Introduction
Tricuspid regurgitation is a comparatively common anomaly. Although mild tricuspid regurgitation is commonly present, hemodynamically significant tricuspid regurgitation can lead to right ventricular dysfunction and cause substantial morbidity and mortality. Structural modifications of any or all of the tricuspid valve apparatus may cause the development of tricuspid regurgitation.
Anatomy
The right atrioventricular valve apparatus, or tricuspid valve complex (see Image. Valves of the Heart), consists of the following 4 components:
- Valve leaflets: Anterior, posterior, and septal
- Fibrous tricuspid valve annulus
- Supporting chordae tendineae
- Papillary muscles: from 2 to 9.[4]
- Just before the onset of the right ventricular systole, the papillary muscle contracts to increase tension in the chordae tendineae so that the 3-valve cusps coapt, preventing regurgitation across the tricuspid valve.[5]
The conduction system and the fibroelastic cardiac skeleton's supporting structure coordinate the tricuspid valve's actions. The tricuspid valve is located between the right atrium and the right ventricle and has a valve area of 4 to 6 cm2.[2]
The pathophysiological variants of the tricuspid valve include the following:
- Ebstein anomaly
- Tricuspid atresia
- Congenital tricuspid stenosis
- Congenital cleft of the anterior leaflet
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
In tricuspid regurgitation, lesions fall into 2 categories: primary, where intrinsic abnormalities in the tricuspid valvular apparatus are responsible, and secondary, where right atrial or ventricular dilatation causes tricuspid regurgitation. The most common cause of tricuspid regurgitation is secondary or functional regurgitation. Secondary disorders like tricuspid annular dilation and leaflet tethering in right ventricular pressure and volume overload are largely responsible for tricuspid regurgitation compared to primary disorders involving the valve apparatus.[6][7][8]
Secondary Tricuspid Regurgitation
Tricuspid regurgitation is most commonly secondary in adults, with probable normal anatomical leaflets and chords. Dilatation of the right atrium and the right ventricle, along with dilatation of the tricuspid annulus and tethering of the tricuspid valve leaflet, are some of the causes of secondary tricuspid regurgitation.[9] This may result from conditions affecting the right ventricle or may be due to an increase in right ventricle systolic pressure, often with pulmonary hypertension. The valves are anatomically normal, but because of the enlarged right ventricular cavity and dilatation of the annulus, the leaflets fail to coapt appropriately. Conditions affecting the right ventricle that eventually cause tricuspid regurgitation include cardiomyopathies and ischemic heart diseases involving the right ventricular myocardium and tricuspid papillary muscles.[10]
The conditions that induce pulmonary hypertension and secondary right ventricle dilatation include the following:
- Left-sided heart disease: Left ventricular dysfunction or left-sided valvular heart disease resulting in pulmonary hypertension
- Pulmonary hypertension: Cor pulmonale, pulmonary embolism, pulmonary hypertension of any cause left to right shunt
- Right atrial abnormalities: Atrial fibrillation [11]
- Stenosis of the pulmonic valve or pulmonary artery
- Hyperthyroidism
Primary Tricuspid Regurgitation
In adolescents and young adults, the cause of tricuspid regurgitation is usually congenital, but conditions that directly affect the tricuspid valvular apparatus are rare in adults.
Causes of primary TR include the following:
Acquired disease
- Infective endocarditis: Intravenous drug use, neoplasms, alcoholism, extensive burns, infected indwelling catheters, and immune deficiency cause infection of the valve
- An annular abscess is common.
- Iatrogenic: Direct valve injury from a permanent pacemaker or implantable cardioverter-defibrillator lead placement or removal or endomyocardial biopsy in cardiac transplant recipients.
- Its prevalence is increasing due to the widespread use of devices with right-sided leads, necessitating specialized interdisciplinary management that includes electrophysiologists skilled in device therapy and transvenous lead extraction. The condition may arise from mechanical interference of the lead with the tricuspid valve apparatus or pacing-induced right ventricular dysfunction.
- Traumatic: Chest wall or deceleration injury trauma
- Rheumatic valve disease: The most common cause of pure tricuspid regurgitation due to damage to the tricuspid leaflets.
- The valves undergo fibrous thickening without commissural fusion, fused chordae, or calcific deposits.
- Carcinoid syndrome: Isolated tricuspid regurgitation (may occur)
- The valve leaflets adhere to the right ventricular wall owing to the fibrous plaques on the valve leaflets and the endocardium. Thus, the tricuspid cusps do not coapt appropriately during systole—causing tricuspid regurgitation.[12]
- Myxomatous degeneration associated with tricuspid valve prolapse
- This occurs in as many as 40% of patients with mitral valve prolapse.
- Marantic endocarditis in systemic lupus erythematosus or rheumatoid arthritis
- Endomyocardial fibrosis
- Drug-induced disease
Congenital conditions
- Ebstein anomaly: The most common form of congenital disease affecting the tricuspid valve. The tricuspid valve's posterior and septal leaflets are displaced apically in the right ventricle, resulting in its atrialization.
