Introduction
Restenosis is the reduction in the diameter of the vessel lumen after angioplasty. Despite advances in stent technology, restenosis continues to be the most frequent cause of target lesion failure following percutaneous coronary intervention (PCI). Following the introduction of bare-metal stents (BMS) in the mid-1990s for the treatment of coronary artery disease, a new clinical entity emerged called in-stent restenosis (ISR), which is restenosis in an implanted coronary stent. Angiographically, ISR is more than 50% stenosis within or immediately adjacent to a previously stented region. Clinical restenosis occurs when there is a recurrence of clinical manifestations of ischemia in the setting of ISR, often requiring a repeat revascularization procedure. In-segment restenosis is often defined as restenosis anywhere between 5 mm from the proximal and distal edges of the stent.[1] Recurrent in-stent restenosis is defined as the failure of at least two revascularization procedures at the stent segment.[2]
In plain-old balloon (no-stent) angioplasty (POBA), mechanisms of restenosis involve vessel remodeling and elastic recoil. In contrast, restenosis in-stent angioplasty involves excessive tissue proliferation called neointimal proliferation, or by a new atherosclerotic process called neoatherosclerosis.[3] The patterns of in-stent restenosis have been described as either diffuse (lesion over 10 mm in length) or focal (lesion less than 10 mm in length) according to the Mehran classification criteria.[4] Clinically, coronary vessel restenosis will present as recurrence of angina or acute coronary syndrome. ISR is associated with significant morbidity. In a prospective cohort study of 10004 patients who underwent routine control angiography 6 to 8 months after coronary stenting, the presence of restenosis at follow-up angiography was predictive of 4-year mortality.[5][4]
Efforts to reduce the incidence of restenosis and treatment options for in-stent restenosis have evolved remarkably over the last two decades. Advancement in the stent platforms (e.g. thin-strut, and biodegradable), eluting drugs (biolimus A9 and zotarolimus, designed specifically for intracoronary use), and intravascular imaging modalities improving implant technique has led the interventional cardiologist to treat patients who were previously limited to surgical revascularization (i.e. left main stem, multivessel disease, complex bifurcations and complex and severely calcified lesions). As a result, real-world registries, including more complex patients and lesions, show a higher rate of ISR when compared to the reports from randomized trials.[3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
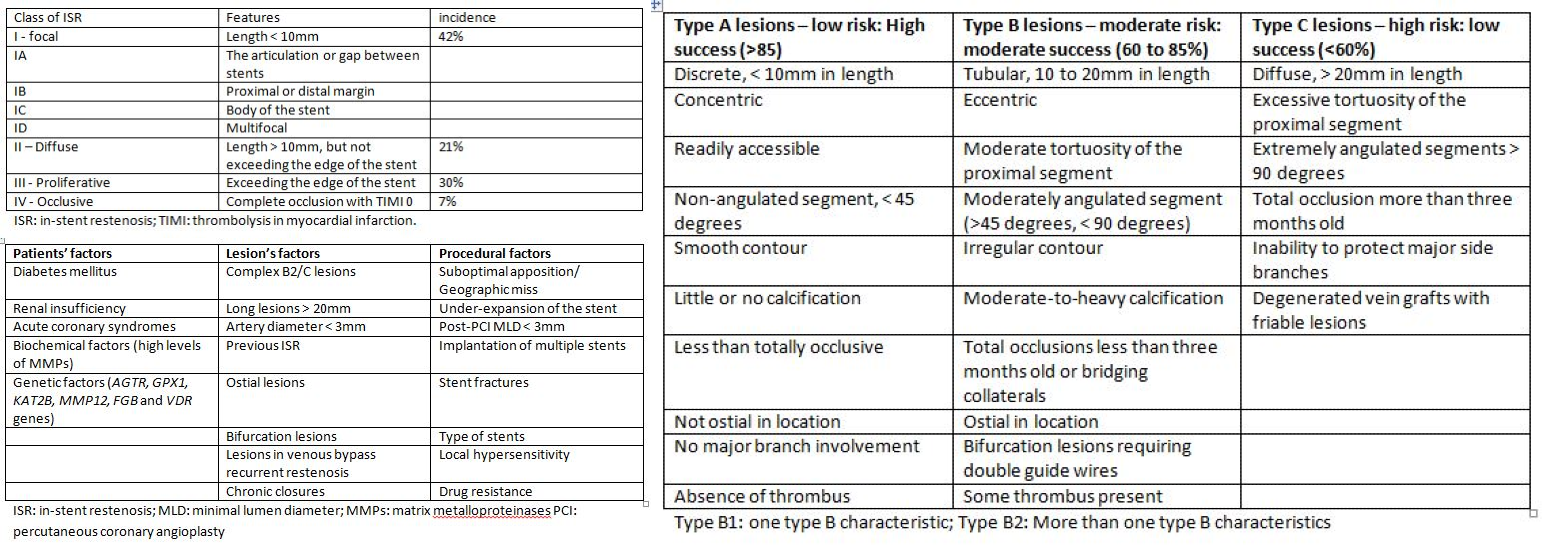
Risk factors for restenosis are classified based on patient features, lesion type, and procedural factors (Table 1). Biological factors associated with an increased risk of restenosis include diabetes mellitus and renal insufficiency. In a multivariate regression analysis, diabetes mellitus in itself increases the risk of BMS-ISR by 30% to 50%.[1] Likewise, the risk of drug-eluting stent ISR (DES-ISR) is increased in diabetic patients when compared to those without diabetes.
