Introduction
Blepharoconjunctivitis is an ophthalmic disease that combines the features of blepharitis and conjunctivitis. It is characterized by inflammation of the eyelid margin (blepharitis) and the surrounding conjunctiva (conjunctivitis). It is closely related to blepharitis and can be considered to be a mature form of blepharitis. If blepharitis is left unmanaged in the initial stages, the inflammation progresses to affect the nearby conjunctiva resulting in blepharoconjunctivitis. Several classification systems have been proposed to describe the condition based on etiology, clinical features, anatomy, and standardized photo grading scales.[1][2][3][4]
The majority of cases in the United States are classified using the American Academy of Ophthalmology preferred practice patterns, which separate cases into anterior or posterior based on the anatomy affected.[5] Treatment is identical to blepharitis and focuses on symptom relief. Management is composed of lid hygiene and reduction of exposure to possible environmental triggers. Topical steroids, antibiotics, and antiseptics can also be used to manage the condition.[6][7]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
It is difficult to separate the cause of blepharoconjunctivitis from the cause of blepharitis. This is due to the proximity of ocular structures and the often rapid involvement of the conjunctiva in blepharitis.[8] Blepharocojunctivitis can be caused by a variety of issues and is often multifactorial. In the acute form, it is useful to categorize the causes by clinical features. If the onset is acute with ulcerating features, this points to an infective process, with the most common organism being Staphylococcus. However, if the onset is acute with no ulceration, this points to an allergic process. It is important to note, however, that the lack of ulcers does not exclude infection as this sign is poorly specific.
If the onset is chronic, one can categorize the causes via the anatomy involved – posterior versus angular versus anterior. Meibomian gland dysfunction is often the culprit in blepharoconjunctivitis involving the posterior aspect of the eyelid.[9] If there is involvement of the canthal angle, this is angular blepharoconjunctivitis and can be caused by an infection such as Moraxella or, in rare cases, deficiency of vitamin B6.[8][10] If the anterior eyelid is involved, this can point to an infection such as Staphylococcus or a seborrheic process.[11] There is an association between this and acne rosacea.[12] Other causes of blepharoconjunctivitis include parasitic infections such as Demodex, pubic lice, and drugs such as dupilumab.[13][14][15]
Epidemiology
