Introduction
Ocular cicatricial pemphigoid (OCP) is a form of mucous membrane pemphigoid (MMP) that features a chronic, relapsing-remitting bilateral conjunctivitis. Ultimately, patients affected by this autoimmune disease will experience conjunctival cicatrization or scarring, and if unresponsive to treatment or left untreated will develop corneal opacification and permanent vision loss.[1] MMP can also affect the skin as well as mucous membranes of the mouth, nose, esophagus, genitals, and anus – causing erosions, blisters, and strictures. Ocular cicatricial pemphigoid represents about 60% to 70% of those affected by MMP. [2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The cause of ocular cicatricial pemphigoid is an autoimmune type II hypersensitivity response.[1] This autoimmune response occurs when a patient has a genetic predisposition and is exposed to an environmental trigger. Antibodies bind to surface antigens on the basement membrane of the conjunctiva. This causes recruitment and activation of complement proteins and inflammatory cytokines and leads to inflammation and scarring. There is evidence of an association to patients with HLA-DR4 and HLA-DQ7.[3]
Epidemiology
Ocular cicatricial pemphigoid predominantly affects females (2:1 over males), and the age of onset is around 60 years of age or older. There is no racial predilection. Ocular cicatricial pemphigoid is considered a rare disease, and incidence is estimated to be about 1 per 10,000 to 50,000. [1]
Histopathology
Conjunctival biopsy with direct immunofluorescence (DIF) is the most reliable method and the gold standard to confirm the ocular cicatricial pemphigoid diagnosis. About 20% to 40% of patients may have clinical signs of ocular cicatricial pemphigoid but may, in fact, have a negative biopsy result.[4],[5],[6] This does not rule out the diagnosis of ocular cicatricial pemphigoid even with a broad and complex differential diagnosis. These patients most likely only have ocular disease, as a positive result is more common in those with ocular, skin, and oral disease. Negative results may be due to the biopsy technique, concurrent quiescence, or even disease burnout.[5] When positive, the results show a linear deposition of IgG, IgA, and sometimes IgM and complement 3 proteins in the epithelial basement membrane zone.[5] Autoantibodies against antigen sites within the basement membrane are rarely detected, even in those patients with a positive biopsy.[5]
A histological analysis will often show positive hematoxylin and eosin (H&E) inflammatory cell staining; periodic acid–Schiff (PAS) stain, showing decreased goblet cells in the affected tissue; and Giemsa stain, showing an increased mast cell population.[5] Histological studies also can help differentiate from neoplasia if direct immunofluorescence is inconclusive.
History and Physical
Patients with ocular cicatricial pemphigoid experience a bilateral, chronic conjunctivitis that has remissions and exacerbations. Ocular cicatricial pemphigoid is often misdiagnosed and delayed due to the insidious onset and nonspecific signs and symptoms in the early stages of the disease. In the beginning, patients experience ocular redness, tearing, burning, light sensitivity, and foreign body sensation; these presentations are similar to dry eye syndrome and many other anterior segment inflammatory conditions. There is minimal to no discharge present, which helps determine infectious versus non-infection causes. As the disease progresses, the signs become pathognomic for ocular cicatricial pemphigoid, most notably with the development of a symblepharon, which is an adhesion between the palpebral and bulbar conjunctiva.
Early on in the disease, the conjunctiva exhibits the following signs: diffuse hyperemia, papillary reaction, dry eye syndrome, and keratoconjunctivitis sicca due to the destruction of goblet cells. Intermediate stages of the disease are notable for subconjunctival fibrosis and shortening of the inferior fornix. This is most often found when patients are diagnosed. Later on, as the disease progresses, the symblephara develop and there is flattening of the plica and keratinization of the caruncle.
Ocular cicatricial pemphigoid affects the cornea, and the beginning stages include punctate epithelial erosions, exposure keratitis, epithelial defects, peripheral infiltrates, ulcers, and vascularization. Worsening of the condition results in limbal stem cell failure leading to keratinization and conjunctivalization. Corneal opacification is possible late in the disease.
The eyelids are also affected throughout the disease process, with the first signs including blepharitis, trichiasis, and entropion due to subepithelial scarring and keratinization of the eyelid margin. Patients with end-stage ocular cicatricial pemphigoid may develop ankyloblepharon, which refers to the fusion of the upper and lower eyelids. [4]
Evaluation
Several evaluation/grading systems can detect progression and monitor ocular cicatricial pemphigoid. The Foster staging system is based on clinical signs whereas the Mondino and Brown system is based on an inferior fornix depth.
