Introduction
Photosensitivity refers to various symptoms, diseases, and conditions (photodermatoses) caused or exacerbated by exposure to sunlight[1]. It is classified into five categories: primary photodermatosis, exogenous photodermatosis, photo-exacerbated dermatoses, metabolic photodermatosis, and genetic photodermatosis.
Primary or autoimmune photodermatoses
- Polymorphic light eruption[2]
- Juvenile spring eruption
- Actinic folliculitis
- Actinic prurigo[3]
- Solar urticaria[4]
- Chronic actinic/photosensitivity dermatitis[5]
- Hydroa vacciniforme (associated with Epstein-Barr virus)[6]
Exogenous or drug/chemical-induced photodermatoses[7][8]
- Drug-induced photosensitivity: common photosensitizing drugs are thiazides, tetracyclines, non-steroidal anti-inflammatory drugs (NSAIDs), phenothiazines, voriconazole, quinine, vemurafenib, and many others[7]
- Photocontact dermatitis: due to phototoxic chemicals such as psoralens in plants, vegetables, fruit; fragrances in cosmetics; sunscreen chemicals; dyes and disinfectants[9]
- Pseudoporphyria: induced by drugs and/or renal insufficiency[10]
Photo-exacerbated or photo-aggravated dermatoses
Usually:
- Cutaneous lupus erythematosus (acute, subacute and chronic variants)[11]
- Dermatomyositis[12]
- Sjogren syndrome
- Darier disease[13]
- Rosacea[14]
- Melasma[15]
Sometimes:
- Pemphigus vulgaris
- Pemphigus foliaceus[16]
- Atopic dermatitis[17]
- Seborrhoeic dermatitis[18]
- Psoriasis[19]
- Lichen planus (actinicus)[20]
- Erythema multiforme[21]
- Mycosis fungoides[22]
Metabolic photodermatoses (rare)
- Porphyria cutanea tarda[23]
- Erythropoietic protoporphyria
- Variegate porphyria[24]
- Erythropoietic porphyria (Gunther disease)[25]
Genetic photodermatoses (very rare disorders due to genomic instability)
- Xeroderma pigmentosum[26]
- Cockayne syndrome[27]
- Trichothiodystrophy[28]
- Bloom syndrome[29]
- Rothmund Thomson syndrome[30]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology of a photodermatosis depends on its classification (see individual topic articles). Some are due to autoimmune reactions, drugs, connective tissue disease, and abnormal inherited biochemical pathways.
Epidemiology
Photosensitivity may be observed in both males and females at all ages and in all ethnic groups. Different types of photosensitivity may be prevalent at different times of life. Genetic and environmental factors intervene in the occurrence of photosensitivity.
Pathophysiology
Photosensitivity is caused by an abnormal reaction to a component of the electromagnetic spectrum of sunlight and a chromophore (reactive compound) within the skin. Patients can be sensitive to one kind of sunlight, for example only to ultraviolet radiation, ultraviolet A or B (UVA, UVB), or visible light, or to a wider range of radiation. The most common photosensitivity is to UVA. Mainly, exposure to visible light triggers porphyria.
Histopathology
Each category and sub-category of photosensitivity has a unique reaction pattern seen on pathology. See the individual chapter for the unique histopathologic characteristics of each entity.
History and Physical
The clinical features depend on the specific photodermatosis.
- Photodermatoses affect areas exposed to sunlight, usually the face, neck, hands, and do not affect areas not exposed to the light (covered at least by underwear), or are less severe in covered areas.
- Sometimes they spare areas that habitually are exposed to the light, for example, the face of a polymorphic light eruption.
- Sometimes they only affect certain parts of the body, for instance, juvenile spring eruption is confined to the tops of the ears.
- Photodermatoses may also occur following indoor exposure to artificial sources of UVR like fluorescent lamps or visible radiation.
- Genomic instability due to DNA repair deficiency disease causes pigmentary changes and high risk (1000 times normal) of skin tumors including basal cell carcinoma, squamous cell carcinoma, and melanoma.
- Children with the photosensitive genodermatoses have characteristic cutaneous features and abnormalities of other organs.
