Introduction
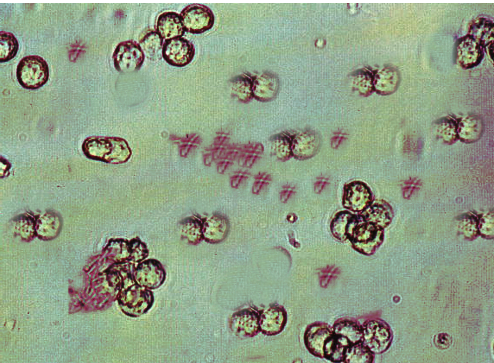
Recurrent urinary tract infections (UTIs) are 2 or more episodes of acute bacterial cystitis, associated symptoms within the last 6 months, or at least 3 episodes within the previous year.[1] Recurrent UTIs are more common in women. The cost of treating UTIs in the United States is about 3.5 billion dollars annually.[2] A UTI is traditionally defined as more than 100,000 colony-forming units (CFU/mL) of urine associated with typical acute symptoms of dysuria, urgency, frequency, or suprapubic pain (see Image. Urinary Tract Infection).[3] However, more than 100 CFUs of Escherichia coli with specific acute urinary symptoms have a positive predictive value of about 90%, indicating that a lower CFU threshold is more appropriate in diagnosing simple and recurrent UTIs.[4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Urinary Tract Infection Risk Factors
Several conditions may predispose both men and women to have an increased risk of developing acute and recurrent UTIs, including:
- Anatomical defects that lead to stasis, obstruction, or urinary reflux
- Atrophic vaginitis
- Bladder diverticula, especially those that do not drain well
- Cystoceles and pelvic organ prolapse in women
- Functional defects (eg, overactive bladder and urinary incontinence)
- Inadequate or incomplete treatment of the initial acute cystitis
- Increasing bacterial resistance to antibiotics
- Older men with outlet obstruction or neurogenic bladder, causing urinary stasis and incomplete bladder emptying
- Sexually active women without any identifiable structural abnormality or another predisposing condition
- Intraluminal (eg, bladder stones, neoplasms, indwelling catheters, stents, foreign bodies), intramural (eg, ureteral stenosis/strictures), and extramural (eg, inflammatory mass, fibrosis, extrinsic mass effect, or neoplasm) lesions
- Ureteroceles, urinary fistula, and urolithiasis
- Vesicoureteric reflux (identified in up to 40% of children with a first UTI) [5][6][7][8][9]
Notably, immunodeficiency alone typically does not lead to isolated recurrent UTIs.
Epidemiology
Approximately 1 in 3 women have an uncomplicated UTI before the age of 24. The lifetime prevalence of at least 1 symptomatic UTI in women is estimated to be over 50%, with about 26% of women demonstrating a recurrence during 6 months of follow-up after treatment of the initial UTI. In a study in the primary care setting, 53% of women who were 55 and older and 36% of younger women reported a recurrence within 1 year.[1]
Pathophysiology
Recurrent UTIs usually involve new infections with different bacterial organisms. If the infection persists after treatment, this may indicate an untreated source, such as an abscess, urinary stone, or prostatitis. The source of these recurrent infections is the same as any uncomplicated cystitis. Typically, the rectal bacterial flora contaminates the periurethral area and urethra. Bacteria can quickly ascend and reach the bladder. Research indicates a complex and poorly understood relationship between the microbiomes of the intestines, vagina, and urinary tract.[10] Three-quarters of recurrent UTIs are caused by Escherichia coli. Other commonly found organisms include Klebsiella, Staphylococcus saprophyticus, Proteus mirabilis, and Enterococcus faecalis.[11]
Differentiating rapid reinfection (a different organism) from a relapse (the same organism not completely treated) is essential. A relapse is further defined as a recurrence within 2 weeks of completing therapy with the same organism. Reinfection occurs if a new infection from the same organism is diagnosed more than 2 weeks after treatment. Most recurrent UTIs typically seen in medical offices and clinics are reinfections and do not warrant an extensive urological evaluation or imaging.