Foster System
- Stage 1 - includes subconjunctival scarring and fibrosis
- Stage 2 - includes fornix shortening
- Stage 3 - occurs when a symblepharon form
- Stage 4 - the formation of ankyloblepharon and keratinization of the ocular surface
Mondino and Brown System
Treatment / Management
The medical management strategy for ocular cicatricial pemphigoid is to control inflammation and halt the progression of fibrosis. Treatments include topical/local therapies, systemic medications, minor procedures, and surgical intervention when necessary.
Topical/Local
Treating dry eye is essential for improving ocular comfort, optimizing visual acuity, and preventing corneal epithelial breakdown. First and foremost, patients should have a regimen of frequent instillation of preservative-free artificial tears and lubricating ointments. Common regimens, depending on the stage of the disease, include artificial tears every 2 hours and ointment 2 to 4 times per day and at bedtime. Topical steroids, cyclosporine-A, and tacrolimus can also be used to reduce ocular surface inflammation and treat signs and symptoms of keratoconjunctivitis sicca (KCS) but do not slow the progression of the disease. Steroids must be used with caution due to the side effects of ocular hypertension and cataract formation. Topical anti-ocular hypertensive drops may worsen the clinical signs and symptoms of ocular cicatricial pemphigoid due to ocular surface toxicity. Cataract surgery is high risk in patients with ocular cicatricial pemphigoid due to the risk of postoperative bacterial infections and abnormal healing at incision sites.
Clinicians should consider autologous serum drops in patients with progressive or severe KCS. Autologous serum drops are derived from the patient's own blood serum and most often diluted to 20% with sterile saline. Serum drops can vary in strength and some patients may require 50% or up to 100% serum. Serum contains growth factors, albumin, and other compounds that help promote epithelial healing. The clinician should also consider silicone punctal plugs to retain a higher volume of tears on the ocular surface if the effects of the disease have not already caused physiological punctal occlusion. It is common that subepithelial scarring of the conjunctiva and eyelids cause tissue shrinkage and physiological punctal occlusion.
Scleral lenses are large diameter rigid gas permeable contact lenses that are inserted with preservative-free saline to provide a moisture reservoir for the ocular surface and help with epithelial healing. The lens also acts as a bandage to protect from desiccation and mechanical irritation from keratinized eyelids and trichiasis. Another benefit of scleral lenses is the correction of irregular astigmatism that may be caused by corneal damage secondary to the disease process. Scleral contact lenses may also be used for non-healing persistent corneal epithelial defects (PCED). Due to symblepharon formation and abnormal architecture of the conjunctiva, it may be difficult to fit patients with this lens type due to its size. While these lenses seem to provide many benefits to patients affected by ocular cicatricial pemphigoid, contact lens wear has the inherent risk of hypoxia, vascularization, and microbial keratitis. These patients need frequent follow-up care.
Severe KCS, exposure keratitis, and PCED may also benefit from the application of a sutureless amniotic membrane. Similar to serum tears, amniotic membranes provide anti-inflammatory cytokines and growth factors to promote epithelial healing.
In addition to addressing the disease effects on the conjunctiva and cornea, the eyelids must be aggressively treated for blepharitis. Untreated blepharitis may contribute to exposure keratitis, trichiasis, and, most importantly, microbial keratitis. Patients with severe blepharitis commonly have thickened, white, toothpaste-like meibomian gland secretions which contribute to worsening dry eye and ocular surface damage. These patients should be educated on the use of eyelid hygiene and the use of warm compresses to reduce eyelid inflammation and promote healthy meibomian gland secretions. Clinicians often prescribe antibiotic ointments and oral doxycycline for its anti-inflammatory benefits. The anti-inflammatory action of doxycycline is also useful in the treatment of recurrent corneal erosions and persistent corneal epithelial defects. The dosage of doxycycline varies among clinicians, but a common regimen is to prescribe 50 to 100 mg twice per day for one month, followed by 20 to 50 mg daily.
Systemic
While topical and local therapies are important for controlling symptoms, lubricating the ocular surface, and reducing local inflammation, only systemic treatment will stop the progression of ocular cicatricial pemphigoid. The consensus is to initiate systemic treatment at Foster stage 2 with evidence of fornix shortening, although many times there is a delay in diagnosis, and ocular cicatricial pemphigoid is not formally diagnosed until the patient has reached stage 3 with the formation of a symblepharon.
