Introduction
The infratemporal fossa is an irregularly shaped cavity in the face that is touted as being one of the most anatomically complex regions in the head and neck. The location of the infratemporal fossa makes it an area of interest for pathology treated by many surgical subspecialties including otolaryngology, neurosurgery, and maxillofacial surgery. The anatomic space defined as the infratemporal fossa contains a variety of nerves, arteries, veins, and muscles. A clinically significant feature of the infratemporal fossa involves potentially life-threatening spread of infection from the infratemporal fossa through the pterygoid plexus to the cavernous sinus. This review article will highlight the important anatomic landmarks and structures contained in and around the infratemporal fossa.[1][2]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
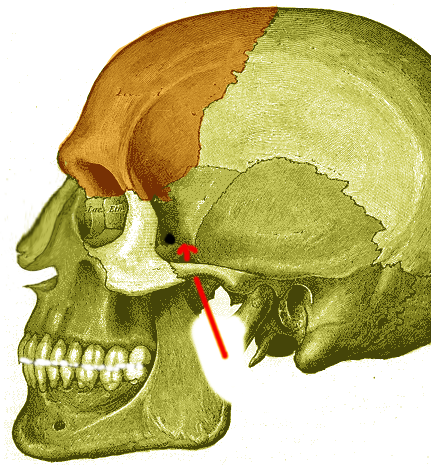
The structure of the infratemporal fossa is formed by osseous boundaries located inferiorly and medially to the zygomatic arch. The shape of the infratemporal fossa can be loosely described as an inverted square pyramid containing directional boundaries that delineate its area. Anteriorly, the boundary is formed by the posterolateral surface of the maxillary sinus. The ramus of the mandible forms the lateral boundary while the medial pterygoid and tensor veli palatini muscles form the medial border. The medial border of the infratemporal fossa is continuous with the pterygopalatine fossa. The medial pterygoid muscle attachment to the mandible also forms the inferior border. The lateral pterygoid muscle is located anteromedially to the infratemporal fossa. The posterior boundary of the infratemporal fossa is broadly defined but includes the styloid process and the tympanic part of the temporal bone. Since it an anatomical landmark in the head and neck, the infratemporal fossa functions to house and protect a wide variety of nerves and vasculature that course through the space.[1][3]
Embryology
The infratemporal fossa encompasses a space that contains a wide variance of embryologic derivation. The mandible and the maxillary artery are formed from the first pharyngeal arch, also known as the mandibular arch. Other anterior bones of the face that participate in the boundaries of the infratemporal fossa, including the maxilla, temporal bone, and zygomatic bone, derive from the mesenchyme of neural crest cells and undergo membranous ossification.[4]
Blood Supply and Lymphatics
The vasculature found in and around the infratemporal fossa has a prominent clinical significance. As previously mentioned, the pterygoid plexus overlying the lateral pterygoid muscle is present within the fossa. This venous plexus connects to the cavernous sinus and eventually drains into the maxillary vein. Infectious processes originating in the infratemporal fossa have the potential to spread via this venous plexus to the cavernous sinus and result in a cavernous sinus thrombosis. In addition to the pterygoid venous plexus, the retromandibular vein is also found within the infratemporal fossa.
Prominent arteries present in the infratemporal fossa include the maxillary artery and associated branches, including the middle meningeal artery and accessory meningeal artery. The maxillary artery is the seventh branch of the external carotid artery. It courses through the infratemporal fossa between the sphenomandibular ligament and condylar process of the mandible to enter the pterygopalatine fossa. Prominent branches of the maxillary artery found in the infratemporal fossa include the middle meningeal artery, inferior alveolar artery, deep temporal artery, and buccal artery. The middle meningeal artery courses between the tensor veli palatine muscle and lateral pterygoid muscle to enter the middle cranial fossa through the foramen spinosum. The accessory meningeal artery can arise from either the maxillary or middle meningeal artery to provide ancillary blood supply to this region.
The posterior boundary of the infratemporal fossa is loosely defined, but some definitions include the internal carotid artery and internal jugular vein. One of the most feared complications of surgery in the infratemporal fossa includes accidental incision of the internal carotid artery. Many surgeons confirm that they are in contact with the internal or external carotid artery by blocking the vessel and checking the pulse at the superficial temporal artery. Pulseless activity in the artery following blocking confirms that the external carotid artery is blocked.[3][1][5]
Nerves
Nerves coursing through and around the infratemporal fossa are responsible for providing a vast majority of sensory and motor function to the lower face and other important structures such as the dura mater. The largest of these nerves is the mandibular branch of the trigeminal nerve that passes through the foramen ovale of the sphenoid before entering the infratemporal fossa. The mandibular nerve bifurcates into a smaller anterior branch and a larger posterior branch. Just before this bifurcation, the mandibular nerve gives off motor nerves to supply the medial pterygoid, tensor tympani, and tensor veli palatini muscles, as well as the meningeal branch of the mandibular which supplies the dura mater.