Clues to photosensitivity include:
- Summer exacerbation; although, note that many photodermatoses are present year round
- Sharp cut-off between affected area and skin covered by clothing or jewellery (e.g., watch strap, ring)
- Sparing of folds of upper eyelids
- Sparing of deep furrows on face and neck
- Sparing of skin covered by hair
- Sparing of skin shadowed by the ears, under the nose and the chin
- Sparing of the web spaces between the fingers.
Evaluation
Medical practitioners diagnose photosensitivity by a history of a skin problem arising from exposure to sunlight. They determine the specific type by taking a careful history, examining the skin and performing specific tests. Photosensitivity is sometimes confirmed by photosets, which only is available in specialized centers.
- Minimal erythema dose (MED) testing (broadband or monochromators) to determine threshold dose
- Provocation photoset procedure using repeated exposures to UVA and/or UVB over four consecutive days in an attempt to reproduce the dermatosis
- Photopatch tests in association with standard patch tests to determine photoallergy
Investigations may include:
- Full blood count
- Connective tissue antibodies including antinuclear antibodies (ANA), extractable nuclear antigens (ENA) if suspicious of lupus erythematosus
- Porphyrins in blood, urine, and feces
- Liver function and iron tests in patients suspected of porphyria
- Skin biopsy for histopathology and direct immune fluorescence in primary and photo-exacerbated dermatoses
- In cases suspicious of xeroderma pigmentosum, measurement of post-UV cell survival and DNA repair capacity in fibroblast assays
- Tiger hair appearance on polarised microscopy of brittle hair (dark and light areas) should lead to chromatography to determine amino acid content, which shows reduced cysteine in trichothiodystrophy
- Gene sequencing may confirm Bloom syndrome or Rothmund Thomson syndrome.
Treatment / Management
Management of photosensitivity involves sun protection and treatment of the underlying disorder. Mainly, photosensitivity reactions are prevented by careful protection from sun exposure and avoidance of exposure to artificial sources of UVR. Use of websites and smartphone apps that indicate local ultraviolet levels are helpful to understand when protection is most essential. There is more ultraviolet radiation in the tropics compared to temperate areas, in the Southern hemisphere compared to the Northern, during summer compared to winter, at high altitude compared to sea level, and in the middle of the day compared to the extremes of the day.
Protection involves:[31]
- Avoiding exposure to direct sunlight
- Staying indoors and away from windows, and seeking shade when outdoors
- Dressing up in covering clothing and wearing a wide-brimmed hat when outdoors. Some clothing is labeled with ultraviolet protection factor (UPF). Best protection from clothing is obtained from thick, tightly woven, dry and dark colored polyester, denim or wool
- Broad-spectrum sunscreen SPF 50 or higher, covering all exposed skin. Sunscreen should protect from UVB and UVA and be water resistant. It should be applied generously and reapplied every two hours while outdoors
- Tanning products containing dihydroxyacetone provide modest photoprotection against UVA and to a lesser extent against UVB.
SPF is sun protection factor, defined as the dose of solar radiation needed to induce just perceptible erythema (minimal erythema dose, MED) on skin treated with 2 mg/cm sunscreen divided by the MED on untreated skin. SPF primarily describes protection from UVB, as it reflects protection from the erythema action spectrum.
The primary photodermatosis polymorphic light eruption may be paradoxically effectively treated by graduated, and cautious, exposure to ultraviolet radiation.[32](B3)
Differential Diagnosis
The first step in considering a diagnosis within the broad scope of photosensitivity is to consider each category of photosensitivity and the specific entities within the given category; whether it is primary photosensitivity such as polymourphous light eruption, autoimmune photosensitivity such as lupus erythematosus, photo-exacerbated or aggravated such as dermatomyositis, genetic such as xeroderma pigmentosum, or metabolic such as porphyria cutanea tarda. Then using the history and physical exam, narrow down the differential. For example, a polymourphous light eruption(PMLE) may be distinguised from lupus erythematosus by the history, presentation, and clinical appearance of these lesions. For photoexacerbated diseases such as dermatomyositis, other clinical findings such as capillary abnormalities around the nail folds or gottron papules over the bony prominences usually help with distinction from other entities such as drug enduced photosensitivity. Once the general category has been suspected, a differential can be developed within that category and helps with the diagnosis. For the differential diagnosis of each entity, please see the specific chapter of that entity.