Dapsone is the first-line treatment for mild to moderate disease. Dapsone is a sulfonamide antibiotic that also has anti-inflammatory and immunomodulatory action. It must be avoided in patients with G6PD deficiency due to the risk of hemolytic anemia. Dapsone is initially dosed at 50 mg/day and slowly increased by 25 mg every 4 to 7 days until the effective dose is achieved, which is usually 100 to 200 mg/day. If the patient has a contraindication to Dapsone, treatment can be initiated with sulfasalazine (1000 to 4000 mg daily) or sulfapyridine (500 to 1000 mg daily); but similar to Dapsone, there is a contraindication to these other sulfa-based medications in patients with G6PD deficiency.
Moderate to severe disease or lack of response to Dapsone or other first-line alternatives after 2 to 3 months will likely require a systemic corticosteroid pulse over 6 to 8 weeks with concurrent immunosuppressant therapy with azathioprine (1 to 2.5 mg/kg daily), mycophenolate mofetil (500 to 1000 mg twice daily), methotrexate (10 to 15 mg weekly) or cyclosporine. Cyclophosphamide should be considered in severe and rapidly progressing disease states, especially when previous therapies have been unsuccessful. Cyclophosphamide (1 to 2 mg/kg daily) is reserved for advanced and recalcitrant disease due to its potentially life-threatening adverse effects, such as pancytopenia and liver toxicity.
Biologics such as etanercept (25 mg subcutaneous injection) or rituximab (375 mg weekly for 8 weeks, then monthly) and intravenous immunoglobulin therapy (2 to 3 g/kg/cycle for 3 consecutive days every 2 to 4 weeks) are reserved for patients who have a poor response to conventional therapy with systemic steroids and immunosuppressants or if there are contraindications and/or risk of severe adverse effects with the abovementioned treatments.
Surgical Intervention
Minor procedures and surgical intervention as adjunctive therapy for ocular cicatricial pemphigoid include eyelash epilation, entropion repair, lateral tarsorrhaphy, and botox injection-induced ptosis. In severe stages of the disease, patients may need limbal stem cell transfer for corneal re-epithelialization and mucous membrane autografts or amniotic membrane transplants for fornix reconstruction. Patients should be in a quiescent phase of the condition before incisional surgery is considered due to a possible uncontrolled post-operative inflammation and scarring. Corneal transplants are often unsuccessful due to graft vascularization and failure. A keratoprosthesis is an artificial cornea that may be required in end-stage disease, although the prognosis is poor for long-term survival of the graft.
Differential Diagnosis
The differential diagnosis includes all conditions that cause an asymmetric bilateral chronic conjunctivitis with conjunctival cicatrization. These include Stevens-Johnson syndrome, toxic epidermal necrolysis, trachoma, graft-versus-host disease, dry eye syndrome, history of adenoviral conjunctivitis, chemical burn, medicamentosa (from topical glaucoma medications and anti-viral medications for herpetic eye disease), atopic keratoconjunctivitis, radiation exposure, systemic lupus erythematosus, and Sjogren syndrome. A distinguishing clinical feature of OCP is a progressive symblepharon.[5] Symblephara from the above etiologies may form and then remain stable. However, a few conditions in which progressive cicatrization occur include neoplasia, lichen planus, and paraneoplastic pemphigus.[5][8]
Prognosis
In general, of those with MMP, those with ocular involvement have a worse prognosis than those affected with skin and/or oral mucosa involvement alone. Systemic therapy can stop the progression of ocular cicatricial pemphigoid in about 90% of patients, and the rate of recurrence is about 20% to 30%, but this is variable.[5] An interesting feature of ocular cicatricial pemphigoid is the presence of “white inflammation” in about 40% of patients. This refers to the progression of subepithelial fibrosis and cicatrization in the absence of clinical signs. The patient is asymptomatic, and on examination, the conjunctiva is clear and quiet but there is evidence of disease progression and histological sampling of conjunctival tissue will show inflammatory cells present.[9] This can lead to difficulties in management.
Several studies show that between 25% to 30% of patients progress to blindness due to the pathophysiology leading up to and including corneal opacification.[5] Ocular cicatricial pemphigoid is a lifelong disease that requires follow up care, even when in remission.