Due to the similarity between blepharoconjunctivitis and blepharitis, it is difficult to separate epidemiological data for the two. Additionally, there is a scarcity of reliable data on the prevalence of blepharitis in the general population. This is largely due to the majority of studies focusing on the population of eye clinics. A US study of ophthalmologists and optometrists found 37% to 47% of patients in their eye clinics exhibited signs of blepharitis.[16] A study of 90 patients at one center found the mean age of their patients to be 50 years old.[17] In a separate study, infective blepharitis (staphylococcal) was more common in females with the age of onset being 42. In seborrheic blepharitis, the mean age was approximately 50, and there was no significant between sexes.[2][18]
Pathophysiology
The pathophysiology of blepharoconjunctivitis is poorly described in the literature and is likely to be multifactorial. As we have discussed, there are many contributing factors, including inflammatory skin conditions, mild longstanding bacterial infections, and parasites.
History and Physical
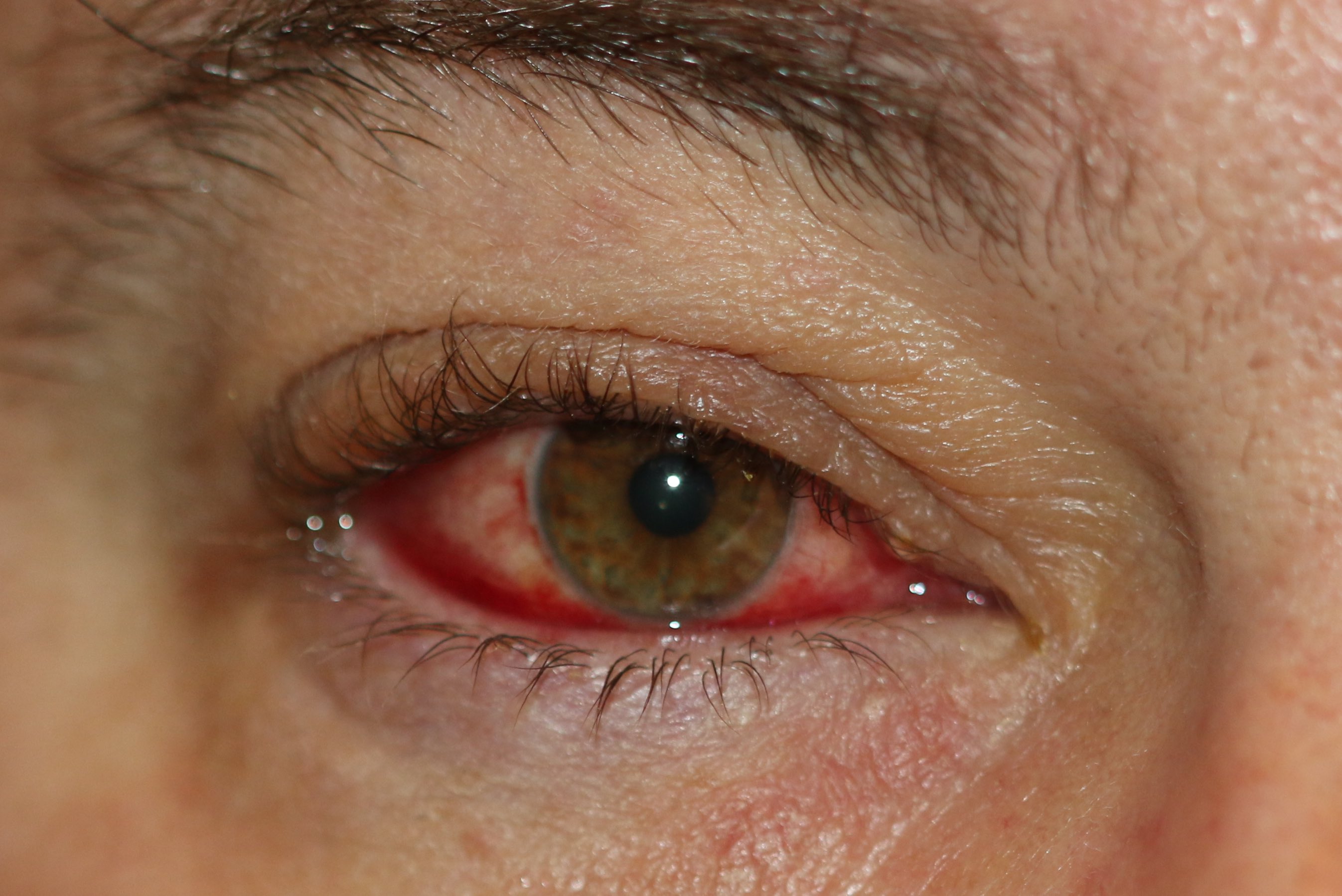
Sufferers of blepharoconjunctivitis describe a typical blepharitic picture of eye irritation with foreign body sensation and crusting of the eyelids along with reports of red eyes. Symptoms are generally worse in the morning, and patients may report eyelids being stuck shut upon waking. Usually, both eyes are affected, and symptoms can fluctuate.
With regards to signs on examination, the patient will likely exhibit a rapid tear film break up time (<10 seconds) when visualized with fluorescein under blue light, and there may be corneal erosions or ulceration. Inspection of the sclera and conjunctivae will show varying degrees of conjunctival injection.
If the underlying blepharitis is anterior in origin, the eyelid margin will appear edematous. The eyelid margin will be erythematous, and telangiectasia may be seen. There may be crusting on the eyelid margin with the formation of collarettes at the base of the lashes. In chronic cases, there may be changes in the eyelashes themselves, such as poliosis (depigmentation), trichiasis (change in direction), or madarosis (reduction in the number of eyelashes). The eyelid may be distorted, and ectropion or entropion may be visible.
If the underlying blepharitis is posterior in origin, the Meibomian glands will be dilated, and the aperture clogged with a visible 'head' or 'cap' of thick oil. On slit-lamp examination, these 'heads' appear like a string of pearls lying on the eyelid margin. The eyelid immediately surrounding the glands may be scarred or visibly inflamed.
Evaluation
Blepharoconjunctivitis is a clinical diagnosis based upon the history, signs, and symptoms of the patient. Investigations such as tear film break up time can be useful but is not necessary. In cases that are refractory to treatment, one should consider lid biopsy to rule out a malignancy. Examination with fluorescein drops and blue light can be useful to detect corneal erosions or ulcers, which are associated with chronic poorly controlled blepharoconjunctivitis.
