Choosing the optimal modality has sometimes proven difficult, as all methods possess specific limitations and indications but share many overlapping characteristics.[9] Specifically, cardiac MRI and CCT or CCTA have developed into modalities of choice when small coronary and cardiac structures must be visualized, likely due to their unrivaled spatial resolution. The clinical uses of CCT are explained below.
Predicting Coronary Artery Disease-Related Events
CAC has been linked to atherosclerosis for decades. CCT provides clinicians with a faster, less cumbersome, more patient-safe method for risk stratification of asymptomatic high-risk patients for CAD. Computer software then evaluates the CAC volume and density, providing data points for prognostic tests, most notably the Agatston method, as discussed above.[10] A CAC score calculated per the Agatston method may be used in conjunction with an already approved stratification tool or alone as a future coronary heart disease (CHD) predictor.
Risk stratification tools that may be used in conjunction with CAC scoring include:
- The Multiethnic Study of Atherosclerosis CAC (MESA CAC) has demonstrated the efficacy of CAC scores by incorporating individual CAC values into the study's demographic database. Including the CAC score in the cardiovascular event prediction model developed by MESA established this parameter as a dominant predictor of CHD and all-cause ASCVD outcomes.[11]
- The CAC Data and Reporting System (CAC-DRS) has been shown to provide better prognostic stratification regarding CHD, cardiovascular disease, and all-cause mortality than the Agatston reporting system alone. This risk stratification considers the CAC score as well as the number of coronary vessels involved.[12]
- Using the CAC score as a reclassification tool in the context of the Framingham Risk Score has shown benefits for intermediate-risk patients. Roughly 60% of atherosclerotic coronary events occur in low-to-intermediate-risk patients, according to the Framingham risk assessment. The addition of a patient's CAC score substantially increases the accuracy of this stratification.[13]
CAC risk stratification provides clinicians with data to support starting an asymptomatic patient on aspirin or statin across all 3 discussed methods.
CAC scoring may also be used as an independent predictor of future CAD-related events. According to the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) consensus report from 2007, the following relative risk (RR) ratios for CAD-related events were calculated based on isolated CAC scores in asymptomatic patients:
- CAC scores of 100 to 400 have an RR of 4.3
- CAC scores of 401 to 999 have an RR of 7.2
- CAC scores greater than 1000 have an RR of 10.8 [14]
Predicting Coronary Artery Disease Degree of Stenosis