- Connective tissue disorder (eg, Marfan or Ehlers-Danlos Syndrome): Pure tricuspid regurgitation is seen and may be due to mildly dilated tricuspid annulus without floppy leaflets and floppy tricuspid valve leaflets.[15]
- Tricuspid valve tethering with ventricular septal aneurysm and perimembranous ventricular septal defect
- Tricuspid valve dysplasia
- Giant right atrium
Epidemiology
Moderate to severe tricuspid regurgitation (TR) affects approximately 3% to 6% of the general population.[16] Still, its prevalence is significantly higher among patients with left-sided valve disorders, particularly those with heart failure (HF), encompassing both heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF), where it ranges from 10% to 23%.[17] In the context of heart failure, TR is linked to a higher risk of mortality and increased rates of HF-related hospitalizations.[18]
The negative impact on prognosis escalates with the severity of TR and persists regardless of right ventricular dysfunction, pulmonary hypertension, associated mitral regurgitation, left ventricular dysfunction, or atrial fibrillation.[19] Tricuspid regurgitation presents at different age groups depending on its etiology. An Ebstein anomaly may be diagnosed at birth and during early childhood. Rheumatic valvular disease is the most common form of tricuspid regurgitation in patients older than 15.
The prevalence of right heart failure (RHF) is substantial, but it varies greatly depending on the underlying causes, populations studied, and the criteria used for diagnosis. In many earlier studies, RHF has often been described as right ventricular dysfunction (RVD). Results from a meta-analysis of 11 studies involving patients with heart failure with reduced ejection fraction (HFrEF) revealed a broad range in the prevalence of RVD, from 19% to 77%, mainly due to varying definitions of RVD.[20]
Similarly, results from another meta-analysis involving 4835 patients with HFpEF found that the prevalence of RVD was 28% when defined by tricuspid annular plane systolic excursion (TAPSE) less than 16 mm, 18% when using right ventricular (RV) fractional area change (FAC) less than 35%, and 21% for RV S' less than 9.5 cm/s. Regardless of the criteria or cause, RVD has been consistently associated with an increased risk of both morbidity and mortality. The impact of RHF on survival is influenced by the clinical severity, with the most severe presentations—characterized by TAPSE less than 17 mm, New York Heart Association class IV, peripheral edema, and the need for diuretic therapy—being linked to the lowest 5-year survival rates.[21]
Pathophysiology
Primary structural abnormalities of the tricuspid valvular apparatus or secondary abnormalities due to myocardial dysfunction or dilatation are responsible for the structural incompetence of the tricuspid valve.[22] The backflow of blood from the right ventricle into the right atrium during systole defines tricuspid regulation. In mild to moderate cases of tricuspid regurgitation, no significant hemodynamic consequences are noted due to the comparatively compliant nature of the right atrium. However, in severe cases, right ventricular volume overload develops, which eventually results in right-sided congestive heart failure presenting with peripheral edema, ascites, and hepatic congestion.
The tricuspid annulus is dynamic and changes with the change in loading conditions; factors affecting the degree of tricuspid regurgitation include right ventricular preload, afterload, and right ventricular systolic function.[2] During inspiration, the severity of tricuspid regurgitation increases. The right ventricle widens during inspiration, further enlarging the tricuspid valve annulus and increasing the effective regurgitant orifice area.[23]
Carpentier’s functional classification, based on leaflet mobility, can describe secondary TR effectively. Carpentier type I corresponds to normal leaflet motion with predominant tricuspid annulus dilation, which is common in atrial secondary TR. Carpentier type IIIb involves leaflet tethering with restricted systolic motion, typically seen in ventricular secondary TR. While the Carpentier classification was initially designed to guide mitral valve surgical repair or replacement, its application for TR is less established but practical for case discussion and presentation. However, the Carpentier classification may be used to discuss and present cases.
The Carpentier classification categorizes mitral valve regurgitation into 3 types based on the motion of the leaflets:
- Type I: Normal Leaflet Motion
- Causes: Annular dilation, leaflet perforationJet Direction: Centrally directed regurgitation jet
- Type II: Excessive Leaflet Motion
- Causes: Papillary muscle rupture, chordal rupture, redundant chordaeJet Direction: Eccentric jet, directed away from the involved leaflet
- Type III: Restricted Leaflet Motion
- IIIa: Restricted in Both Systole and Diastole
- Causes: Rheumatic heart diseaseJet Direction: May be centrally or eccentrically directed
- IIIb: Restricted in Diastole
- Causes: Papillary muscle dysfunction, left ventricular dilationJet Direction: May be centrally or eccentrically directed [24]
History and Physical
Symptoms
Patients present with clinical features of right-sided heart failure. These features may be painful hepatosplenomegaly, ascites, and peripheral edema. In severe cases, pulsations in the neck from the distended and pulsatile jugular veins are noted. Exercise intolerance may be seen. Clinical features of the underlying condition causing tricuspid regurgitation may be observed. For example, pulmonary hypertension may cause symptoms such as weakness, shortness of breath, and exercise intolerance; patients presenting with infective endocarditis, a common cause of tricuspid regurgitation, may present with febrile episodes.
Physical Examination
- Jugular venous distension with a prominent V wave reflects the elevation in right atrial pressure. An increase in venous return causes jugular venous distension, which is more prominent with inspiration (Kussmaul sign)
- S3 gallop is associated with an extremely dilated right ventricle
- Pansystolic murmur: high-pitched and loudest in the fourth intercostal space in the parasternal region. The intensity of the murmur increases during inspiration, exercise, and leg raising (due to an increase in venous return) and decreases in a standing position and during the Valsalva maneuver
- Ascites
- Cachexia and jaundice
- Atrial fibrillation
- Peripheral edema
- The right ventricular heave is due to a dilated right ventricle and S4 gallop, which increases with inspiration.