Treatment / Management
The mainstay treatment of blepharoconjunctivitis is meticulous lid hygiene. Using a warm eye compress for 5 to 10 minutes helps to soften the oil within the Meibomian glands. Massaging of the lid margin can help express the oil, and an eyelash scrub with a mild shampoo removes debris. Lid hygiene should be encouraged even after an acute exacerbation has subsided due to the chronic nature of the condition. Artificial tears can aid dry eye symptoms, and topical steroids are useful in the acute inflammatory stages of an exacerbation. Topical antibiotics should be offered if lid hygiene alone is insufficient, and this proves to be especially effective if the cause is bacterial such as in a staphylococcal infection.[19] Cases of seborrheic blepharitis often coincide with seborrheic dermatitis. These patients will benefit from concurrent treatment of the underlying dermatitis. In patients suffering from posterior blepharitis, oral azithromycin can prove useful.[20](B2)
Supplementation of omega-3 and omega-6 fatty acids to alleviate dry eye symptoms is a controversial topic. A recent Cochrane systematic review suggested that Omega-3 supplementation may be beneficial but states the quality of evidence is poor.[21](A1)
Differential Diagnosis
In patients who are refractory to treatment, it is important to rule out malignancy, especially if there are lash changes. Malignancy tends to affect the lower lid, and there should be a high index of suspicion if the symptoms are unilateral. Patients with dry eye syndrome may present with a similar 'gritty' foreign body sensation in their eyes. However, they will usually lack the inflammation and crusting on the lid margins.
Prognosis
Prognosis is generally good, and the majority of patients achieve symptomatic relief. Due to the chronic nature of the condition, ongoing meticulous lid hygiene is necessary as maintenance therapy to prevent acute exacerbations.
Complications
Complications can occur in long-term chronic cases. Involvement of the cornea, such as ulceration, scarring, or vascularization, is possible. Additionally, the lid margin can be distorted, leading to trichiasis, ectropion/entropion, or madarosis. Ulceration or perforation requires urgent aggressive therapy to prevent further permanent vision impairment.
Deterrence and Patient Education
Patients need to be educated that this is a chronic condition that requires ongoing maintenance therapy (lid hygiene in most cases) to prevent acute exacerbations. Patients should be educated on the symptoms of complications and advised to seek urgent medical advice if there is any deterioration in vision or new eye pain.
Enhancing Healthcare Team Outcomes
Health professionals such as optometrists, nurses, pharmacists, or primary care clinicians who may be the first port of call for mild ailments should be aware of the importance of lid hygiene in blepharoconjunctivitis and the practicalities surrounding this. When symptoms persist despite proper treatment, an ophthalmologist should be consulted. Excellent communication within the interprofessional team is vital to improve patient outcomes. Disseminating accurate advice is central to preventing exacerbation of blepharoconjunctivitis, particularly in the initial stages. Promoting prevention education can help to reduce the need for ophthalmic consultation and empower patients to engage with their own care.
As discussed, there is a subset of patients who may benefit from dermatology input. These individuals should be identified early and discussed with dermatologist colleagues to ensure the patient is receiving optimal care.
Media
(Click Image to Enlarge)
References
THYGESON P. The etiology and treatment of blepharitis; a study in military personnel. Military surgeon. 1946 Mar:98():191-203 [PubMed PMID: 21017790]
McCulley JP, Dougherty JM, Deneau DG. Classification of chronic blepharitis. Ophthalmology. 1982 Oct:89(10):1173-80 [PubMed PMID: 6218459]
Huber-Spitzy V, Baumgartner I, Böhler-Sommeregger K, Grabner G. Blepharitis--a diagnostic and therapeutic challenge. A report on 407 consecutive cases. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 1991:229(3):224-7 [PubMed PMID: 1831177]
Level 3 (low-level) evidenceMathers WD, Choi D. Cluster analysis of patients with ocular surface disease, blepharitis, and dry eye. Archives of ophthalmology (Chicago, Ill. : 1960). 2004 Nov:122(11):1700-4 [PubMed PMID: 15534133]