A recent study demonstrated the CAC score to accurately predict the degree of coronary arterial stenosis via histological evaluation of postmortem coronary arteries. This study showed CAC scoring to be an effective tool in determining a patient's degree of coronary arterial stenosis.[15]
Media
(Click Image to Enlarge)
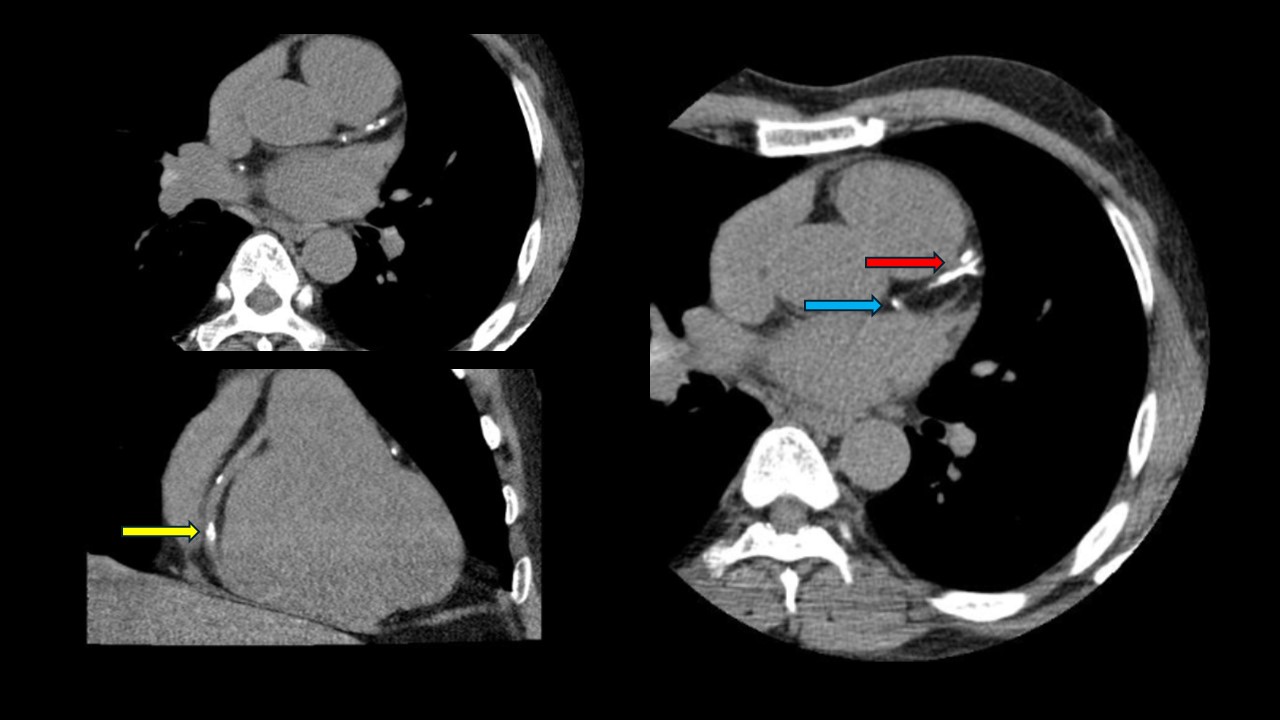
Computed Tomography Coronary Angiogram. This computed tomography coronary angiogram of a patient with an Agatston score of 828 reveals a heavily calcified left anterior descending coronary artery (red arrow). The right coronary artery (yellow arrow) and ostial left circumflex artery (blue arrow) also have calcified lesions.
Contributed by P Shams, MBBS, FCPS
References
Ramjattan NA, Lala V, Kousa O, Shams P, Makaryus AN. Coronary CT Angiography. StatPearls. 2024 Jan:(): [PubMed PMID: 29262000]
Prat-Gonzalez S, Sanz J, Garcia MJ. Cardiac CT: indications and limitations. Journal of nuclear medicine technology. 2008 Mar:36(1):18-24. doi: 10.2967/jnmt.107.042424. Epub 2008 Feb 20 [PubMed PMID: 18287198]
Neves PO, Andrade J, Monção H. Coronary artery calcium score: current status. Radiologia brasileira. 2017 May-Jun:50(3):182-189. doi: 10.1590/0100-3984.2015.0235. Epub [PubMed PMID: 28670030]
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC Jr, Sperling L, Virani SS, Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Jun 18:139(25):e1082-e1143. doi: 10.1161/CIR.0000000000000625. Epub 2018 Nov 10 [PubMed PMID: 30586774]
Level 1 (high-level) evidenceNarula J, Chandrashekhar Y, Ahmadi A, Abbara S, Berman DS, Blankstein R, Leipsic J, Newby D, Nicol ED, Nieman K, Shaw L, Villines TC, Williams M, Hecht HS. SCCT 2021 Expert Consensus Document on Coronary Computed Tomographic Angiography: A Report of the Society of Cardiovascular Computed Tomography. Journal of cardiovascular computed tomography. 2021 May-Jun:15(3):192-217. doi: 10.1016/j.jcct.2020.11.001. Epub 2020 Nov 20 [PubMed PMID: 33303384]
Level 3 (low-level) evidenceSenapati A, Faza NN, Mahmarian J, Chang SM. Cardiac Computed Tomography for Structural Heart Disease Assessment and Therapeutic Planning: Focus on Prosthetic Valve Dysfunction. Methodist DeBakey cardiovascular journal. 2020 Apr-Jun:16(2):86-96. doi: 10.14797/mdcj-16-2-86. Epub [PubMed PMID: 32670468]
Gündüz S, Özkan M, Kalçik M, Gürsoy OM, Astarcioğlu MA, Karakoyun S, Aykan AÇ, Biteker M, Gökdeniz T, Kaya H, Yesin M, Duran NE, Sevinç D, Güneysu T. Sixty-Four-Section Cardiac Computed Tomography in Mechanical Prosthetic Heart Valve Dysfunction: Thrombus or Pannus. Circulation. Cardiovascular imaging. 2015 Dec:8(12):. pii: e003246. doi: 10.1161/CIRCIMAGING.115.003246. Epub [PubMed PMID: 26659372]
Mlynarska A, Mlynarski R, Sosnowski M. Usefulness of the Coronary Artery Calcium Score in Predicting Subsequent Coronary Interventions-A Ten-Year Single-Center Perspective. International journal of environmental research and public health. 2019 Jun 16:16(12):. doi: 10.3390/ijerph16122132. Epub 2019 Jun 16 [PubMed PMID: 31208148]