Evaluation
The primary modality used to diagnose and evaluate tricuspid regurgitation is Doppler echocardiography. This modality is used to precisely contemplate regurgitant blood flow and its flow velocity and accurately measure the systolic pressure in the right ventricle. See Video. Tricuspid Valve Doppler. Echocardiography modalities have various advantages and pitfalls (see Table 1).
Echocardiographic Findings
- Tricuspid valve motion may be normal or abnormal. Characteristic primary valvular abnormalities include Ebstein anomaly, leaflet prolapse, flail leaflet, endocarditis, carcinoid heart disease, and rheumatic valve disease.
- A dilated right atrium and right ventricle in moderate to severe tricuspid regurgitation.
- The tricuspid annulus is often dilated.
- The paradoxical interventricular septal movement reflects the increased volume within the right ventricle (diastolic overload).
- Right ventricle function may be hyperdynamic, normal, or reduced, thus reflecting the underlying cause of tricuspid regurgitation and the degree of right ventricle compensation.
- There may be other abnormalities seen when tricuspid regurgitation is due to pulmonary hypertension secondary to a left-sided cardiac abnormality.
- The peak regurgitant flow velocity across the tricuspid valve is measured, which helps estimate the right ventricular and pulmonary arterial systolic pressure. The modified Bernoulli equation converts this to a pressure gradient, which is then added to estimate the right atrial pressure. Thus, the extent of pulmonary hypertension can be estimated.[25][26]
- Normal right ventricular systolic function is characterized by tricuspid annular plane systolic excursion >16 mm, fractional area change >35%, and right ventricle end-systolic area <20 cm2.
- Stages of tricuspid regurgitation are presented in Table 2.
- Parameter/severity of tricuspid regurgitation is categorized as mild, moderate, or severe (see Table 3).
Table 1. Advantages and Pitfalls of Echocardiography Modalities
|
Modality |
Advantages |
Pitfalls |
|
Color Doppler (2) dimensional echocardiography
|
Qualitative assessment |
Multiple regurgitation jets are present. |
|
Quantitative Doppler aanalysis
|
Quantitative assessment |
This Doppler is less accurate for eccentric jets and requires operator experience for precise measurements. |
|
Continuous wave analysis of tricupsid regurgitant jet |
Simple to obtain, qualitative |
The regurgitant jet should be aligned to the Doppler signal for accurate assessment and changes with loading conditions. |
|
Pulsed wave analysis of hepatic veins |
Simple to obtain |
Depending on the right atrial compliance, this may not be reliable in arrhythmias. |
Table 2. Stages of Tricuspid Regurgitation
| Stage | Definition | Valve hemodynamics and consequence | Symptoms clinical presentation | Surgical Management |
| B | Progressive tricuspid regurgitation | Central jetless than 50% Right atrial area, vena contracts <0.7 | None or minimal | Operate at the time of left-sided valve surgery if tricuspid annular dilation >4.0 cm or right heart failure (2a) |
| C | Asymptomatic severe tricuspid regurgitation | Central jet >50% of the right atrial area, vena contracts >0.7 cm, a dense jet of continuous wave doppler signal at the tricuspid valve. Hepatic vein systolic flow reversal. Dilated right atrium and right ventricle | No symptoms, elevated central venous pressure |
Surgical treatment At the time of Left heart surgery (1) If asymptomatic primary tricuspid regurgitation with progressive RV dilation/systolic dysfunction: TV surgery (2b) |
| D | Severe symptomatic tricuspid regurgitation | Central jet >50% of the right atrial area, vena contracts >0.7 cm, a dense jet of continuous wave doppler signal at the tricuspid valve. Hepatic vein systolic flow Heversal. Dilated right atrium and right ventricle. | Elevated venous pressure and signs of right heart failure, congestive hepatopathy, ascites, and edema. |
Surgical treatment At the time of left heart surgery (1) Primary tricuspid regurgitation, or secondary tricuspid regurgitation with poor response to GDMT, annular dilation without tricuspid valve surgery (2a).[27] |
Table 3. Grading Severity of Tricuspid Regurgitation Based on Echocardiography Findings
| Parameters severity of tricuspid regurgitation | Mild | Moderate | Severe |
|
Anatomic
|
Valve: Normal leaflets or mildly abnormal anatomy The right atrium and right ventricle: Usually normal size and function Inferior vena cava: Usually normal (<2 cm diameter) |
Valve: Moderately abnormal leaflets The right atrium and right ventricle: Usually normal to mild dilation Inferior vena cava: Usually normal-to-mild dilation |
Valve: Severe valve lesions like flail leaflets, perforation, and severe tethering of leaflets The right atrium and right ventricle: Usually dilated, may have reduced right ventricle function Inferior vena cava: Likely dilated (>2.5 cm diameter) |
|
Qualitative Doppler analysis
|
Color flow jet area small central, transient, or small flow convergence and faint continuous wave Doppler jet | Color flow jet moderate central, flow convergence intermediate in size and duration, and continuous wave Doppler jet dense parabolic or triangular | Color flow jet large central or eccentric and wall hugging with possible Coanda effect; flow convergence significant and throughout systole and a dense jet of continuous wave Doppler |
|
Semiquantitative
|
Vena contracta </= 0.3 cm Proximal isovelocity surface area radius <0.5 cm Hepatic vein Doppler systolic predominant |
Vena contracta 0.3 to to .69 cm Proximal isovelocity surface area radius 0.6 to 0.9 cm Hepatic vein Doppler-systolic blunting |
Vena contracta >/= 0.7 cm Proximal isovelocity surface area radius >0.9 cm Hepatic vein Doppler systolic reversal |
|
Quantitative
|
Effective regurgitant orifice area <0.2 cm2 Right ventricle <30 mL |
Effective regurgitant orifice area 0.2 to 0.39 cm2 Right ventricle 30 mL to 44 mL |
Effective regurgitant orifice area >/= 0.4 cm2 Right ventricle >/= 45 mL [11] |
Additional Tests
Chest Radiography
The following findings are noted:
- Marked cardiomegaly in severe tricuspid regurgitation
- Pleural effusions and ascites with diaphragmatic elevation
- Pulmonary arterial and venous hypertension are common
Serum chemistry: Abnormal liver function test and hyperbilirubinemia secondary to hepatic congestion may be noted.