Indications for imaging include persistent hematuria, a history of kidney stones, repeatedly finding Proteus (often associated with urolithiasis), and relapsing infections. Menopause and atrophic vaginitis cause the number of protective vaginal lactobacilli to decrease. Bladder contractions tend to become less forceful, leading to higher postvoid residual volumes predisposing to recurrent UTIs. The numbers of Lactobacilli in the vagina naturally decline. The contraction of the bladder weakens with age, leading to difficulties in complete emptying.
Risk Factors for Recurrent Infections
The most significant risk factors for recurrent UTI include the use of a diaphragm with spermicide, menopause, untreated atrophic vaginitis, and frequent sexual intercourse. Spermicides and lack of estrogen effect will disrupt the normal vaginal flora, while sexual intercourse tends to introduce vaginal bacteria into the urethra and bladder. Genetic factors are likely if a sister or mother has a history of frequent UTIs. Recurrent UTI risk factors include:
- Bladder diverticula
- Bladder fistula
- Chronic diarrhea
- Cystocele
- Diabetes
- First UTI before age 16
- Genetic predisposition (usually through bacterial/vaginal mucosal adherence factors)
- Higher frequency of sexual intercourse (>2 times a week triples the risk of a UTI)
- History of 5 or more UTIs
- Inadequate fluid intake (low urinary volumes)
- Increased post-void residual urine (incomplete bladder emptying >150 mL)
- Mother or sister with a history of frequent or multiple UTIs
- New or multiple sexual partners
- Short anal to urethral meatus distance
- Urethral diverticula
- Urinary incontinence
- Use of spermicide-coated condoms [11][12][13][14][15]
Personal Hygiene Factors
Hygiene risk factors that increase the likelihood of developing recurrent UTIs include:
- Failing to use a gentle, liquid soap when washing the vaginal area
- Not cleaning the urethral area first when washing
- Not using clean, soft washcloths to clean the vaginal area when washing
- Not using vaginal estrogen, when appropriate, in those who are postmenopausal
- Not washing hands before wiping the vaginal area after voiding
- Taking baths instead of showers
- Wiping and washing the vaginal area (incorrectly) from back to front or more than once
History and Physical
Accurate assessment of a UTI requires a complete history and physical examination. Differentiating the various types of UTIs, their severity, and associated complications also necessitates recognizing characteristic clinical features.
Urinary Tract Infection Clinical Features
Acute simple cystitis presents with urinary frequency or urgency symptoms, dysuria, or suprapubic pain. The probability of cystitis is >90% in women with dysuria and frequency without vaginal discharge or irritation.[16] The presence of fever, chills, rigors, marked fatigue, or malaise suggests that the infection has extended beyond the bladder and is now regarded as acute complicated cystitis. Pyuria and bacteriuria without any urinary symptoms are not urinary tract infections and do not require treatment except in certain circumstances (ie, pregnancy before urological surgery).
Clinical features of pyelonephritis include fever, chills, flank pain, costovertebral angle tenderness, nausea, and vomiting. Symptoms of cystitis are often, but not universally, present in patients with pyelonephritis. Women with recurrent UTIs should have a pelvic examination to check for cystoceles, vaginitis, vaginal atrophy, and prolapse of pelvic organs. The results of a study of 113 women found that hematuria and urgency as symptoms during an initial urinary infection were the strongest predictors of a second UTI.
Men who have recurrent episodes of cystitis should undergo an evaluation for prostatitis. At the same time, older or debilitated patients may present with more generalized symptoms of infection (eg, fever and chills) or a change in mental status without any precise localization to the urinary tract.
Recurrent Versus Relapsing Urinary Tract Infection
A recurrence is termed reinfection if the interval between the 2 episodes is longer than 2 weeks, if a different uropathogenic strain is documented, or if a sterile culture (with the patient off antibiotics) was documented between the 2 UTI episodes. If the interval between the 2 episodes is less than 2 weeks, this is considered a relapse. Relapsing infections often require additional evaluation with urological imaging, which is rarely indicated in recurrent infections.