Enhancing Healthcare Team Outcomes
The management of ocular pemphigoid is primarily by the eye surgeon but the follow up is with the primary care provider, dermatologist or nurse practitioner. The medical management strategy for ocular cicatricial pemphigoid is to control inflammation and halt the progression of fibrosis. Treatments include topical/local therapies, systemic medications, minor procedures, and surgical intervention when necessary.
In general, of those with MMP, those with ocular involvement have a worse prognosis than those affected with skin and/or oral mucosa involvement alone. Systemic therapy can stop the progression of ocular cicatricial pemphigoid in about 90% of patients, and the rate of recurrence is about 20% to 30%, but this is variable.[5] Several studies show that between 25% to 30% of patients progress to blindness due to the pathophysiology leading up to and including corneal opacification.[5] Ocular cicatricial pemphigoid is a lifelong disease that requires follow up care, even when in remission.
Media
(Click Image to Enlarge)
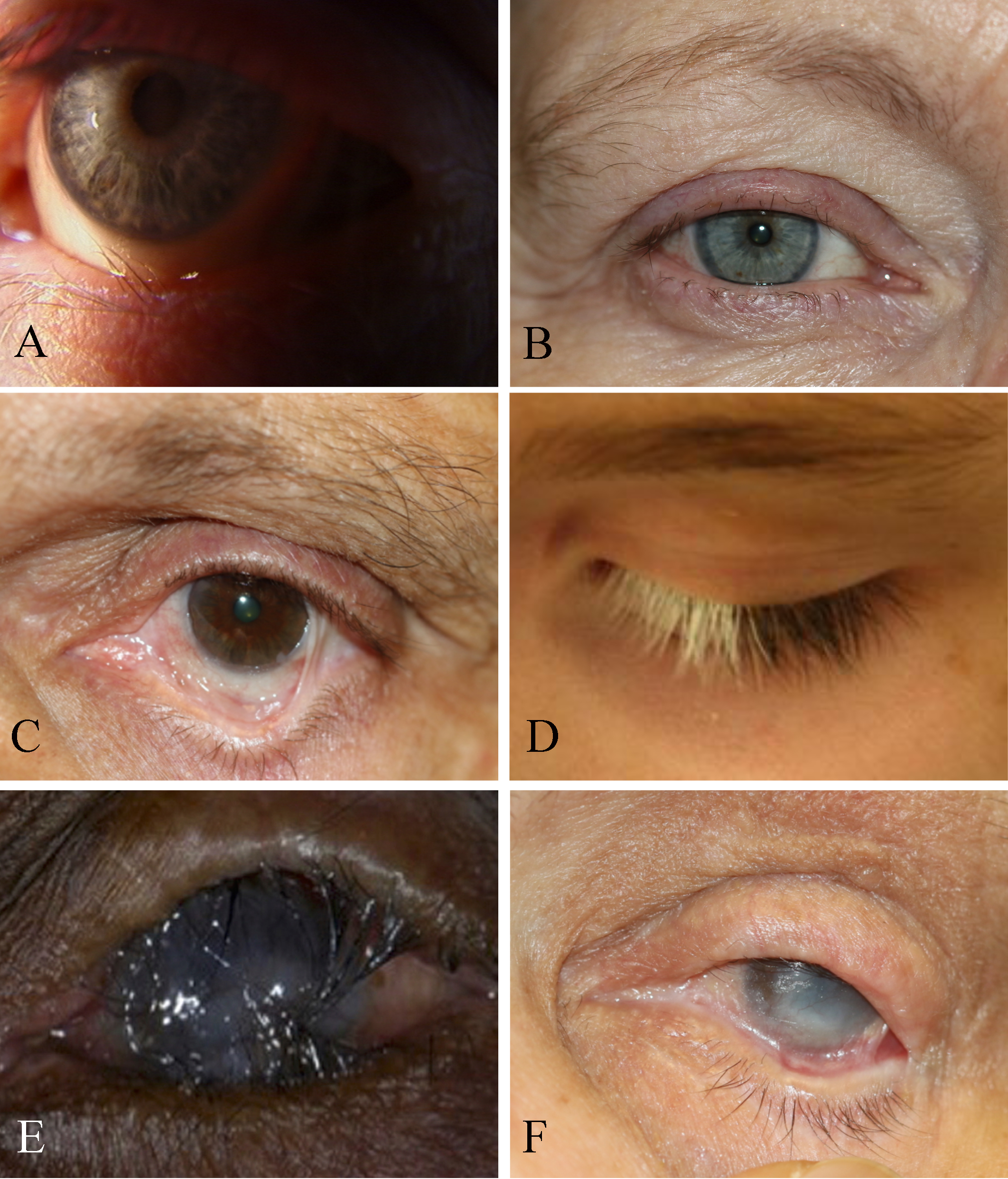
Eye Disorders and Trachoma-Associated Symptoms, Trichiasis. The eyelid itself is not turning in, but the lashes are pointing inward (A). Madarosis. Short stubby lashes of different sizes indicate trichotillomania (B). Symblepharon with secondary trichiasis, fornix shortening, and cicatricial entropion (C). Poliosis (D). Trachoma with corneal opacification (E). Pemphigoid disease with cicatricial entropion, trichiasis, ankyloblepharon, corneal scarring, and dry eyes (F).