Electrocardiography: Nonspecific ST and T waves in the right precordial leads reflecting right ventricular dysfunction seen. If pulmonary hypertension causes tricuspid regurgitation, the electrocardiogram may show right axis deviation, indicating right ventricle hypertrophy and tall R waves in V1 to V2. In severe pulmonary hypertension, right atrial hypertrophy and P pulmonale may also be present.
Cardiac catheterization: Elevated end-diastolic pressures in the right atrium and right ventricle are noted.
Cardiac CT scan and magnetic resonance (CMR) imaging can provide valuable information in defining tricuspid valve anatomy in various imaging planes; however, these imaging modalities have the limitation that flow cannot be separated from structural imaging, as can be done with color Doppler echocardiography. Both help determine the right ventricular size, function, and remodeling.
Treatment / Management
Treatment preference depends on the severity of tricuspid regurgitation, etiology, and the presence and extent of associated abnormalities, including pulmonary hypertension, heart failure, and other valve conditions.
Management of severe tricuspid regurgitation includes medical therapy, counseling regarding pregnancy and physical activity, consideration of tricuspid valve surgery, and evaluation and treatment of the underlying cause.
Medical Treatment
Control fluid overload adequately for patients with tricuspid regurgitation secondary to left-sided heart failure. Diuretics, particularly loop diuretics, are commonly recommended. Advise a restricted salt intake. Consider elevating the head of the bed to improve dyspnea. Additionally, treatment may include using digitalis, potassium-sparing diuretics, angiotensin-converting enzyme inhibitors, and anticoagulants for optimal management in these cases. Atrial fibrillation, if present, can be controlled by starting the patients on antiarrhythmics.
The following medications are used:
- Diuretics (eg, furosemide)
- Antiarrhythmics
- Digoxin
- Angiotensin-converting enzyme inhibitors
- Anticoagulants
Tricuspid Valve Surgery
The necessity for tricuspid valve surgery hinges on whether surgery for left-sided (aortic or mitral) valve disease is warranted. In a comprehensive international survey focusing on patients with severe left-sided valvular heart disease (VHD) across Europe, several key findings emerged from the results:
• Moderate to severe tricuspid regurgitation (TR) was commonly observed in patients with severe mitral valve disease but was infrequent in those with aortic valve disease.• An escalation in TR severity was linked to a more severe clinical presentation and reduced overall survival at the 6-month mark.• The rate of performing concomitant tricuspid valve (TV) procedures during left-sided heart valve surgeries was high in mitral valve surgeries but notably lower in aortic valve surgeries.• There was strong alignment (88% overall) between the guideline-recommended class I indications for concomitant TV surgery in patients with severe TR and actual clinical practice, particularly for those undergoing mitral valve surgery (95%).• In the majority of cases (76% overall), patients with moderate TR also underwent concomitant TV surgery during left-sided valve procedures.[28](B3)
For patients undergoing left-sided valve surgery
- Tricuspid valve surgery is recommended in patients with severe tricuspid regurgitation, as observed in the 2014 American Heart Association/American College of Cardiology (AHA/ACC) and the 2012 European Society of Cardiology (ESC) valvular disease guidelines [3][29][30] (A1)
For patients undergoing left-sided valve surgery and who have mild, moderate, or severe tricuspid regurgitation, concomitant tricuspid valve repair is recommended in the following cases:
- Dilation of the tricuspid annulus (transthoracic echocardiogram indicating a diameter of greater than 40 mm or 21 mm/m2 indexed for body surface area or intraoperative diameter greater than 70 mm).
- Previous history of right heart failure; this is a recommendation in the AHA/ACC valve guidelines,[31] and similar recommendations are indicated in the 2012 ESC guidelines.[32]
Isolated Tricuspid Surgery
The medical community still needs to establish the optimal timing for isolated tricuspid valve surgery. In primary tricuspid regurgitation, surgical intervention is indicated when the patient is symptomatic despite medical therapy. In patients who are refractory to medical treatment but have severe tricuspid regurgitation, tricuspid valve surgery is suggested (weak recommendation). For patients exhibiting refractoriness to medical treatment yet facing severe tricuspid regurgitation, there is a weak recommendation for tricuspid valve surgery. The preferred timing is before the onset of significant right ventricular dysfunction to control or prevent symptoms, aligning with the 2014 AHA/ACC valvular guidelines.[31](A1)
Tricuspid valve surgery is strongly recommended in symptomatic and severe isolated tricuspid regurgitation without right ventricular dysfunction, as per the 2012 ESC valvular guidelines.[32] In asymptomatic or minimally symptomatic patients with severe tricuspid regurgitation, the role of tricuspid valve surgery is ambiguous.