Biochemical factors such as elevated serum matrix metalloproteinases (MMPs), the proteolytic enzymes that degrade the extracellular matrix (ECM), and facilitate the proliferation and migration of endothelial and vascular smooth muscle cells, has been associated with a higher risk of ISR. Hematological indices, including neutrophil/lymphocyte ratio, platelet/lymphocyte ratio, red blood cell distribution width, mean platelet volume, and platelet distribution width, have been hypothesized in some studies to predict the occurrence of increased risk for DES-ISR.[6] The GENetic DEterminants of Restenosis (GENDER) study identified single-nucleotide polymorphisms (SNPs) in AGTR, GPX1, KAT2B, MMP12, FGB, and VDR genes as being associated with an increased risk of restenosis.[7] Significant mechanical predictors of restenosis include complex lesions ACC/AHA Type B2/C (B2 and C lesions are not only more frequently related to suboptimal acute results but also with a higher restenosis rate and poorer long-term clinical outcomes),[2] the length of the lesion and small vessel diameter. A stent length greater than 35 mm correlates with nearly double the ISR risk compared to less than 20 mm stents. The major risk factors for recurrent ISR are diabetes mellitus, and previous ISR, and type according to Mehran's classification (with an increase from I to IV).[2][4]
Procedural risk factors
The most known and preventable cause for ISR is stent under-expansion. Stent under-expansion can be due to stent under-sizing, low-pressure deployment, inadequate vessel preparation, or extensive vessel calcification leading to an under-expanded stent. However, under-sizing is not the only risk factor for ISR. Failure to stent from healthy segment to healthy segment, or geographic miss, is another common risk factor. Geographic miss appears as a characteristic “candy-wrapper” appearance at the edge of a stented segment. Additionally, stent fracture is another possible mechanical precipitant for ISR. Finally, the development and use of DES has led to the recognition of drug resistance and local hypersensitivity reactions as a potential cause of ISR and DES failure.[8][9]
Epidemiology
Several different factors and variables often confound efforts to determine the precise incidence of restenosis. In the pre-stent era, the incidence of restenosis ranged between 32 and 55% of all angioplasties. This figure dropped to 17 to 41% in the BMS era.[3] The advent of DES has led to a further reduction in the incidence of restenosis to numbers under 10%.[1]
The ISR rate is often higher in the setting of multivessel disease compared with single-vessel disease, as demonstrated in the study of Zhao et al; the occurrence of ISR was significantly higher in patients with two-vessel (OR: 2.922; 95% CI: 1.266–6.745; P=0.012) or three-vessel disease (OR: 2.574; 95% CI: 1.128–5.872; P=0.025) when compared with those with one-vessel disease.[10][3] In a separate study with angiographic follow-up of 10004 patients who had stenting, implantation of first-generation DES versus BMS (OR 0.35, 95% CI 0.31 to 0.39), and second-generation DES versus first-generation DES (OR 0.67, 95% CI 0.58 to 0.77) were found to be independent predictors of lower rates of restenosis.[11] Multivariate analysis identified small vessel size, total stent length, complex lesion morphology, presence of diabetes mellitus, and history of bypass surgery as independent predictors of worse restenosis outcomes, and these were similar across the spectrum of stent devices.[11]
ISR is an important predictor for future restenosis, and these lesions pose numerous challenges for successful PCI. In the ICARUS Cooperation study, a total of 546 patients treated with drug-coated balloon (DCB) angioplasty for drug-eluting stent (DES) restenosis had followup with angiography at 6 to 9 months. Researchers observed recurrent restenosis in 101 (20.8%) patients. Likewise, on multivariate analysis, increased lesion length, and reduced vessel size were independently associated with recurrent restenosis.[12]
Pathophysiology
Restenosis may occur as a result of an excessive reaction to the vascular injury sustained from the PCI. The first vascular response following the trauma of PCI includes elastic recoil, platelet plug, and thrombus formation, occurring in the initial minutes and hours following intervention. This initial response is followed by a complex inflammatory and reparative process that lasts weeks to months or even years in the case of DES-ISR. The acute phase is characterized by the deposition of platelets and fibrin, with the adhesion of circulating neutrophils and monocytes. Over weeks, chronic inflammatory cells (macrophages and giant cells) will gradually replace the acute inflammatory cells at the site of vascular injury. These processes occur over a relatively short period (weeks to months), unlike the slow progression (years) of atherosclerotic disease in native coronary lesions. The two principal biologic mechanisms of ISR are neointimal hyperplasia and neoatherosclerosis.[13]
Neointimal hyperplasia is a reparative process whereby various coagulation and inflammatory factors and cells stimulate vascular smooth muscle cell (VSMC) proliferation and extracellular matrix (ECM) formation at the site of injury. In addition to initial inflammatory response, platelet- and leukocyte-related growth factors stimulate further VSMC proliferation and migration from the media to the inceptive neointima with the formation of ECM. At about two weeks after stent implantation, a neointimal layer, composed of VSMCs and a proteoglycan-rich ECM are visible above the stent struts. Subsequently, endothelial cells proliferate and cover the ECM from the luminal side.
A diffuse pattern of ISR, characterized by a predominance of VSMCs surrounded by lesser amount ECM, is typical of BMS-ISR. Peak BMS-ISR is observed at 3 to 6 months and remains relatively stable beyond one year. DES implantation, on the other hand, enables the local release of antiproliferative agents [paclitaxel or “-limus” drug group (sirolimus, everolimus, zotarolimus, biolimus, etc)] resulting in delayed vessel wall healing, characterized by the presence of chronic fibrin deposits, incomplete neoendothelization, and prolonged inflammatory changes that persist for up to 48 months. This process prevents excessive neointimal hyperplasia after DES stent implantation and leads to a reduction in the occurrence of ISR.[1]
Neoatherosclerosis, on the other hand, is related to incomplete regeneration of the endothelium leading to excessive uptake of circulating lipids and accelerated development of atherosclerotic plaques in the nascent neointima. Intimal thickening, intracellular lipid deposition with thin-cap fibroatheroma (TCFA), or the presence of necrotic tissue has been detected using histopathological or optical coherence tomography (OCT) evaluations. Nakazawa, et al. found in their histopathological autopsy study that neoatherosclerosis as a result of persistent endothelial dysfunction and incomplete neoendothelization occurs more frequently (31% vs. 16%; P < 0.001) and earlier (median: 420 vs. 2160 days; P < 0.001) following DES than BMS implantation.
Moreover, neoatherosclerosis in DES shows unstable characteristics (TCFA or plaque rupture) earlier (about two years) after implantation, whereas similar features in BMS occur relatively later (about six years). Independent predictors of neoatherosclerosis include younger age, longer implant durations, sirolimus- or paclitaxel-eluting stent implantation, smoking, chronic kidney disease, and LDL-cholesterol greater than 3.9 mmol/l. The belief is that neoatherosclerosis, along with the rupturing of the TCFA, are among the predominant causes of late stent failure (i.e., delayed ISR and late or very late stent thrombosis).[14][1] Examination of 299 patients post-mortem revealed that, compared to BMS, DES had almost twice the rate of neoatherosclerosis (31% vs. 16 %, p < 0.001).[15]
History and Physical
Restenosis presents with a wide spectrum of clinical features that depict varying levels of cardiac ischemia in the setting of previous coronary intervention. The clinical features of restenosis depend on the individual patient and lesion characteristics, as well as the anatomic location. They may present as stable angina, unstable angina (26 to 53 % for BMS, 16 to 66 % for DES), or acute myocardial infarction (MI) (3.5 to 20 % for BMS, 1 to 20 % for DES).[15] The Mehran's classification of ISR is a predictor of clinical outcome based on BMS-ISR, with the necessity of repeated target vessel revascularization being 19% for group I, 35% for group II, 50% for group III and 83% for group IV (P < 0.001).[1] Depending on the duration since the deployment of the stent, ISR can also be classified as acute (within 24 hours), subacute (from 24 hours to 30 days), late (30 days to 1 year), and very late (>1 year).[8]
In a study of 909 patients who had ISR after BMS, first-generation DES, or second-generation DES, the clinical presentation was acute coronary syndrome in 67.8%, 71.0%, and 66.7% of patients, respectively (P=0.470). In contrast, myocardial infarction occurred in 10.6%, 10.1%, and 5.2% of patients, respectively (P=0.273). These are not statistically significant and may suggest that patient and lesion characteristics, rather than the specific initial device deployed, are the major determinants of the clinical presentation of ISR.[16] Current smoking status and chronic renal failure were found to correlate with presentation of MI (odds ratio, 3.02; 95% confidence interval [CI], 1.78-5.13; P<0.001), and (odds ratio, 2.73; 95% CI, 1.60-4.70; P<0.001), respectively; while second-generation DES-ISR was attributed to be protective for a presentation with MI (odds ratio, 0.35; 95% CI, 0.12-1.03; P=0.060).[16]
Evaluation
Coronary angiography historically has been a well established diagnostic modality for identifying restenosis and for the guidance of PCI. In a study of 288 BMS-ISR lesions in 245 patients, Mehran and colleagues classified ISR into four angiographic patterns (Table 2 and 3). Pattern I: focal (length of 10 mm or less) lesions; pattern II: ISR involving more than 10 mm within the stent; pattern III: ISR more than 10 mm and extending outside the stent; and pattern IV is a completely occlusive ISR. The incidence was 42%, 21%, 30%, and 7% for pattern I, pattern II, pattern III, and pattern IV, respectively.[4] Table 3 highlight the lesion-specific characteristics and their corresponding outcomes with balloon angioplasty.