Contributed by BCK Patel, MD, FRCS
(Click Image to Enlarge)

Causes of Epiphora. The conditions that can cause epiphora include herpes zoster with keratitis (A), lacrimal mucocele (B), corneal calcific keratopathy (C), floppy eyelid syndrome (D), kissing puncta syndrome (E), and pemphigoid disease with trichiasis and obliteration of puncta (F).
Contributed by BCK Patel, MD, FRCS
(Click Image to Enlarge)

A. Punctal stenosis caused by a chemical burn with conjunctival and lid margin muco-cutaneous junction scarring B. Complete obliteration of the puncta secondary to cicatrization caused by Stevens Johnson syndrome C. Punctal occlusion in the presence of mucous membrane pemphigoid disease Contributed by Professor Bhupendra C. K. Patel MD, FRCS
References
Foster CS. Cicatricial pemphigoid. Transactions of the American Ophthalmological Society. 1986:84():527-663 [PubMed PMID: 3296406]
Chan LS,Ahmed AR,Anhalt GJ,Bernauer W,Cooper KD,Elder MJ,Fine JD,Foster CS,Ghohestani R,Hashimoto T,Hoang-Xuan T,Kirtschig G,Korman NJ,Lightman S,Lozada-Nur F,Marinkovich MP,Mondino BJ,Prost-Squarcioni C,Rogers RS 3rd,Setterfield JF,West DP,Wojnarowska F,Woodley DT,Yancey KB,Zillikens D,Zone JJ, The first international consensus on mucous membrane pemphigoid: definition, diagnostic criteria, pathogenic factors, medical treatment, and prognostic indicators. Archives of dermatology. 2002 Mar [PubMed PMID: 11902988]
Level 3 (low-level) evidenceAhmed AR, Foster S, Zaltas M, Notani G, Awdeh Z, Alper CA, Yunis EJ. Association of DQw7 (DQB1*0301) with ocular cicatricial pemphigoid. Proceedings of the National Academy of Sciences of the United States of America. 1991 Dec 15:88(24):11579-82 [PubMed PMID: 1763074]
Saw VP,Dart JK, Ocular mucous membrane pemphigoid: diagnosis and management strategies. The ocular surface. 2008 Jul [PubMed PMID: 18781259]
Labowsky MT, Stinnett SS, Liss J, Daluvoy M, Hall RP 3rd, Shieh C. Clinical Implications of Direct Immunofluorescence Findings in Patients With Ocular Mucous Membrane Pemphigoid. American journal of ophthalmology. 2017 Nov:183():48-55. doi: 10.1016/j.ajo.2017.08.009. Epub 2017 Aug 30 [PubMed PMID: 28860044]
Hingorani M, Lightman S. Ocular cicatricial pemphigoid. Current opinion in allergy and clinical immunology. 2006 Oct:6(5):373-8 [PubMed PMID: 16954792]
Level 1 (high-level) evidenceMondino BJ, Brown SI. Ocular cicatricial pemphigoid. Ophthalmology. 1981 Feb:88(2):95-100 [PubMed PMID: 7015218]
De Rojas MV, Dart JK, Saw VP. The natural history of Stevens Johnson syndrome: patterns of chronic ocular disease and the role of systemic immunosuppressive therapy. The British journal of ophthalmology. 2007 Aug:91(8):1048-53 [PubMed PMID: 17314145]
Level 2 (mid-level) evidenceSaw VP,Schmidt E,Offiah I,Galatowicz G,Zillikens D,Dart JK,Calder VL,Daniels JT, Profibrotic phenotype of conjunctival fibroblasts from mucous membrane pemphigoid. The American journal of pathology. 2011 Jan [PubMed PMID: 21224056]