The 2014 AHA/ACC valvular guidelines note this uncertainty and include a very weak recommendation for considering tricuspid valve surgery for asymptomatic or minimally symptomatic patients with severe primary tricuspid regurgitation and progressive moderate or more significant RV dilation and systolic dysfunction.[31] The ESC guidelines view surgery in this setting slightly more favorably and indicate considering surgery in patients with severe isolated tricuspid regurgitation with mild or no symptoms and progressive right ventricular dilation or deterioration of right ventricular function.[32](A1)
Treatment Based on the Etiology
There is a recommendation to excise the tricuspid valve without immediate replacement in endocarditis. The excision of the diseased valve wipes out the endocarditis while continuing antibiotic treatment. If right heart failure symptoms prove refractory to medical management and the infection is well controlled, surgeons can insert an artificial valve. Asymptomatic tricuspid regurgitation in Ebstein anomaly does not necessitate surgery. However, symptomatic patients may require treatment through tricuspid valve repair or replacement.
For patients with tricuspid stenosis and regurgitation due to carcinoid disease, valve replacement is a viable option if the symptoms are severe or right ventricular dysfunction is evident. The procedure can significantly improve the patient's condition and, possibly, survival rate. However, repairing complex deformities is not always reliable. Previous studies have suggested using mechanical prostheses instead of bioprostheses because of the latter's potential to fail early due to carcinoid plaque formation. Nevertheless, warfarin use presents a higher bleeding risk in patients with liver dysfunction. Bioprosthetic valves may be a better choice for old and young patients, especially women of childbearing age, as it eliminates the need for long-term anticoagulation.
Differential Diagnosis
Differential diagnosis of tricuspid regurgitation include the following:
- Ascites
- Cirrhosis
- Ebstein anomaly
- Eisenmenger syndrome
- Heart failure
- Marfan syndrome
- Cardiogenic shock
- Atrial fibrillation
- Dilated cardiomyopathy
- Biliary disease
- Cor pulmonale
- Mitral regurgitation
- Carcinoid tumor
Prognosis
The growing attention to TR often called the "forgotten valve," stems from consistent evidence in three key areas. First, numerous studies have demonstrated that higher grades of TR severity are independently associated with increased mortality.[33] Second, isolated surgical procedures for TR are rarely performed and carry an in-hospital mortality rate of approximately 8% to 10%.[34] Finally, the early success of transcatheter repair and replacement techniques has expanded access to treatments that are considered relatively low-risk.[35] The prognosis of tricuspid regurgitation is generally good. The presence of elevated pulmonary artery pressure and pulmonary hypertension predict an increased incidence of right ventricular dysfunction and the need for inotropic support post tricuspid valve surgery.
Complications
Complications of Tricuspid Regurgitation
Increasing evidence suggests that severe TR significantly affects clinical outcomes across various cardiovascular conditions. The fact that many patients present late with advanced TR underscores the disease's underrecognition and the limitations of current guideline-directed medical therapies.
- Cardiac cirrhosis
- Ascites
- Thrombus formation and embolization
Complications of Operative Interventions
Due to the high in-hospital mortality rates linked to isolated tricuspid valve surgery, there is ongoing exploration of transcatheter alternatives to enhance survival and reduce hospitalizations related to heart failure.
- Heart block
- Thrombosis of the prosthetic valve
- Infection
- Arrhythmias
Postoperative and Rehabilitation Care
Postoperative and Rehabilitation Inpatient Care of Tricuspid Regurgitation
- Anticoagulation
- This may be needed in cases of atrial fibrillation or if the patient has sustained a valve replacement.
- Management of arrhythmias, if present
- Treatment of any infections
- Heart failure
In patients whose valves have been removed, repeat echocardiography is indicated at 6-month intervals. In patients whose valve has been replaced, annual echocardiography is recommended.
Consultations
Consultations that may be needed to evaluate tricuspid regurgitation include the following:
- Cardiologist for evaluation and medical management
- Cardiac surgeon if the patient is symptomatic and may need surgical evaluation or management
- Cardiac anesthesia consults for preoperative monitoring and management
Deterrence and Patient Education
Here are some key points to discuss with patients about tricuspid regurgitation:
Types: Tricuspid regurgitation comes in 3 forms, and the severity of the condition influences the symptoms and the necessary treatment.
Symptoms: While mild tricuspid regurgitation often presents no symptoms, moderate to severe cases can lead to leg swelling, difficulty breathing, irregular heartbeats, and chest pain.
Causes: The most common cause of tricuspid regurgitation is an enlargement of the right ventricle, which can result from various underlying conditions.
Treatment: Treatment options for tricuspid regurgitation include medications and potentially surgery, depending on the severity.
Lifestyle changes: To manage the condition, it is recommended that people adopt lifestyle changes, such as following a heart-healthy diet, avoiding smoking, and engaging in regular exercise.
Dental care: Patients with heart valve disease should maintain good oral hygiene and visit the dentist every 3 months. Antibiotics may be necessary before dental procedures to prevent endocarditis.
Strep throat: Individuals with heart valve disease must seek medical attention promptly if they suspect they have strep throat.
Atrial fibrillation: People with tricuspid regurgitation may develop an irregular heartbeat, which increases the risk of blood clot formation.
Pearls and Other Issues
TR remains significantly undertreated surgically and is often diagnosed late, typically in patients presenting with right-sided heart failure.
TR detection and management: Accurate detection, quantification, categorization, risk assessment, monitoring of interventions, and evaluation of outcomes—especially regarding right-sided heart function—are essential for effective patient management and developing clinical trials for interventional and surgical approaches.