Intravascular imaging techniques, including intravascular ultrasound (IVUS) and optical coherence tomography (OCT), provide additional advantages over angiography, providing more distinct lesion characterization and identification of the etiology of ISR potentially optimizing the short and long term outcomes of PCI for ISR.[17][18] [19]
Intravascular imaging with IVUS or OCT determination of the potential mechanisms of ISR can guide appropriate treatment. Both imaging modalities can identify stent under-expansion, presence of neointimal hyperplasia, and borders of the external elastic lamina for appropriate balloon sizing during post-dilation. OCT has a superior axial resolution, and can further highlight the morphologic differences between BMS-ISR and DES-ISR. Findings of homogenous, continuous tissue bands on OCT are consistent with neointimal hyperplasia that is typical of BMS-ISR, while a focal, heterogeneous, and layering appearance represents proteoglycan and fibrin deposition which occurs in the setting of neoatherosclerosis. Other specific findings that are suggestive of neoatherosclerosis include neointimal rupture, TCFA formation, microvessels, presence of lipid pools, macrophage accumulation, and evidence of non-occlusive thrombosis.[8][20]
In a meta-analysis of thirteen studies with 1384 stents on double source computed tomography angiography (DSCTA) and five studies including 622 stents on 320-row computed tomography angiography (320-row CTA), the sensitivity, the specificity, and the area under the curve of DSCTA in diagnosing ISR were 0.92 (0.87 to 0.96), 0.91 (0.87 to 0.94), and 0.97 (0.95 to 0.98), respectively, and they were 0.91 (0.82 to 0.96), 0.95 (0.88 to 0.98), and 0.96 (0.94 to 0.97) for 320-row CTA. This data suggested that both DSCTA and 320-row CTA had high diagnostic accuracy in detecting ISR, especially for stent diameters of more than 3 mm, and may be appropriate tools for further evaluation of ISR in the future.[21][22]
Newer data fusion methodologies and hybrid, dual-probe catheters are being developed to allow complete and detailed evaluation of plaque morphology and pathophysiology, and for reliable identification of high-risk and vulnerable lesions. Examples of these dual-probe catheters are combined IVUS-OCT,near-infrared spectroscopy (NIRS)-IVUS, OCT-NIRS, OCT-near infrared fluorescence (NIRF) molecular imaging (IVUS-NIRF), IVUS intravascular photoacoustic imaging, and combined fluorescence lifetime-IVUS imaging. These multimodal approaches can provide a comprehensive visualization of plaque composition and plaque morphology and are useful for guiding optimal intervention decisions.[23]
Several studies have indicated that asymptomatic patients with moderate disease severity ISR are unlikely to benefit from routine reintervention. Assessment of fractional flow reserve (FFR) during cardiac catheterization can assist in determining those that will benefit from revascularization. Prospective studies have shown that deferring revascularization in patients with ISR and FFR of over 0.75 is safe and appropriate.[24][8][25]
Treatment / Management
There are numerous treatment modalities available for the treatment of ISR, and treatment often involves more than one technique. The optimal therapy is individualized for each case of ISR and often based on the etiology of ISR and patient and lesion characteristics. Intravascular imaging allows for the identification of the mechanism of ISR and appropriate tailoring of treatment.
Medical therapy: Secondary prophylaxis with aspirin and statins in persons who have had PCI for coronary artery disease should follow current guideline recommendations. However, large clinical trials have not shown any medication with demonstrated efficacy in halting the progression of established ISR. Evidence for drug therapy in treating ISR is limited. Antiplatelet agents are used as per current guideline recommendations but are ineffective for specifically treating ISR. Despite the initial promise, larger trials looking at the use of abciximab to prevent ISR recurrence did not suggest a clinical benefit. Limited evidence also suggests that oral sirolimus, when given before reintervention, may prevent repeat ISR. However, the lack of long-term outcomes and the drug side-effect profile have shown sirolimus to be a poor option for the treatment of ISR.[8][24]
POBA: Plain old balloon angioplasty (POBA) historically has been one of the primary treatment modalities used in the management of ISR. POBA frequently results in an acceptable acute angiographic outcome. POBA is a particularly attractive option in focal areas of restenosis and when there is a documented evidence of stent/native artery size mismatch on intravascular imaging. Nevertheless, POBA is not without risk, and stent edge-related injuries and complications are always a concern whenever a stenotic site undergoes dilation. Balloon slippage is another element of POBA, which may not only prolong the procedure but can also lead to edge dissection and suboptimal outcomes. Incremental balloon upsizing as well as the use of short, low profile balloons, can help avoid balloon slippage and edge-related complications. Although the acute angiographic results may show significant improvement, tissue re-intrusion can occur within minutes of the final balloon inflation; this is one of the factors that contribute to ISR recurrence in up to 50% of patients treated with POBA.[8][26](A1)
Vascular Brachytherapy (VBT): Brachytherapy involves temporary intracoronary deposition of a radioactive isotope within the diseased segment. The goal of treatment is to suppress new tissue growth within areas of established ISR. This approach has demonstrated greater efficacy in halting ISR progression, as well as improving clinical outcomes than debulking techniques or POBA. The complexity of the procedure and issues with radioprotection/radiation dosing limited this technique to a few expert centers. Based on the findings of both the SISR (Sirolimus-Eluting Stents vs Vascular Brachytherapy for In-Stent Restenosis Within Bare-Metal Stents) and TAXUS V ISR (Paclitaxel-Eluting Stents vs Vascular Brachytherapy for In-Stent Restenosis Within Bare-Metal Stents) trials, DES was superior in decreasing restenosis rates and need for revascularization as compared to brachytherapy extending out to 5 years. Due in large part to the results of these two studies, vascular brachytherapy has been essentially abandoned for the management of BMS-ISR.[27][28] VBT, however, continues to play an important role in the treatment of DES ISR, especially in lesions with multiple layers of the stent.[29][30][31](A1)