Following the bifurcation, the anterior division of the mandibular nerve provides motor supply to the masseter, temporalis, and lateral pterygoid muscles via individual branches. Additionally, the buccal nerve from the anterior division courses between the two heads of the lateral pterygoid to provide sensory innervation from the buccal membrane in the oral cavity and the posterior lower second and third molar teeth.
The larger posterior division of the mandibular nerve gives rise to three main nerves: the auriculotemporal, lingual, and inferior alveolar nerves. Both the inferior alveolar and lingual nerves course between the lateral and medial pterygoid muscles, crossing the lateral side of the medial pterygoid. The inferior alveolar provides sensation to the lower teeth and terminates as the mental nerve, providing sensation to the lower lip and chin. The inferior alveolar nerve also provides the motor function to the mylohyoid and anterior digastric muscles. The lingual nerve carries general sensation from the anterior two-thirds of the tongue. The lingual nerve is joined by the chorda tympani nerve in the infratemporal fossa to provide presynaptic parasympathetic axons to the submandibular ganglion from the facial nerve. The chorda tympani nerve is also responsible for carrying taste sensation from the anterior two-thirds of the tongue. The auriculotemporal branch of the posterior division is a sensory nerve supplying various regions on the lateral portion of the head.
Further autonomic nervous system association within the infratemporal fossa includes the otic ganglion on the medial side of the mandibular nerve close to the foramen ovale. The otic ganglion is presynaptically linked with the glossopharyngeal nerve, and postsynaptic parasympathetic axons innervate the parotid gland by joining fibers of the auriculotemporal nerve.[1][3]
Muscles
The lateral pterygoid muscle contains two heads and occupies most of the area in the superior infratemporal fossa. This muscle is often used as a landmark for dissection depending on the surgical approach that will be discussed further in the following section. The upper head of the lateral pterygoid muscle originates from the greater wing of the sphenoid and infratemporal surface and inserts on the joint capsule of the temporomandibular joint. The lower head originates from the lateral pterygoid plate and inserts inferior to the condylar process of the mandible at the pterygoid fovea. The lateral pterygoid is the only muscle of mastication that functions to depress the mandible, allowing the jaw to open.
Located inferior to the lateral pterygoid muscle in the infratemporal fossa is the medial pterygoid muscle. The medial pterygoid also contains 2 origins from the maxillary tuberosity and lateral pterygoid plate, respectively. Both heads course posteriorly to form a common insertion tendon with the masseter muscle on the medial surface of the ramus of the mandible, allowing the muscles to function synergistically as powerful jaw elevators.
The tensor veli palatini and levator veli palatini are two muscles also seen in the infratemporal fossa that interact to facilitate elevation of the palate to prevent food from entering the nasopharynx when swallowing. Additionally, the contraction of both muscles allows the opening of the Eustachian tube to equalize the pressure between the middle ear and nasopharynx.[1][6]
Surgical Considerations
Surgical procedures related to the infratemporal fossa are complicated due to the intricate anatomy present in this area. Complications related to surgical intervention in the infratemporal fossa include hearing loss, facial nerve weakness, temporomandibular joint dysfunction, dental malocclusion, and cosmetic deformities. One of the most life-threatening complications of surgery in the infratemporal fossa includes accidental incision of the internal carotid artery. This can result in profuse hemorrhage and rapid death. One technique employed by surgeons to confirm whether a visible vessel is the internal or external carotid artery involves the temporary blocking of the vessel and checking the pulse of the superficial temporal artery. Pulselessness of this artery confirms that the external carotid is blocked. In this section, we will explore 2 traditional surgical approaches to pathology in the infratemporal fossa.
The classic lateral approach to the infratemporal fossa involves beginning with a posterior auricular incision. This is followed by mastoidectomy, parotidectomy with facial nerve dissection, and disarticulation of the mandible from the temporomandibular joint. Disarticulation of the mandibular joint is performed instead of mastication muscle dissection due to severe trismus that can occur from fibrosis of the muscles following incision and healing. The lateral approach provides great exposure to the entire unilateral infratemporal fossa and good control over vasculature. Disadvantages of this approach include an increased risk of hearing loss, facial nerve weakness, and temporomandibular joint dysfunction.
The anterior approach involves utilizing the airspace of the maxillary sinus and can be performed either endoscopically or the traditional open approach depending on the degree of pathology. The traditional transmaxillary approach involves a facial dissection followed by Le Fort osteotomy, maxillary sinusotomy, and maxillectomy. Advantages of this approach include safety margins provided by the natural airspace within the sinus cavities. Disadvantages include limited exposure to the infratemporal fossa and distal access point.