Standardized care protocols: It is crucial to implement standardized definitions of TR causes and mechanisms and consistently use quantitative methods for measuring TR. Moving beyond basic assessments of cardiac remodeling and right ventricular function, using cardiac computed tomography and magnetic resonance imaging for precise quantification is a critical step, necessitating the establishment of rigorous protocols for routine clinical practice.
Enhancing Healthcare Team Outcomes
The diagnosis and management of tricuspid regurgitation involve an interprofessional team consisting of a cardiologist, cardiac surgeon, internist, primary care provider, and nurse practitioner. Treatment preference depends on the severity of tricuspid regurgitation, its etiology, and the presence and extent of associated abnormalities, including pulmonary hypertension, heart failure, and other valve conditions.
Managing severe tricuspid regurgitation includes medical therapy, counseling regarding pregnancy and physical activity, consideration of tricuspid valve surgery, and evaluation and treatment of the underlying causes. Mild cases are usually managed medically, but severe cases require open heart surgery. The tricuspid valve can be repaired or replaced depending on the status of the leaflets. Because of the risk of thrombosis, all mechanical valves in the tricuspid position need anticoagulation, and patients will need to be monitored for international normalized ratio regularly. The outcomes of tricuspid regurgitation are usually fair to good.[36]
Media
(Click Image to Enlarge)
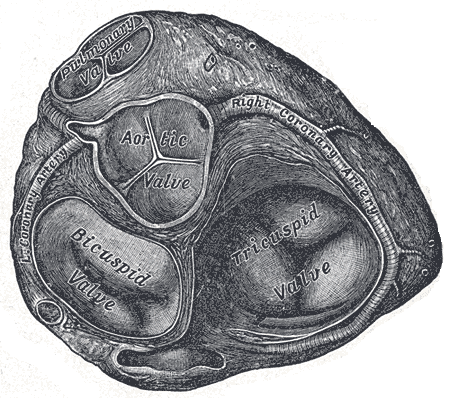
Valves of the Heart. The bicuspid valve, aortic valve, pulmonary valve, tricuspid valve, and right coronary artery are illustrated.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Video to Play)
Tricuspid Valve Doppler. A transthoracic echocardiogram shows the color Doppler across the tricuspid valve.
Contributed by Pirbhat Shams, MBBS
References
Wafae N, Hayashi H, Gerola LR, Vieira MC. Anatomical study of the human tricuspid valve. Surgical and radiologic anatomy : SRA. 1990:12(1):37-41 [PubMed PMID: 2345895]
Rogers JH, Bolling SF. The tricuspid valve: current perspective and evolving management of tricuspid regurgitation. Circulation. 2009 May 26:119(20):2718-25. doi: 10.1161/CIRCULATIONAHA.108.842773. Epub [PubMed PMID: 19470900]
Level 3 (low-level) evidenceAntunes MJ, Rodríguez-Palomares J, Prendergast B, De Bonis M, Rosenhek R, Al-Attar N, Barili F, Casselman F, Folliguet T, Iung B, Lancellotti P, Muneretto C, Obadia JF, Pierard L, Suwalski P, Zamorano P, ESC Working Groups of Cardiovascular Surgery and Valvular Heart Disease. Management of tricuspid valve regurgitation: Position statement of the European Society of Cardiology Working Groups of Cardiovascular Surgery and Valvular Heart Disease. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2017 Dec 1:52(6):1022-1030. doi: 10.1093/ejcts/ezx279. Epub [PubMed PMID: 28950325]
Aktas EO, Govsa F, Kocak A, Boydak B, Yavuz IC. Variations in the papillary muscles of normal tricuspid valve and their clinical relevance in medicolegal autopsies. Saudi medical journal. 2004 Sep:25(9):1176-85 [PubMed PMID: 15448762]
Xanthos T, Dalivigkas I, Ekmektzoglou KA. Anatomic variations of the cardiac valves and papillary muscles of the right heart. Italian journal of anatomy and embryology = Archivio italiano di anatomia ed embriologia. 2011:116(2):111-26 [PubMed PMID: 22303639]
Nath J, Foster E, Heidenreich PA. Impact of tricuspid regurgitation on long-term survival. Journal of the American College of Cardiology. 2004 Feb 4:43(3):405-9 [PubMed PMID: 15013122]
Level 2 (mid-level) evidenceMutlak D, Lessick J, Reisner SA, Aronson D, Dabbah S, Agmon Y. Echocardiography-based spectrum of severe tricuspid regurgitation: the frequency of apparently idiopathic tricuspid regurgitation. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2007 Apr:20(4):405-8 [PubMed PMID: 17400120]
Tornos Mas P, Rodríguez-Palomares JF, Antunes MJ. Secondary tricuspid valve regurgitation: a forgotten entity. Heart (British Cardiac Society). 2015 Nov:101(22):1840-8. doi: 10.1136/heartjnl-2014-307252. Epub [PubMed PMID: 26503944]
Sagie A, Schwammenthal E, Padial LR, Vazquez de Prada JA, Weyman AE, Levine RA. Determinants of functional tricuspid regurgitation in incomplete tricuspid valve closure: Doppler color flow study of 109 patients. Journal of the American College of Cardiology. 1994 Aug:24(2):446-53 [PubMed PMID: 8034882]