Cutting and scoring balloons: These balloons work by incising neointimal tissue, thereby allowing for better balloon anchoring during angioplasty. The cutting or scoring action also helps to prep the lesion before balloon angioplasty to allow for better tissue extrusion. However, the largest randomized trial to date to compare cutting balloon angioplasty to POBA in the treatment of ISR, Restenosis Cutting Balloon Evaluation (RESCUT) Trial, failed to show improvement in angiographic stenosis or the rate of clinical events during its seven-month follow-up. Cutting balloon angioplasty correlated with a need to use fewer balloons, less additional stenting, and a lower rate of balloon slippage. The ISAR-DESIRE IV trial (Intracoronary Stenting and Angiographic Results: Optimizing Treatment of Drug-Eluting Stent In-Stent Restenosis 4) subsequently evaluated the use of scoring balloons before paclitaxel-coated balloon angioplasty for treatment of DES-ISR. The trial showed superior angiographic outcomes at six months in the scoring balloon arm but was underpowered to show any significant difference in clinical outcomes. At this time, there are no large randomized trials to show improvement in clinical outcomes with the use of either cutting or scoring balloons in the treatment of ISR. Their use may be a consideration in those situations where balloon migration is of particular concern as well as with the presence of significant tissue.[8][32][33](A1)
Rotational atherectomy and laser techniques: The development of debulking technologies such as rotational/directional atherectomy and excimer laser have allowed for a novel treatment approach to ISR through physical removal of neointimal tissue or neoatherosclerotic plaque. The technique involves the initial removal of excess stenotic tissue by the debulking device, followed by low-pressure balloon post-dilation. However, a subsequent multicenter randomized trial comparing POBA to rotational atherectomy revealed lower restenosis rates, improved safety profile, and superior clinical outcomes in the POBA arm. As a result of this study, debulking technology is not considered to be a routine part of ISR management. Instead, it is now a pretreatment option for heavily calcified lesions, which would otherwise compromise balloon expansion.[8]
Repeat stenting with BMS: Although stenting may improve the short-term angiographic appearance of ISR, two newly overlapping layers of stents (sandwich technique) with BMS may predispose to subsequent lumen loss. Patients with large vessel ISR (greater than 3 mm) and patients with stent edge disease had better angiographic and clinical outcomes when they received repeat BMS placement as opposed to POBA. To date, no large randomized trials have been performed to evaluate the role of BMS placement in DES-ISR, and BMS should not be used as a primary option.[34](A1)
Repeat Stenting with DES: Use of DES has thus become an attractive option in the treatment of neointimal hyperplasia seen in BMS-ISR. Indeed, several large scale studies, including ISAR-DESIRE (Intracoronary Stenting and Angiographic Results: Drug-Eluting Stents for In-Stent Restenosis) and RIBS-II (Balloon Angioplasty vs Elective Sirolimus-Eluting Stenting), have shown that the use of DES significantly decreased restenosis rates, reduced neointimal proliferation as seen on IVUS imaging, and improved clinical outcomes compared to balloon angioplasty. Some schools of thought have also suggested that using a stent with a different drug (hetero-DES approach) may help overcome the issue of drug resistance. The use of repeat stenting remains a common treatment strategy in the management of DES-ISR. However, current data suggest that 10 to 20% of these patients will go on to develop a recurrence of ISR. Innovative approaches, including the use of drug-coated balloons (DCB) and bioresorbable vascular scaffolds (BVS), continue to be developed to avoid the drawback of multiple layers of stent struts; referred to as “onion skinning effect.”[8][34][35] Despite the higher initial costs, recent meta-analyses have proved the cost-effectiveness of the second generation DES implantations. The cost-reduction in the long term was primarily due to the avoidance of secondary revascularisations and the absence of myocardial infarction.[36][34][8](A1)
Drug-coated balloons (DCB): The desire to deliver an anti-proliferative drug to the area of ISR without leaving behind an additional layer of the stent has led to the development of DCB. Although the data does not currently support the use of DCB over BMS or DES for newly diagnosed obstructive atherosclerotic coronary artery disease, the use of DCBs may have an important role in the management of both bare metal and drug-eluting ISR. Importantly, the overall non-inferior outcomes with DCB use as compared with DES placement supports the use of DCB for treatment of BMS-ISR, particularly in situations where it is preferable to avoid additional stent layering, or there are concerns for bleeding. The use of DCB for the management of DES-ISR has also been a topic of research. Similar to other treatment modalities, evidence suggests that DCB therapy is likely more effective for BMS-ISR than DES-ISR, highlighting the therapeutic challenges presented by DES-ISR.[37](A1)
As with BMS-ISR, initial data supporting the use of DCB in DES-ISR came from a small single-center study.[38] Subsequently, two large multicenter randomized trials have provided important comparative data for DCB use over both first and second-generation DES. The ISAR-DESIRE 3 (Efficacy Study of Paclitaxel-Eluting Balloon, Stent vs. Plain Angioplasty for Drug-Eluting Stent Restenosis) trial compared DCB therapy to both 1st generation DES and POBA. The results of the study revealed that DCB application was non-inferior to DES placement, and both were superior to POBA.[39] Perhaps the more clinically relevant study is the Restenosis Intra-stent of Drug-eluting Stents: Paclitaxel-Eluting Balloon vs. Everolimus-Eluting Stent (RIBS-IV) trial,[40] which compared second-generation everolimus-eluting stents to DCB angioplasty for treatment of DES-ISR. Second-generation DES showed better angiographic and clinical outcomes than DCB, thereby suggesting that in situations where there is no clear contraindication to repeat stenting, DES strategy may be the preferred option.[8](A1)
Bioresorbable Vascular scaffolds (BVS): The use of bioabsorbable scaffolds allows for the delivery of an anti-proliferative drug to the area of ISR similar to that seen in DCB angioplasty. Unlike DCB, however, the scaffold also prevents early lumen loss associated with tissue retraction seen in balloon angioplasty. Furthermore, unlike the traditional DES architecture, the bioabsorbable nature of the scaffold avoids permanent deposition of an additional layer of stent strut, potentially reducing the risk of restenosis. These characteristics make BVS an attractive option in the management of ISR. The minimal lumen diameter after BVS was comparable to that obtained with DCB (1.88 +/- 0.6 mm; p = NS) but smaller than that achieved after Everolimus-Eluting Stent (EES) (2.16 +/- 0.7 mm; p < 0.001). Similarly, target lesion revascularization rates after BVS were similar to those seen with DCB (10.4%) but higher than with EES (3.2%; p < 0.001). BVS obtained late angiographic and clinical results similar to DCB but inferior to EES.[41][42][43]
Comparing all treatment modalities: Treatment options for ISR are in constant evolution, and despite the large volume of published data on the various treatment modalities for ISR, it is difficult to determine which method is the gold standard as most studies compare one or at most two established modalities to the novel approach. Two recent large network meta-analyses have tried to clarify which strategy has the best evidence behind it.