Another anterior approach utilizing endoscopic technology includes the endonasal endoscopic approach. This approach utilizes small intranasal incisions to reach the infratemporal fossa using endoscopic equipment. This approach is advantageous by avoiding cosmetic morbidity while still providing a detailed view of the infratemporal fossa. One major complication that can result from this approach includes difficulty controlling hemorrhage in the area if bleeding occurs.[1][7]
Clinical Significance
The clinical significance of the infratemporal fossa involves neoplastic and infectious processes that can either arise from this area or spread to it. Pathology found in this region tends to spread posteriorly due to anterior, medial, and lateral bony barriers present in the infratemporal fossa. Symptoms experienced from pathology present in this region include trismus and any manifestation of mandibular nerve compression including paresis of mastication muscles, numbness or loss of taste sensation from the tongue, anesthesia of the gums, or speech articulation difficulties.
Neoplastic tumors that have been documented in the infratemporal fossa are numerous and include rhabdomyosarcoma, liposarcoma, fibrosarcoma, meningioma, hemangioma, and peripheral nerve sheath tumors arising from any of the nerves in this region. Schwannomas and neurofibromas are typically found between the pterygoid muscles due to the location of the lingual and inferior alveolar nerves in this region. Hemangiomas arising from the pterygoid venous plexus can also be seen in this area often between the lateral pterygoid and temporalis muscles.
The infratemporal fossa also provides a space into which tumors originating from other regions can spread. Tumors found in the nasopharynx and sphenoid sinus are known to spread to the infratemporal fossa. Meningiomas can spread to the infratemporal fossa through the foramen ovale and often push the lateral and medial pterygoids apart. Due to the continuity of the infratemporal fossa with the inferior parapharyngeal space, larger neoplasms have the potential to spread to this region.
Although rare, infectious processes including abscesses can be seen within the infratemporal fossa. As previously mentioned, infections in the infratemporal can spread to the cavernous sinus and cause cavernous sinus thrombosis. Due to the complex anatomy of the infratemporal fossa, a multidisciplinary team-based approach involving otolaryngology and oral-maxillofacial surgery is often employed to treat these issues surgically.[1][8]
Media
References
Joo W, Funaki T, Yoshioka F, Rhoton AL Jr. Microsurgical anatomy of the infratemporal fossa. Clinical anatomy (New York, N.Y.). 2013 May:26(4):455-69. doi: 10.1002/ca.22202. Epub 2013 Jan 27 [PubMed PMID: 23355316]
Emes Y, Yalcin S, Aybar B, Bilici IS. Infratemporal fossa infection with inferior alveolar nerve involvement. Journal of Istanbul University Faculty of Dentistry. 2016:50(3):46-50. doi: 10.17096/jiufd.34851. Epub 2016 Oct 1 [PubMed PMID: 28955575]
Guo YX, Sun ZP, Liu XJ, Bhandari K, Guo CB. Surgical safety distances in the infratemporal fossa: three-dimensional measurement study. International journal of oral and maxillofacial surgery. 2015 May:44(5):555-61. doi: 10.1016/j.ijom.2014.06.004. Epub 2014 Nov 11 [PubMed PMID: 25441861]
Burford CM, Mason MJ. Early development of the malleus and incus in humans. Journal of anatomy. 2016 Dec:229(6):857-870. doi: 10.1111/joa.12520. Epub 2016 Jul 26 [PubMed PMID: 27456698]
Şimşek Kaya G, Daltaban Ö, Kaya M, Kocabalkan B, Sindel A, Akdağ M. The potential clinical relevance of anatomical structures and variations of the maxillary sinus for planned sinus floor elevation procedures: A retrospective cone beam computed tomography study. Clinical implant dentistry and related research. 2019 Feb:21(1):114-121. doi: 10.1111/cid.12703. Epub 2018 Dec 17 [PubMed PMID: 30556642]
Level 2 (mid-level) evidencePerez C. Temporomandibular disorders in children and adolescents. General dentistry. 2018 Nov-Dec:66(6):51-55 [PubMed PMID: 30444707]
Bozkurt G, Turri-Zanoni M, Russo F, Elhassan HA, Castelnuovo P, Battaglia P. Ultrasonic Scalpel-Assisted Endoscopic Endonasal Surgery of Infratemporal Fossa: Our First Impressions. World neurosurgery. 2019 Mar:123():23-28. doi: 10.1016/j.wneu.2018.11.202. Epub 2018 Dec 3 [PubMed PMID: 30521958]
Park MY, Kim HS, Ko HC, Kim MB, Kim BS. Infratemporal fossa abscess of dental origin: a rare, severe and misdiagnosed infection. Journal of the Korean Association of Oral and Maxillofacial Surgeons. 2018 Feb:44(1):37-39. doi: 10.5125/jkaoms.2018.44.1.37. Epub 2018 Feb 26 [PubMed PMID: 29535969]