Level 2 (mid-level) evidenceNavia JL, Elgharably H, Javadikasgari H, Ibrahim A, Koprivanac M, Lowry AM, Blackstone EH, Klein AL, Gillinov AM, Roselli EE, Svensson LG. Tricuspid Regurgitation Associated With Ischemic Mitral Regurgitation: Characterization, Evolution After Mitral Surgery, and Value of Tricuspid Repair. The Annals of thoracic surgery. 2017 Aug:104(2):501-509. doi: 10.1016/j.athoracsur.2016.11.024. Epub 2017 Feb 21 [PubMed PMID: 28223050]
Zoghbi WA, Adams D, Bonow RO, Enriquez-Sarano M, Foster E, Grayburn PA, Hahn RT, Han Y, Hung J, Lang RM, Little SH, Shah DJ, Shernan S, Thavendiranathan P, Thomas JD, Weissman NJ. Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2017 Apr:30(4):303-371. doi: 10.1016/j.echo.2017.01.007. Epub 2017 Mar 14 [PubMed PMID: 28314623]
Simula DV, Edwards WD, Tazelaar HD, Connolly HM, Schaff HV. Surgical pathology of carcinoid heart disease: a study of 139 valves from 75 patients spanning 20 years. Mayo Clinic proceedings. 2002 Feb:77(2):139-47 [PubMed PMID: 11838647]
Level 2 (mid-level) evidencePritchett AM, Morrison JF, Edwards WD, Schaff HV, Connolly HM, Espinosa RE. Valvular heart disease in patients taking pergolide. Mayo Clinic proceedings. 2002 Dec:77(12):1280-6 [PubMed PMID: 12479512]
Level 3 (low-level) evidenceBaseman DG, O'Suilleabhain PE, Reimold SC, Laskar SR, Baseman JG, Dewey RB Jr. Pergolide use in Parkinson disease is associated with cardiac valve regurgitation. Neurology. 2004 Jul 27:63(2):301-4 [PubMed PMID: 15277624]
Level 3 (low-level) evidenceWaller BF, Howard J, Fess S. Pathology of tricuspid valve stenosis and pure tricuspid regurgitation--Part III. Clinical cardiology. 1995 Apr:18(4):225-30 [PubMed PMID: 7788951]
Vieitez JM, Monteagudo JM, Mahia P, Perez L, Lopez T, Marco I, Perone F, González T, Sitges M, Bouzas A, González-Salvado V, Li CH, Alonso D, Carrasco F, Adeba A, de la Hera JM, Fernandez-Golfin C, Zamorano JL. New insights of tricuspid regurgitation: a large-scale prospective cohort study. European heart journal. Cardiovascular Imaging. 2021 Jan 22:22(2):196-202. doi: 10.1093/ehjci/jeaa205. Epub [PubMed PMID: 32783057]
Adamo M, Chioncel O, Benson L, Shahim B, Crespo-Leiro MG, Anker SD, Coats AJS, Filippatos G, Lainscak M, McDonagh T, Mebazaa A, Piepoli MF, Rosano GMC, Ruschitzka F, Savarese G, Seferovic P, Shahim A, Popescu BA, Iung B, Volterrani M, Maggioni AP, Metra M, Lund LH. Prevalence, clinical characteristics and outcomes of heart failure patients with or without isolated or combined mitral and tricuspid regurgitation: An analysis from the ESC-HFA Heart Failure Long-Term Registry. European journal of heart failure. 2023 Jul:25(7):1061-1071. doi: 10.1002/ejhf.2929. Epub 2023 Jun 26 [PubMed PMID: 37365841]
De la Espriella R, Santas E, Chorro FJ, Miñana G, Soler M, Bodí V, Valero E, Núñez E, Bayés-Genis A, Lupón J, Sanchis J, Núñez J. Functional tricuspid regurgitation and recurrent admissions in patients with acute heart failure. International journal of cardiology. 2019 Sep 15:291():83-88. doi: 10.1016/j.ijcard.2019.03.051. Epub 2019 Mar 27 [PubMed PMID: 30955879]
Wang TKM, Akyuz K, Mentias A, Kirincich J, Duran Crane A, Xu S, Popovic ZB, Xu B, Gillinov AM, Pettersson GB, Griffin BP, Desai MY. Contemporary Etiologies, Outcomes, and Novel Risk Score for Isolated Tricuspid Regurgitation. JACC. Cardiovascular imaging. 2022 May:15(5):731-744. doi: 10.1016/j.jcmg.2021.10.015. Epub 2021 Dec 15 [PubMed PMID: 34922866]
Iglesias-Garriz I, Olalla-Gómez C, Garrote C, López-Benito M, Martín J, Alonso D, Rodríguez MA. Contribution of right ventricular dysfunction to heart failure mortality: a meta-analysis. Reviews in cardiovascular medicine. 2012:13(2-3):e62-9. doi: 10.3909/ricm0602. Epub [PubMed PMID: 23160163]
Level 1 (high-level) evidenceDietz MF, Prihadi EA, van der Bijl P, Ajmone Marsan N, Delgado V, Bax JJ. Prognostic Implications of Staging Right Heart Failure in Patients With Significant Secondary Tricuspid Regurgitation. JACC. Heart failure. 2020 Aug:8(8):627-636. doi: 10.1016/j.jchf.2020.02.008. Epub 2020 Jun 10 [PubMed PMID: 32535118]
Frater R. Tricuspid insufficiency. The Journal of thoracic and cardiovascular surgery. 2001 Sep:122(3):427-9 [PubMed PMID: 11547290]
Topilsky Y, Tribouilloy C, Michelena HI, Pislaru S, Mahoney DW, Enriquez-Sarano M. Pathophysiology of tricuspid regurgitation: quantitative Doppler echocardiographic assessment of respiratory dependence. Circulation. 2010 Oct 12:122(15):1505-13. doi: 10.1161/CIRCULATIONAHA.110.941310. Epub 2010 Sep 27 [PubMed PMID: 20876436]