Siontis et al. identified 27 trials with a total of 5923 patients.[44] The primary outcome of this meta-analysis was the percent diameter stenosis at the longest available follow-up (6 months to 1 year). Secondary endpoints included binary restenosis (presence or absence of stenosis), rates of target lesion revascularization, myocardial infarction, or death. ISR therapies included POBA, debulking techniques, brachytherapy, BMS, DES, and DCB. Repeat stenting with everolimus-eluting stents showed statistical superiority over other methods in the primary outcome, binary restenosis rates, and target lesion revascularization. DCB was the second most preferable approach but did not achieve a significant difference over sirolimus or paclitaxel-eluting stents.(A1)
Giacoppo et al. included 24 trials for a total of 4880 patients.[45] One clinical (target lesion revascularization) and one angiographic (late lumen loss) primary outcome were predefined for this analysis. The included ISR-therapies were similar to those evaluated by Siontis. Both DCB and DES showed superiority to other approaches based on the predefined clinical outcome, and in a head-to-head comparison, there was no significant difference. Angiographic outcomes again favored DCB or DES over all other modalities, however late tissue loss was slightly lower in the DCB arm when compared to DES. When compared to available options for treatments of coronary in-stent restenosis, second-generation drug-coated balloons, and drug-eluting stents were associated with superior angiographic and clinical outcomes, with similar comparative efficacy.[8][44](A1)
Differential Diagnosis
The recurrence of signs and symptoms of cardiac ischemia in a patient with a history of coronary artery disease and prior stent implantation could result from incomplete revascularization at the time of initial stent implantation, in-stent thrombosis, disease progression in other arterial territories, or restenosis. Patients with incomplete revascularization usually experience residual cardiac ischemic symptoms from the time of revascularization, and it may appear as a 'geographic miss' on repeat angiography. In-stent thrombosis will present as an acute event, resulting from sudden in-stent thrombus formation and acute occlusion. The pathogenesis of neoatherosclerosis after drug-eluting stent implantation carries associations with increased risk of late in-stent thrombosis. Most patients with coronary artery disease requiring revascularization have coexisting multivessel disease at varying levels of severity.
Prognosis
The advent of second-generation drug-eluting stents has dramatically improved the outcome of PCI, with an ISR rate of approximately 5 to 10%. Patients that follow exercise and diet cardiac rehabilitation programs are medically optimized and are compliant with appropriate dual antiplatelet therapy can help to minimize adverse events. The occurrence of clinical adverse events closely correlates with the final stent area, and maximizing the minimal stent area can help to mitigate adverse events.[46][47][48][49]
Complications
Complications of restenosis include stable angina, unstable angina, acute coronary syndrome, acute myocardial infarction, or death. Revascularization procedures for ISR could also encounter complications from access site bleeding, stent under-expansion, incomplete revascularization, coronary artery dissection, and stent thrombosis.
Deterrence and Patient Education
Although the use of the newer generation drug-eluting stents in the treatment of coronary stenosis with percutaneous coronary intervention has improved outcomes, the occurrence of ISR remains approximately 10%. The following conditions increase the risk of restenosis following stent implantation:
1. Uncontrolled diabetes mellitus
2. Continued cigarette smoking
3. High levels of LDL cholesterol
4. Uncontrolled hypertension
5. Renal insufficiency
These conditions should be adequately controlled and monitored. Smoking cessation, moderate exercise, and weight loss are advisable lifestyle interventions.
The metal of the stent scaffold can predispose to blood clot formation within the stent, with severe consequences. Dual antiplatelet therapy [DAPT], aspirin, and a second drug that prevents blood clot formation can help to prevent it, and adherence to DAPT must be per the instructions and duration of the treating cardiologist. Any interruption or cessation of DAPT should be with the approval of a cardiologist.
Enhancing Healthcare Team Outcomes
Historically, the decision-making process in the management of patients with coronary artery disease, including medical management, percutaneous coronary intervention, as well as referral for coronary artery bypass surgery, has been the sole responsibility of the cardiologist. The management of coronary restenosis is complex and challenging; research shows that an interprofessional heart team results in the best clinical outcomes. The heart team for coronary revascularization can include, the interventional cardiologist, the cardiovascular surgeon when necessary, intravascular imaging specialists, and the primary cardiologist. Some patients with complex lesions not suitable for percutaneous treatment will ultimately benefit from coronary artery bypass surgery, and the presence of a cardiovascular surgeon in the team will facilitate that decision when indicated.
Patients with coronary in-stent restenosis often have other co-morbidities, and broadening the interprofessional team to include appropriate sub-specialists such as the expertise of an endocrinologist for diabetes mellitus, a pulmonologist for pulmonary disorders, or a nephrologist for chronic kidney disease is imperative. Individualized optimization of patients in the peri-procedural period leads to improved outcomes. Registered nurses and radiologic technologists who possess highly specialized critical care and technical skills are essential components of the cardiac catheterization laboratory team. In the post-procedural period, the role of the nurse case managers and social workers in addressing the social circumstances that could preclude patients' compliance with medications and necessary lifestyle changes cannot be over-emphasized. Their management must be coordinated with the clinicians.