Prognosis
The prognosis of each entity is unique, please see the individual chapters for each condition.
Complications
The complications of each entity is unique, please see the individual chapters for each condition.
Deterrence and Patient Education
In general, treatment of photosensitivity regardless of the entity is going to center around managing symptoms and pursuing photoprotection.
Pearls and Other Issues
Patients with photodermatoses also may need to:
- Take vitamin D supplements and oral antioxidants
- Wear a clear plastic mask to protect the face
- Choose gray-tinted laminated glass for automobile
- Apply photoprotective UV films to windows at home, school work, and vehicles
- Have regular skin checks to locate and treat skin cancers early.
Enhancing Healthcare Team Outcomes
The healthcare team, including nurses, pharmacists, and clinicians must work together to educate patients with photodermatoses as they need to be reminded to take vitamin D supplements and oral antioxidants, wear a clear plastic mask to protect the face, choose gray-tinted laminated glass for their automobile, and apply photoprotective UV films to windows at home, school work, and vehicles. The team should remind patients they need to have regular skin checks to locate and treat skin cancers early. [Level V]
Media
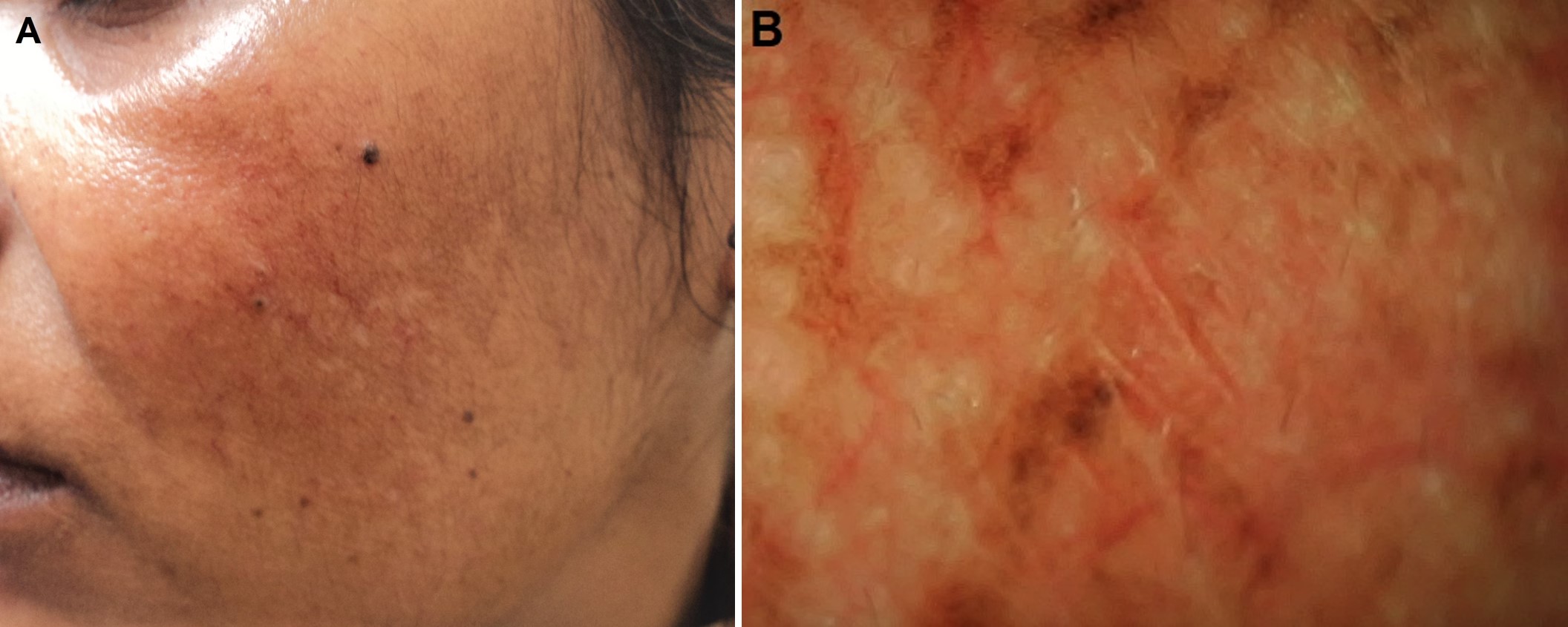
(Click Image to Enlarge)
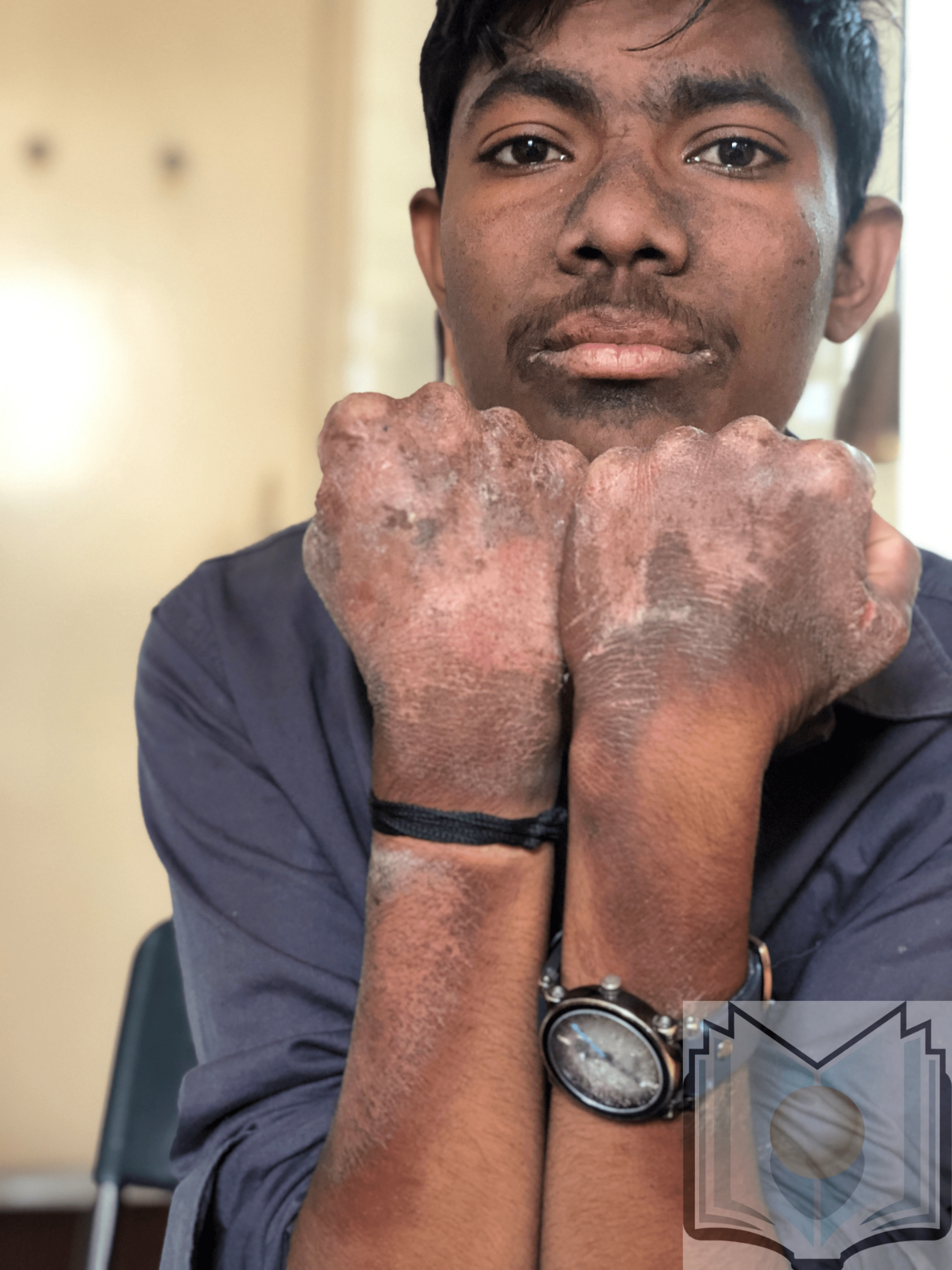
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Lehmann P, Schwarz T. Photodermatoses: diagnosis and treatment. Deutsches Arzteblatt international. 2011 Mar:108(9):135-41. doi: 10.3238/arztebl.2011.0135. Epub 2011 Mar 4 [PubMed PMID: 21442060]
Lembo S, Raimondo A. Polymorphic Light Eruption: What's New in Pathogenesis and Management. Frontiers in medicine. 2018:5():252. doi: 10.3389/fmed.2018.00252. Epub 2018 Sep 10 [PubMed PMID: 30250845]
Pile HD, Crane JS. Actinic Prurigo. StatPearls. 2023 Jan:(): [PubMed PMID: 29763132]