Level 3 (low-level) evidenceASCI Practice Guideline Working Group, Beck KS, Kim JA, Choe YH, Hian SK, Hoe J, Hong YJ, Kim SM, Kim TH, Kim YJ, Kim YH, Kuribayashi S, Lee J, Leong L, Lim TH, Lu B, Park JH, Sakuma H, Yang DH, Yaw TS, Wan YL, Zhang Z, Zhao S, Yong HS. 2017 Multimodality Appropriate Use Criteria for Noninvasive Cardiac Imaging: Expert Consensus of the Asian Society of Cardiovascular Imaging. Korean journal of radiology. 2017 Nov-Dec:18(6):871-880. doi: 10.3348/kjr.2017.18.6.871. Epub 2017 Sep 21 [PubMed PMID: 29089819]
Level 3 (low-level) evidenceChua A, Blankstein R, Ko B. Coronary artery calcium in primary prevention. Australian journal of general practice. 2020 Aug:49(8):464-469. doi: 10.31128/AJGP-03-20-5277. Epub [PubMed PMID: 32738864]
Greenland P, Blaha MJ, Budoff MJ, Erbel R, Watson KE. Coronary Calcium Score and Cardiovascular Risk. Journal of the American College of Cardiology. 2018 Jul 24:72(4):434-447. doi: 10.1016/j.jacc.2018.05.027. Epub [PubMed PMID: 30025580]
Dzaye O, Dudum R, Mirbolouk M, Orimoloye OA, Osei AD, Dardari ZA, Berman DS, Miedema MD, Shaw L, Rozanski A, Holdhoff M, Nasir K, Rumberger JA, Budoff MJ, Al-Mallah MH, Blankstein R, Blaha MJ. Validation of the Coronary Artery Calcium Data and Reporting System (CAC-DRS): Dual importance of CAC score and CAC distribution from the Coronary Artery Calcium (CAC) consortium. Journal of cardiovascular computed tomography. 2020 Jan-Feb:14(1):12-17. doi: 10.1016/j.jcct.2019.03.011. Epub 2019 Mar 28 [PubMed PMID: 30952612]
Level 1 (high-level) evidenceLehmann N, Erbel R, Mahabadi AA, Rauwolf M, Möhlenkamp S, Moebus S, Kälsch H, Budde T, Schmermund A, Stang A, Führer-Sakel D, Weimar C, Roggenbuck U, Dragano N, Jöckel KH, Heinz Nixdorf Recall Study Investigators. Value of Progression of Coronary Artery Calcification for Risk Prediction of Coronary and Cardiovascular Events: Result of the HNR Study (Heinz Nixdorf Recall). Circulation. 2018 Feb 13:137(7):665-679. doi: 10.1161/CIRCULATIONAHA.116.027034. Epub 2017 Nov 15 [PubMed PMID: 29142010]
Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, Lauer MS, Post WS, Raggi P, Redberg RF, Rodgers GP, Shaw LJ, Taylor AJ, Weintraub WS, American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography), Society of Atherosclerosis Imaging and Prevention, Society of Cardiovascular Computed Tomography. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography. Journal of the American College of Cardiology. 2007 Jan 23:49(3):378-402 [PubMed PMID: 17239724]
Level 3 (low-level) evidenceKaur M, Rahimi R, Razali F, Mohd Noor N, Omar E, Abdul Manaf Z, Mahmood MS, Abdullah N, Nawawi H. Association of coronary artery calcium score with calcification and degree of stenosis: An autopsy study. The Malaysian journal of pathology. 2019 Aug:41(2):177-183 [PubMed PMID: 31427553]