Nursing staff can assess for medication adherence (especially DAPT) and also monitor for adverse events associated with medication therapy, reporting concerns to the team. Pharmacists must perform medication reconciliation and verify dosing; they may also offer suggestions for which antiplatelet medication may be most effective, in conjunction with the treating vascular surgeon or cardiologist. Managing restenosis, or potential restenosis, to optimal outcomes is a collaborative interprofessional effort for the entire healthcare team. [Level 5]
Media
(Click Image to Enlarge)
References
Pleva L, Kukla P, Hlinomaz O. Treatment of coronary in-stent restenosis: a systematic review. Journal of geriatric cardiology : JGC. 2018 Feb:15(2):173-184. doi: 10.11909/j.issn.1671-5411.2018.02.007. Epub [PubMed PMID: 29662511]
Level 1 (high-level) evidencePiraino D, Cimino G, Buccheri D, Dendramis G, Andolina G, Cortese B. Recurrent in-stent restenosis, certainty of its origin, uncertainty about treatment. International journal of cardiology. 2017 Mar 1:230():91-96. doi: 10.1016/j.ijcard.2016.12.073. Epub 2016 Dec 22 [PubMed PMID: 28038808]
Buccheri D, Piraino D, Andolina G, Cortese B. Understanding and managing in-stent restenosis: a review of clinical data, from pathogenesis to treatment. Journal of thoracic disease. 2016 Oct:8(10):E1150-E1162 [PubMed PMID: 27867580]
Level 3 (low-level) evidenceMehran R, Dangas G, Abizaid AS, Mintz GS, Lansky AJ, Satler LF, Pichard AD, Kent KM, Stone GW, Leon MB. Angiographic patterns of in-stent restenosis: classification and implications for long-term outcome. Circulation. 1999 Nov 2:100(18):1872-8 [PubMed PMID: 10545431]
Level 2 (mid-level) evidenceCassese S, Byrne RA, Schulz S, Hoppman P, Kreutzer J, Feuchtenberger A, Ibrahim T, Ott I, Fusaro M, Schunkert H, Laugwitz KL, Kastrati A. Prognostic role of restenosis in 10 004 patients undergoing routine control angiography after coronary stenting. European heart journal. 2015 Jan 7:36(2):94-9. doi: 10.1093/eurheartj/ehu383. Epub 2014 Oct 8 [PubMed PMID: 25298237]
Wang Z, Liu C, Fang H. Blood Cell Parameters and Predicting Coronary In-Stent Restenosis. Angiology. 2019 Sep:70(8):711-718. doi: 10.1177/0003319719830495. Epub 2019 Feb 17 [PubMed PMID: 30773906]
Verschuren JJ, Trompet S, Postmus I, Sampietro ML, Heijmans BT, Houwing-Duistermaat JJ, Slagboom PE, Jukema JW. Systematic testing of literature reported genetic variation associated with coronary restenosis: results of the GENDER Study. PloS one. 2012:7(8):e42401. doi: 10.1371/journal.pone.0042401. Epub 2012 Aug 3 [PubMed PMID: 22879966]
Level 1 (high-level) evidenceNicolais C, Lakhter V, Virk HUH, Sardar P, Bavishi C, O'Murchu B, Chatterjee S. Therapeutic Options for In-Stent Restenosis. Current cardiology reports. 2018 Feb 12:20(2):7. doi: 10.1007/s11886-018-0952-4. Epub 2018 Feb 12 [PubMed PMID: 29435779]
Dangas GD, Claessen BE, Caixeta A, Sanidas EA, Mintz GS, Mehran R. In-stent restenosis in the drug-eluting stent era. Journal of the American College of Cardiology. 2010 Nov 30:56(23):1897-907. doi: 10.1016/j.jacc.2010.07.028. Epub [PubMed PMID: 21109112]
Zhao LP, Xu WT, Wang L, Li H, Shao CL, Gu HB, Chan SP, Xu HF, Yang XJ. Influence of insulin resistance on in-stent restenosis in patients undergoing coronary drug-eluting stent implantation after long-term angiographic follow-up. Coronary artery disease. 2015 Jan:26(1):5-10. doi: 10.1097/MCA.0000000000000170. Epub [PubMed PMID: 25211654]
Cassese S, Byrne RA, Tada T, Pinieck S, Joner M, Ibrahim T, King LA, Fusaro M, Laugwitz KL, Kastrati A. Incidence and predictors of restenosis after coronary stenting in 10 004 patients with surveillance angiography. Heart (British Cardiac Society). 2014 Jan:100(2):153-9. doi: 10.1136/heartjnl-2013-304933. Epub 2013 Nov 22 [PubMed PMID: 24270744]
Cassese S, Xu B, Habara S, Rittger H, Byrne RA, Waliszewski M, Pérez-Vizcayno MJ, Gao R, Kastrati A, Alfonso F. Incidence and predictors of reCurrent restenosis after drug-coated balloon Angioplasty for Restenosis of a drUg-eluting Stent: The ICARUS Cooperation. Revista espanola de cardiologia (English ed.). 2018 Aug:71(8):620-627. doi: 10.1016/j.rec.2017.08.005. Epub 2017 Sep 13 [PubMed PMID: 28916429]
Kim MS, Dean LS. In-stent restenosis. Cardiovascular therapeutics. 2011 Jun:29(3):190-8. doi: 10.1111/j.1755-5922.2010.00155.x. Epub 2010 Apr 9 [PubMed PMID: 20406239]
Nakazawa G, Otsuka F, Nakano M, Vorpahl M, Yazdani SK, Ladich E, Kolodgie FD, Finn AV, Virmani R. The pathology of neoatherosclerosis in human coronary implants bare-metal and drug-eluting stents. Journal of the American College of Cardiology. 2011 Mar 15:57(11):1314-22. doi: 10.1016/j.jacc.2011.01.011. Epub [PubMed PMID: 21376502]
Looser PM, Kim LK, Feldman DN. In-Stent Restenosis: Pathophysiology and Treatment. Current treatment options in cardiovascular medicine. 2016 Feb:18(2):10. doi: 10.1007/s11936-015-0433-7. Epub [PubMed PMID: 26781658]
Magalhaes MA, Minha S, Chen F, Torguson R, Omar AF, Loh JP, Escarcega RO, Lipinski MJ, Baker NC, Kitabata H, Ota H, Suddath WO, Satler LF, Pichard AD, Waksman R. Clinical presentation and outcomes of coronary in-stent restenosis across 3-stent generations. Circulation. Cardiovascular interventions. 2014 Dec:7(6):768-76. doi: 10.1161/CIRCINTERVENTIONS.114.001341. Epub 2014 Dec 2 [PubMed PMID: 25466551]
Level 2 (mid-level) evidenceOchijewicz D, Tomaniak M, Koltowski L, Rdzanek A, Pietrasik A, Kochman J. Intravascular imaging of coronary artery disease: recent progress and future directions. Journal of cardiovascular medicine (Hagerstown, Md.). 2017 Oct:18(10):733-741. doi: 10.2459/JCM.0000000000000552. Epub [PubMed PMID: 28834786]
Level 3 (low-level) evidenceGiacoppo D, Gargiulo G, Aruta P, Capranzano P, Tamburino C, Capodanno D. Treatment strategies for coronary in-stent restenosis: systematic review and hierarchical Bayesian network meta-analysis of 24 randomised trials and 4880 patients. BMJ (Clinical research ed.). 2015 Nov 4:351():h5392. doi: 10.1136/bmj.h5392. Epub 2015 Nov 4 [PubMed PMID: 26537292]
Level 1 (high-level) evidenceShlofmitz E, Kuku KO, Waksman R, Garcia-Garcia HM. Intravascular ultrasound-guided drug-eluting stent implantation. Minerva cardioangiologica. 2019 Aug:67(4):306-317. doi: 10.23736/S0026-4725.19.04895-3. Epub 2019 Mar 4 [PubMed PMID: 30845795]