Photiou L,Foley P,Ross G, Solar urticaria - An Australian case series of 83 patients. The Australasian journal of dermatology. 2018 Dec 25; [PubMed PMID: 30585308]
Level 2 (mid-level) evidencePaek SY, Lim HW. Chronic actinic dermatitis. Dermatologic clinics. 2014 Jul:32(3):355-61, viii-ix. doi: 10.1016/j.det.2014.03.007. Epub [PubMed PMID: 24891057]
Ahad T, Rhodes LE. Images in paediatrics: Haemorrhagic vesicles and varioliform scarring: consider photosensitivity. Archives of disease in childhood. 2020 Mar:105(3):302-303. doi: 10.1136/archdischild-2018-316272. Epub 2018 Nov 13 [PubMed PMID: 30425076]
Blakely KM, Drucker AM, Rosen CF. Drug-Induced Photosensitivity-An Update: Culprit Drugs, Prevention and Management. Drug safety. 2019 Jul:42(7):827-847. doi: 10.1007/s40264-019-00806-5. Epub [PubMed PMID: 30888626]
Ibbotson S . Drug and chemical induced photosensitivity from a clinical perspective. Photochemical & photobiological sciences : Official journal of the European Photochemistry Association and the European Society for Photobiology. 2018 Dec 5:17(12):1885-1903. doi: 10.1039/c8pp00011e. Epub [PubMed PMID: 30283959]
Level 3 (low-level) evidenceSnyder M, Turrentine JE, Cruz PD Jr. Photocontact Dermatitis and Its Clinical Mimics: an Overview for the Allergist. Clinical reviews in allergy & immunology. 2019 Feb:56(1):32-40. doi: 10.1007/s12016-018-8696-x. Epub [PubMed PMID: 29951786]
Level 3 (low-level) evidenceVelander MJ, Þorsteinsdóttir S, Bygum A. [Clinical review of pseudoporphyria]. Ugeskrift for laeger. 2015 Feb 2:177(6):. pii: V11140599. Epub [PubMed PMID: 25650579]
Foering K, Chang AY, Piette EW, Cucchiara A, Okawa J, Werth VP. Characterization of clinical photosensitivity in cutaneous lupus erythematosus. Journal of the American Academy of Dermatology. 2013 Aug:69(2):205-13. doi: 10.1016/j.jaad.2013.03.015. Epub 2013 May 3 [PubMed PMID: 23648190]
Level 2 (mid-level) evidenceAuriemma M, Capo A, Meogrossi G, Amerio P. Cutaneous signs of classical dermatomyositis. Giornale italiano di dermatologia e venereologia : organo ufficiale, Societa italiana di dermatologia e sifilografia. 2014 Oct:149(5):505-17 [PubMed PMID: 25014587]