Level 2 (mid-level) evidenceCarpentier A. Cardiac valve surgery--the "French correction". The Journal of thoracic and cardiovascular surgery. 1983 Sep:86(3):323-37 [PubMed PMID: 6887954]
Ha JW, Chung N, Jang Y, Rim SJ. Tricuspid stenosis and regurgitation: Doppler and color flow echocardiography and cardiac catheterization findings. Clinical cardiology. 2000 Jan:23(1):51-2 [PubMed PMID: 10680030]
Level 3 (low-level) evidenceShah PM, Raney AA. Tricuspid valve disease. Current problems in cardiology. 2008 Feb:33(2):47-84. doi: 10.1016/j.cpcardiol.2007.10.004. Epub [PubMed PMID: 18222317]
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O'Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A, Toly C. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2:143(5):e72-e227. doi: 10.1161/CIR.0000000000000923. Epub 2020 Dec 17 [PubMed PMID: 33332150]
Level 1 (high-level) evidenceDreyfus J, Komar M, Attias D, De Bonis M, Ruschitzka F, Popescu BA, Laroche C, Tribouilloy C, Bogachev Prokophiev A, Mizariene V, Bax JJ, Maggioni AP, Messika-Zeitoun D, Vahanian A, Iung B, EORP VHD II Registry Investigators Group. Tricuspid regurgitation: Frequency, clinical presentation, management and outcome among patients with severe left-sided valvular heart disease in Europe. Insights from the ESC-EORP Valvular Heart Disease II survey. European journal of heart failure. 2024 Apr:26(4):994-1003. doi: 10.1002/ejhf.3157. Epub 2024 Feb 19 [PubMed PMID: 38374610]
Level 3 (low-level) evidenceBaumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Muñoz D, Rosenhek R, Sjögren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL, ESC Scientific Document Group. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. European heart journal. 2017 Sep 21:38(36):2739-2791. doi: 10.1093/eurheartj/ehx391. Epub [PubMed PMID: 28886619]
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Fleisher LA, Jneid H, Mack MJ, McLeod CJ, O'Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017 Jun 20:135(25):e1159-e1195. doi: 10.1161/CIR.0000000000000503. Epub 2017 Mar 15 [PubMed PMID: 28298458]
Level 1 (high-level) evidenceNishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O'Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD, American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014 Jun 10:63(22):e57-185. doi: 10.1016/j.jacc.2014.02.536. Epub 2014 Mar 3 [PubMed PMID: 24603191]
Level 1 (high-level) evidenceJoint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC), European Association for Cardio-Thoracic Surgery (EACTS), Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, Borger MA, Carrel TP, De Bonis M, Evangelista A, Falk V, Iung B, Lancellotti P, Pierard L, Price S, Schäfers HJ, Schuler G, Stepinska J, Swedberg K, Takkenberg J, Von Oppell UO, Windecker S, Zamorano JL, Zembala M. Guidelines on the management of valvular heart disease (version 2012). European heart journal. 2012 Oct:33(19):2451-96. doi: 10.1093/eurheartj/ehs109. Epub 2012 Aug 24 [PubMed PMID: 22922415]
Chorin E, Rozenbaum Z, Topilsky Y, Konigstein M, Ziv-Baran T, Richert E, Keren G, Banai S. Tricuspid regurgitation and long-term clinical outcomes. European heart journal. Cardiovascular Imaging. 2020 Feb 1:21(2):157-165. doi: 10.1093/ehjci/jez216. Epub [PubMed PMID: 31544933]
Level 2 (mid-level) evidenceDreyfus J, Flagiello M, Bazire B, Eggenspieler F, Viau F, Riant E, Mbaki Y, Bohbot Y, Eyharts D, Senage T, Dubrulle H, Nicol M, Doguet F, Nguyen V, Coisne A, Le Tourneau T, Lavie-Badie Y, Tribouilloy C, Donal E, Tomasi J, Habib G, Selton-Suty C, Raffoul R, Iung B, Obadia JF, Messika-Zeitoun D. Isolated tricuspid valve surgery: impact of aetiology and clinical presentation on outcomes. European heart journal. 2020 Dec 1:41(45):4304-4317. doi: 10.1093/eurheartj/ehaa643. Epub [PubMed PMID: 32974668]
Hahn RT, Meduri CU, Davidson CJ, Lim S, Nazif TM, Ricciardi MJ, Rajagopal V, Ailawadi G, Vannan MA, Thomas JD, Fowler D, Rich S, Martin R, Ong G, Groothuis A, Kodali S. Early Feasibility Study of a Transcatheter Tricuspid Valve Annuloplasty: SCOUT Trial 30-Day Results. Journal of the American College of Cardiology. 2017 Apr 11:69(14):1795-1806. doi: 10.1016/j.jacc.2017.01.054. Epub [PubMed PMID: 28385308]
Level 2 (mid-level) evidenceZhang FE, Li JY, Bo P, Zhang JQ, Ren T, Cao XR. [Midterm outcomes of surgical treatment of traumatic severe tricuspid insufficiency]. Zhonghua wai ke za zhi [Chinese journal of surgery]. 2019 Feb 1:57(2):134-138. doi: 10.3760/cma.j.issn.0529-5815.2019.02.012. Epub [PubMed PMID: 30704218]