Liu ZJ, Shi B, Deng CC, Xu GX, Zhao RZ, Shen CY, Wang ZL, Liu HL. [Analysis of optical coherence tomography of early and very late stent restenosis after drug-eluting stent implantation]. Zhonghua yi xue za zhi. 2017 Jun 20:97(23):1778-1783. doi: 10.3760/cma.j.issn.0376-2491.2017.23.005. Epub [PubMed PMID: 28647998]
Liu HF, Wang M, Xu YS, Shrestha MK, Lu XR, Lei JQ. Diagnostic accuracy of dual-source and 320-row computed tomography angiography in detecting coronary in-stent restenosis: a systematic review and meta-analysis. Acta radiologica (Stockholm, Sweden : 1987). 2019 Feb:60(2):149-159. doi: 10.1177/0284185118774956. Epub 2018 May 14 [PubMed PMID: 29758995]
Level 1 (high-level) evidenceWang LF, Tao LW, Huang MX, Liao WB, Zhu YZ, Zhou WB, Li H, Li D, Lu HT, Zhang BZ, Chen Z. Clinical Evaluation of Coronary In-Stent Restenosis Using Dual-Source Computed Tomography. Echocardiography (Mount Kisco, N.Y.). 2015 Nov:32(11):1681-7. doi: 10.1111/echo.12932. Epub 2015 Mar 25 [PubMed PMID: 25816917]
Bourantas CV, Jaffer FA, Gijsen FJ, van Soest G, Madden SP, Courtney BK, Fard AM, Tenekecioglu E, Zeng Y, van der Steen AFW, Emelianov S, Muller J, Stone PH, Marcu L, Tearney GJ, Serruys PW. Hybrid intravascular imaging: recent advances, technical considerations, and current applications in the study of plaque pathophysiology. European heart journal. 2017 Feb 7:38(6):400-412. doi: 10.1093/eurheartj/ehw097. Epub [PubMed PMID: 27118197]
Level 3 (low-level) evidenceNam CW, Rha SW, Koo BK, Doh JH, Chung WY, Yoon MH, Tahk SJ, Lee BK, Lee JB, Yoo KD, Cho YK, Chung IS, Hur SH, Kim KB, Choi CU, Oh DJ. Usefulness of coronary pressure measurement for functional evaluation of drug-eluting stent restenosis. The American journal of cardiology. 2011 Jun 15:107(12):1783-6. doi: 10.1016/j.amjcard.2011.02.328. Epub 2011 Apr 8 [PubMed PMID: 21481824]
Uchida T, Popma J, Stone GW, Ellis SG, Turco MA, Ormiston JA, Muramatsu T, Nakamura M, Nanto S, Yokoi H, Baim DS. The clinical impact of routine angiographic follow-up in randomized trials of drug-eluting stents: a critical assessment of "oculostenotic" reintervention in patients with intermediate lesions. JACC. Cardiovascular interventions. 2010 Apr:3(4):403-11. doi: 10.1016/j.jcin.2010.01.010. Epub [PubMed PMID: 20398868]
Level 1 (high-level) evidenceAlfonso F, García P, Fleites H, Pimentel G, Sabaté M, Hernández R, Escaned J, Bañuelos C, Pérez-Vizcayno MJ, Moreno R, Macaya C. Repeat stenting for the prevention of the early lumen loss phenomenon in patients with in-stent restenosis. Angiographic and intravascular ultrasound findings of a randomized study. American heart journal. 2005 Feb:149(2):e1-8 [PubMed PMID: 15846250]
Level 1 (high-level) evidenceHolmes DR Jr, Teirstein P, Satler L, Sketch M, O'Malley J, Popma JJ, Kuntz RE, Fitzgerald PJ, Wang H, Caramanica E, Cohen SA, SISR Investigators. Sirolimus-eluting stents vs vascular brachytherapy for in-stent restenosis within bare-metal stents: the SISR randomized trial. JAMA. 2006 Mar 15:295(11):1264-73 [PubMed PMID: 16531619]
Level 1 (high-level) evidenceStone GW, Ellis SG, O'Shaughnessy CD, Martin SL, Satler L, McGarry T, Turco MA, Kereiakes DJ, Kelley L, Popma JJ, Russell ME, TAXUS V ISR Investigators. Paclitaxel-eluting stents vs vascular brachytherapy for in-stent restenosis within bare-metal stents: the TAXUS V ISR randomized trial. JAMA. 2006 Mar 15:295(11):1253-63 [PubMed PMID: 16531618]
Level 1 (high-level) evidenceWaksman R, Iantorno M. Refractory In-Stent Restenosis: Improving Outcomes by Standardizing Our Approach. Current cardiology reports. 2018 Oct 22:20(12):140. doi: 10.1007/s11886-018-1076-6. Epub 2018 Oct 22 [PubMed PMID: 30350271]
Negi SI, Torguson R, Gai J, Kiramijyan S, Koifman E, Chan R, Randolph P, Pichard A, Satler LF, Waksman R. Intracoronary Brachytherapy for Recurrent Drug-Eluting Stent Failure. JACC. Cardiovascular interventions. 2016 Jun 27:9(12):1259-1265. doi: 10.1016/j.jcin.2016.03.018. Epub 2016 Jun 20 [PubMed PMID: 27339842]
Varghese MJ, Bhatheja S, Baber U, Kezbor S, Chincholi A, Chamaria S, Buckstein M, Bakst R, Kini A, Sharma S. Intravascular Brachytherapy for the Management of Repeated Multimetal-Layered Drug-Eluting Coronary Stent Restenosis. Circulation. Cardiovascular interventions. 2018 Oct:11(10):e006832. doi: 10.1161/CIRCINTERVENTIONS.118.006832. Epub [PubMed PMID: 30354630]
Albiero R, Silber S, Di Mario C, Cernigliaro C, Battaglia S, Reimers B, Frasheri A, Klauss V, Auge JM, Rubartelli P, Morice MC, Cremonesi A, Schofer J, Bortone A, Colombo A, RESCUT Investigators. Cutting balloon versus conventional balloon angioplasty for the treatment of in-stent restenosis: results of the restenosis cutting balloon evaluation trial (RESCUT). Journal of the American College of Cardiology. 2004 Mar 17:43(6):943-9 [PubMed PMID: 15028348]
Level 1 (high-level) evidenceKufner S, Joner M, Schneider S, Tölg R, Zrenner B, Repp J, Starkmann A, Xhepa E, Ibrahim T, Cassese S, Fusaro M, Ott I, Hengstenberg C, Schunkert H, Abdel-Wahab M, Laugwitz KL, Kastrati A, Byrne RA, ISAR-DESIRE 4 Investigators. Neointimal Modification With Scoring Balloon and Efficacy of Drug-Coated Balloon Therapy in Patients With Restenosis in Drug-Eluting Coronary Stents: A Randomized Controlled Trial. JACC. Cardiovascular interventions. 2017 Jul 10:10(13):1332-1340. doi: 10.1016/j.jcin.2017.04.024. Epub [PubMed PMID: 28683939]
Level 1 (high-level) evidenceKastrati A, Mehilli J, von Beckerath N, Dibra A, Hausleiter J, Pache J, Schühlen H, Schmitt C, Dirschinger J, Schömig A, ISAR-DESIRE Study Investigators. Sirolimus-eluting stent or paclitaxel-eluting stent vs balloon angioplasty for prevention of recurrences in patients with coronary in-stent restenosis: a randomized controlled trial. JAMA. 2005 Jan 12:293(2):165-71 [PubMed PMID: 15644543]
Level 1 (high-level) evidenceAlfonso F, Pérez-Vizcayno MJ, Hernández R, Bethencourt A, Martí V, López-Mínguez JR, Angel J, Iñiguez A, Morís C, Cequier A, Sabaté M, Escaned J, Jiménez-Quevedo P, Bañuelos C, Suárez A, Macaya C, RIBS-II Investigators. Long-term clinical benefit of sirolimus-eluting stents in patients with in-stent restenosis results of the RIBS-II (Restenosis Intra-stent: Balloon angioplasty vs. elective sirolimus-eluting Stenting) study. Journal of the American College of Cardiology. 2008 Nov 11:52(20):1621-7. doi: 10.1016/j.jacc.2008.08.025. Epub [PubMed PMID: 18992651]