Baba T, Yaoita H. UV radiation and keratosis follicularis. Archives of dermatology. 1984 Nov:120(11):1484-7 [PubMed PMID: 6497416]
Level 3 (low-level) evidenceMurphy G. Ultraviolet light and rosacea. Cutis. 2004 Sep:74(3 Suppl):13-6, 32-4 [PubMed PMID: 15499753]
Suggs AK,Hamill SS,Friedman PM, Melasma: update on management. Seminars in cutaneous medicine and surgery. 2018 Dec; [PubMed PMID: 30475935]
Igawa K, Matsunaga T, Nishioka K. Involvement of UV-irradiation in pemphigus foliaceus. Journal of the European Academy of Dermatology and Venereology : JEADV. 2004 Mar:18(2):216-7 [PubMed PMID: 15009310]
Level 3 (low-level) evidenceEllenbogen E, Wesselmann U, Hofmann SC, Lehmann P. Photosensitive atopic dermatitis--a neglected subset: Clinical, laboratory, histological and photobiological workup. Journal of the European Academy of Dermatology and Venereology : JEADV. 2016 Feb:30(2):270-5. doi: 10.1111/jdv.13451. Epub 2015 Nov 2 [PubMed PMID: 26523351]
Palmer RA, Hawk JL. Light-induced seborrhoeic eczema: severe photoprovocation from subclinical disease. Photodermatology, photoimmunology & photomedicine. 2004 Feb:20(1):62-3 [PubMed PMID: 14738536]
Level 3 (low-level) evidenceWolf P,Weger W,Patra V,Gruber-Wackernagel A,Byrne SN, Desired response to phototherapy vs photoaggravation in psoriasis: what makes the difference? Experimental dermatology. 2016 Dec; [PubMed PMID: 27376966]
Tiwary AK. Actinic Lichen Planus. Indian pediatrics. 2018 Aug 15:55(8):715 [PubMed PMID: 30218531]
Rodríguez-Pazos L, Gómez-Bernal S, Rodríguez-Granados MT, Toribio J. Photodistributed erythema multiforme. Actas dermo-sifiliograficas. 2013 Oct:104(8):645-53. doi: 10.1016/j.adengl.2012.01.024. Epub 2013 Aug 17 [PubMed PMID: 23962583]
Haber R, Ram-Wolff C, Laly P, Bouaziz JD, Jachiet M, Rivet J, Bagot M. Photo-sensitive mycosis fungoides: a new variant? European journal of dermatology : EJD. 2017 Apr 1:27(2):181-182. doi: 10.1684/ejd.2016.2924. Epub [PubMed PMID: 27869099]