Amescua G, Akpek EK, Farid M, Garcia-Ferrer FJ, Lin A, Rhee MK, Varu DM, Musch DC, Dunn SP, Mah FS, American Academy of Ophthalmology Preferred Practice Pattern Cornea and External Disease Panel. Blepharitis Preferred Practice Pattern®. Ophthalmology. 2019 Jan:126(1):P56-P93. doi: 10.1016/j.ophtha.2018.10.019. Epub 2018 Oct 23 [PubMed PMID: 30366800]
Pelletier JS, Stewart KP, Capriotti K, Capriotti JA. Rosacea Blepharoconjunctivitis Treated with a Novel Preparation of Dilute Povidone Iodine and Dimethylsulfoxide: a Case Report and Review of the Literature. Ophthalmology and therapy. 2015 Dec:4(2):143-50. doi: 10.1007/s40123-015-0040-4. Epub 2015 Nov 2 [PubMed PMID: 26525679]
Level 3 (low-level) evidenceLibrando A, Carlesimo SC, Albanese G, Albanese GM, Migliorini R, Pacella E. Effectiveness of 0.1% topical salicylic acid on blepharoconjunctivitis affecting glaucoma patients treated with topical prostaglandin analogues: a prospective randomized trial. International journal of ophthalmology. 2018:11(12):1936-1940. doi: 10.18240/ijo.2018.12.10. Epub 2018 Dec 18 [PubMed PMID: 30588426]
Level 1 (high-level) evidencePutnam CM. Diagnosis and management of blepharitis: an optometrist's perspective. Clinical optometry. 2016:8():71-78. doi: 10.2147/OPTO.S84795. Epub 2016 Aug 8 [PubMed PMID: 30214351]
Level 3 (low-level) evidenceSuzuki T. Inflamed Obstructive Meibomian Gland Dysfunction Causes Ocular Surface Inflammation. Investigative ophthalmology & visual science. 2018 Nov 1:59(14):DES94-DES101. doi: 10.1167/iovs.17-23345. Epub [PubMed PMID: 30481812]
IRINODA K, MIKAMI H. Angular blepharoconjunctivitis and pyridoxine (vitamin B6) deficiency. A.M.A. archives of ophthalmology. 1958 Aug:60(2):303-11 [PubMed PMID: 13558802]
McCulley JP. Blepharoconjunctivitis. International ophthalmology clinics. 1984 Summer:24(2):65-77 [PubMed PMID: 6233233]
Machalińska A, Zakrzewska A, Markowska A, Safranow K, Wiszniewska B, Parafiniuk M, Machaliński B. Morphological and Functional Evaluation of Meibomian Gland Dysfunction in Rosacea Patients. Current eye research. 2016 Aug:41(8):1029-1034 [PubMed PMID: 26644191]
Liu J, Sheha H, Tseng SC. Pathogenic role of Demodex mites in blepharitis. Current opinion in allergy and clinical immunology. 2010 Oct:10(5):505-10. doi: 10.1097/ACI.0b013e32833df9f4. Epub [PubMed PMID: 20689407]
Level 3 (low-level) evidencePaulose SA, Sherman SW, Dagi Glass LR, Suh LH. Dupilumab-associated blepharoconjunctivitis. American journal of ophthalmology case reports. 2019 Dec:16():100550. doi: 10.1016/j.ajoc.2019.100550. Epub 2019 Sep 5 [PubMed PMID: 31535057]
Level 3 (low-level) evidenceBaskan C, Duman R, Balci M, Ozdogan S. A rare cause of blepharoconjunctivitis: Phthiriasis palpebrarum. Nigerian journal of clinical practice. 2014 Nov-Dec:17(6):817-8. doi: 10.4103/1119-3077.144419. Epub [PubMed PMID: 25385926]
Level 3 (low-level) evidenceLemp MA, Nichols KK. Blepharitis in the United States 2009: a survey-based perspective on prevalence and treatment. The ocular surface. 2009 Apr:7(2 Suppl):S1-S14 [PubMed PMID: 19383269]
Level 3 (low-level) evidenceSchaumberg DA, Nichols JJ, Papas EB, Tong L, Uchino M, Nichols KK. The international workshop on meibomian gland dysfunction: report of the subcommittee on the epidemiology of, and associated risk factors for, MGD. Investigative ophthalmology & visual science. 2011 Mar:52(4):1994-2005. doi: 10.1167/iovs.10-6997e. Epub 2011 Mar 30 [PubMed PMID: 21450917]
McCulley JP, Dougherty JM. Blepharitis associated with acne rosacea and seborrheic dermatitis. International ophthalmology clinics. 1985 Spring:25(1):159-72 [PubMed PMID: 3156100]
Raskin EM, Speaker MG, Laibson PR. Blepharitis. Infectious disease clinics of North America. 1992 Dec:6(4):777-87 [PubMed PMID: 1460262]
Greene JB, Jeng BH, Fintelmann RE, Margolis TP. Oral azithromycin for the treatment of meibomitis. JAMA ophthalmology. 2014 Jan:132(1):121-2. doi: 10.1001/jamaophthalmol.2013.5295. Epub [PubMed PMID: 24201556]
Level 2 (mid-level) evidenceDownie LE, Ng SM, Lindsley KB, Akpek EK. Omega-3 and omega-6 polyunsaturated fatty acids for dry eye disease. The Cochrane database of systematic reviews. 2019 Dec 18:12(12):CD011016. doi: 10.1002/14651858.CD011016.pub2. Epub 2019 Dec 18 [PubMed PMID: 31847055]
Level 1 (high-level) evidence