Level 1 (high-level) evidenceBaschet L, Bourguignon S, Marque S, Durand-Zaleski I, Teiger E, Wilquin F, Levesque K. Cost-effectiveness of drug-eluting stents versus bare-metal stents in patients undergoing percutaneous coronary intervention. Open heart. 2016:3(2):e000445. doi: 10.1136/openhrt-2016-000445. Epub 2016 Aug 25 [PubMed PMID: 27621830]
Habara S, Iwabuchi M, Inoue N, Nakamura S, Asano R, Nanto S, Hayashi Y, Shiode N, Saito S, Ikari Y, Kimura T, Hosokawa J, Nakamura M, Kotani J, Kozuma K, Mitsudo K. A multicenter randomized comparison of paclitaxel-coated balloon catheter with conventional balloon angioplasty in patients with bare-metal stent restenosis and drug-eluting stent restenosis. American heart journal. 2013 Sep:166(3):527-33. doi: 10.1016/j.ahj.2013.07.002. Epub 2013 Aug 13 [PubMed PMID: 24016503]
Level 1 (high-level) evidenceHabara S, Mitsudo K, Kadota K, Goto T, Fujii S, Yamamoto H, Katoh H, Oka N, Fuku Y, Hosogi S, Hirono A, Maruo T, Tanaka H, Shigemoto Y, Hasegawa D, Tasaka H, Kusunose M, Otsuru S, Okamoto Y, Saito N, Tsujimoto Y, Eguchi H, Miyake K, Yoshino M. Effectiveness of paclitaxel-eluting balloon catheter in patients with sirolimus-eluting stent restenosis. JACC. Cardiovascular interventions. 2011 Feb:4(2):149-54. doi: 10.1016/j.jcin.2010.10.012. Epub [PubMed PMID: 21349452]
Level 1 (high-level) evidenceByrne RA, Neumann FJ, Mehilli J, Pinieck S, Wolff B, Tiroch K, Schulz S, Fusaro M, Ott I, Ibrahim T, Hausleiter J, Valina C, Pache J, Laugwitz KL, Massberg S, Kastrati A, ISAR-DESIRE 3 investigators. Paclitaxel-eluting balloons, paclitaxel-eluting stents, and balloon angioplasty in patients with restenosis after implantation of a drug-eluting stent (ISAR-DESIRE 3): a randomised, open-label trial. Lancet (London, England). 2013 Feb 9:381(9865):461-7. doi: 10.1016/S0140-6736(12)61964-3. Epub 2012 Dec 1 [PubMed PMID: 23206837]
Level 1 (high-level) evidenceAlfonso F, Pérez-Vizcayno MJ, Cárdenas A, García del Blanco B, García-Touchard A, López-Minguéz JR, Benedicto A, Masotti M, Zueco J, Iñiguez A, Velázquez M, Moreno R, Mainar V, Domínguez A, Pomar F, Melgares R, Rivero F, Jiménez-Quevedo P, Gonzalo N, Fernández C, Macaya C, RIBS IV Study Investigators (under auspices of Interventional Cardiology Working Group of Spanish Society of Cardiology). A Prospective Randomized Trial of Drug-Eluting Balloons Versus Everolimus-Eluting Stents in Patients With In-Stent Restenosis of Drug-Eluting Stents: The RIBS IV Randomized Clinical Trial. Journal of the American College of Cardiology. 2015 Jul 7:66(1):23-33. doi: 10.1016/j.jacc.2015.04.063. Epub [PubMed PMID: 26139054]
Level 1 (high-level) evidenceAlfonso F, Cuesta J, Pérez-Vizcayno MJ, García Del Blanco B, Rumoroso JR, Bosa F, Pérez de Prado A, Masotti M, Moreno R, Cequier A, Gutiérrez H, García Touchard A, López-Mínguez JR, Zueco J, Martí V, Velázquez M, Morís C, Bastante T, García-Guimaraes M, Rivero F, Fernández C, Interventional Cardiology Working Group of the Spanish Society of Cardiology. Bioresorbable Vascular Scaffolds for Patients With In-Stent Restenosis: The RIBS VI Study. JACC. Cardiovascular interventions. 2017 Sep 25:10(18):1841-1851. doi: 10.1016/j.jcin.2017.06.064. Epub 2017 Aug 30 [PubMed PMID: 28866036]
Picard F, Avram R, Marquis-Gravel G, Tadros VX, Ly HQ, de Hemptinne Q, Dorval JF, L'allier PL, Tanguay JF. Bioresorbable vascular scaffold to treat in-stent restenosis: Single-center experience. Journal of interventional cardiology. 2017 Dec:30(6):558-563. doi: 10.1111/joic.12420. Epub 2017 Aug 7 [PubMed PMID: 28786151]
Moscarella E, Tanaka A, Ielasi A, Cortese B, Coscarelli S, De Angelis MC, Piraino D, Latib A, Grigis G, Bianchi R, Buccheri D, Calabrò P, Tespili M, Silva Orrego P, Colombo A, Varricchio A. Bioresorbable vascular scaffold versus everolimus-eluting stents or drug eluting balloon for the treatment of coronary in-stent restenosis: 1-Year follow-up of a propensity score matching comparison (the BIORESOLVE-ISR Study). Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2018 Oct 1:92(4):668-677. doi: 10.1002/ccd.27473. Epub 2018 Jan 22 [PubMed PMID: 29356269]
Siontis GC, Stefanini GG, Mavridis D, Siontis KC, Alfonso F, Pérez-Vizcayno MJ, Byrne RA, Kastrati A, Meier B, Salanti G, Jüni P, Windecker S. Percutaneous coronary interventional strategies for treatment of in-stent restenosis: a network meta-analysis. Lancet (London, England). 2015 Aug 15:386(9994):655-64. doi: 10.1016/S0140-6736(15)60657-2. Epub [PubMed PMID: 26334160]
Level 1 (high-level) evidenceGiacoppo D, Colleran R, Cassese S, Frangieh AH, Wiebe J, Joner M, Schunkert H, Kastrati A, Byrne RA. Percutaneous Coronary Intervention vs Coronary Artery Bypass Grafting in Patients With Left Main Coronary Artery Stenosis: A Systematic Review and Meta-analysis. JAMA cardiology. 2017 Oct 1:2(10):1079-1088. doi: 10.1001/jamacardio.2017.2895. Epub [PubMed PMID: 28903139]
Level 1 (high-level) evidenceGoto K, Zhao Z, Matsumura M, Dohi T, Kobayashi N, Kirtane AJ, Rabbani LE, Collins MB, Parikh MA, Kodali SK, Leon MB, Moses JW, Mintz GS, Maehara A. Mechanisms and Patterns of Intravascular Ultrasound In-Stent Restenosis Among Bare Metal Stents and First- and Second-Generation Drug-Eluting Stents. The American journal of cardiology. 2015 Nov 1:116(9):1351-7. doi: 10.1016/j.amjcard.2015.07.058. Epub 2015 Aug 14 [PubMed PMID: 26341188]
Kang SJ, Mintz GS, Kim WJ, Lee JY, Park DW, Yun SC, Lee SW, Kim YH, Lee CW, Han KH, Kim JJ, Park SW, Park SJ. Effect of intravascular ultrasound findings on long-term repeat revascularization in patients undergoing drug-eluting stent implantation for severe unprotected left main bifurcation narrowing. The American journal of cardiology. 2011 Feb 1:107(3):367-73. doi: 10.1016/j.amjcard.2010.09.028. Epub [PubMed PMID: 21257000]
Iakovou I, Mintz GS, Dangas G, Abizaid A, Mehran R, Lansky AJ, Kobayashi Y, Hirose M, Ashby DT, Stone GW, Moses JW, Leon MB. Optimal final lumen area and predictors of target lesion revascularization after stent implantation in small coronary arteries. The American journal of cardiology. 2003 Nov 15:92(10):1171-6 [PubMed PMID: 14609591]
Mintz GS, Choi SY. Optimal stent expansion and complete neointimal coverage: does this association make sense? JACC. Cardiovascular interventions. 2009 Oct:2(10):995-6. doi: 10.1016/j.jcin.2009.08.003. Epub [PubMed PMID: 19850261]