Singal AK, Porphyria cutanea tarda: Recent update. Molecular genetics and metabolism. 2019 Nov [PubMed PMID: 30683557]
Wang B, Rudnick S, Cengia B, Bonkovsky HL. Acute Hepatic Porphyrias: Review and Recent Progress. Hepatology communications. 2019 Feb:3(2):193-206. doi: 10.1002/hep4.1297. Epub 2018 Dec 20 [PubMed PMID: 30766957]
Erwin AL, Desnick RJ. Congenital erythropoietic porphyria: Recent advances. Molecular genetics and metabolism. 2019 Nov:128(3):288-297. doi: 10.1016/j.ymgme.2018.12.008. Epub 2018 Dec 27 [PubMed PMID: 30685241]
Level 3 (low-level) evidenceLehmann J, Seebode C, Martens MC, Emmert S. Xeroderma Pigmentosum - Facts and Perspectives. Anticancer research. 2018 Feb:38(2):1159-1164 [PubMed PMID: 29374753]
Level 3 (low-level) evidenceHafsi W, Badri T. Cockayne Syndrome. StatPearls. 2023 Jan:(): [PubMed PMID: 30252254]
Yew YW, Giordano CN, Spivak G, Lim HW. Understanding photodermatoses associated with defective DNA repair: Photosensitive syndromes without associated cancer predisposition. Journal of the American Academy of Dermatology. 2016 Nov:75(5):873-882. doi: 10.1016/j.jaad.2016.03.044. Epub [PubMed PMID: 27745642]
Level 3 (low-level) evidenceHafsi W, Badri T, Rice AS. Bloom Syndrome. StatPearls. 2023 Jan:(): [PubMed PMID: 28846287]
Giordano CN,Yew YW,Spivak G,Lim HW, Understanding photodermatoses associated with defective DNA repair: Syndromes with cancer predisposition. Journal of the American Academy of Dermatology. 2016 Nov [PubMed PMID: 27745641]
Level 3 (low-level) evidenceGozali MV, Zhou BR, Luo D. Update on treatment of photodermatosis. Dermatology online journal. 2016 Feb 17:22(2):. pii: 13030/qt1rx7d228. Epub 2016 Feb 17 [PubMed PMID: 27267185]
Guarrera M. Polymorphous Light Eruption. Advances in experimental medicine and biology. 2017:996():61-70. doi: 10.1007/978-3-319-56017-5_6. Epub [PubMed PMID: 29124691]
Level 3 (low-level) evidence