Positive urine cultures should be documented to confirm a diagnosis of recurrent UTIs, and appropriate urinary symptoms should be noted. A catheterized specimen will be needed if clean-catch urine samples are suspicious of contamination (especially in women). In women who have very rapid recurrences of cystitis after treatment, clinical clues and culture results will allow classification of cystitis as a reinfection (ie, a new infection after the previous one was wholly eradicated) or a relapse (ie, the reemergence of the last infection with the same bacteria, which was incompletely eradicated previously.)
Evaluation
Laboratory Studies for Urinary Tract Infection
The typical patient with recurrent UTIs does not require cystoscopy or urological imaging.[1][3][11][17] In women with a history of recurrent UTIs with typical symptoms, urological evaluation primarily involves a urine culture and sensitivity. Furthermore, urine cultures are obtained in patients with severe infection or a high risk of antibiotic resistance (eg, multidrug-resistant isolate, recent inpatient admission, recent antibiotic use, a history of travel to India, Israel, Spain, or Mexico).
Urine cultures are also necessary to differentiate recurrent infections (repeat infections with different organisms) from relapsing (identical organisms on culture). Relapsing infections suggest a persistent source of bacterial inoculation, eg, an abscess, chronic bacterial prostatitis, or an infected stone. The American Urological Association (AUA) guidelines on recurrent UTIs in women recommend obtaining a urinalysis and urine culture with each episode of acute cystitis.[3]
Urological Imaging Studies
Urological imaging is advised for only a select group of women. Indications for urological imaging include relapsing infections, persistent hematuria after treatment, a history of stone passage, or repeated isolation of Proteus from the urine, often associated with renal stones. Preferred imaging modalities include renal ultrasonography or, ideally, a computed tomography scan of the abdomen and pelvis.
Pediatric Urinary Tract Infection Evaluation
Various sampling methods have been described to establish the diagnosis of UTI in the pediatric population. Obtaining the urine sample utilizing suprapubic aspiration or catheterization is more invasive but results in lower contamination and more reliable results. If the urine sample is collected through a plastic bag, several steps are required to rule out the possibility of a UTI, including dipstick evaluation and microscopic analysis.
The presence of leukocyte esterase and nitrite on a urinary dipstick and the possibility of pyuria and bacteriuria should be excluded to rule out the impression of a UTI. Utilizing a clean, voided midstream urine sample for the diagnosis is limited to toilet-trained children and individuals.[18] Patients with negative urinary cultures who have persistent symptoms should be evaluated for other causes, including atypical organisms, interstitial cystitis, endometriosis, atrophic vaginitis, trauma, urethral pathology, neoplasms, diverticula, strictures, medication adverse effects, and vaginitis.[19][20][21]
Diagnostic Cystoscopy
Performing a cystoscopy to diagnose recurrent UTIs is rarely indicated, as this might only induce an ascending lower urinary tract infection and rarely provides any useful clinical information.[3][22][23] While cystoscopy is rarely helpful when utilized routinely, it can be useful in managing selected postoperative cases to identify possible ureteral or bladder injuries, evaluate incomplete bladder emptying, or visualize vesical calculi.
The optimal recommended type of irrigation fluid utilized during cystoscopy has been investigated. For instance, in the 8-month-long study of Cleveland health system clinics, a significantly higher rate of UTIs was found in those patients who had undergone cystoscopy with 10% dextrose and water irrigation compared to normal saline.[24] All cystoscopies were planned to exclude intraoperative ureteral injuries during complicated urogynecology procedures.
Treatment / Management
Treatment for Uncomplicated Urinary Tract Infections
Acute uncomplicated UTIs are primarily managed in the outpatient setting.[6] Women with typical symptoms of acute cystitis can be prescribed antibiotic therapy through telehealth.[25] In cases of initial treatment failure and high-risk patients, a urine culture is recommended to optimize antibiotic therapy. The decision to hospitalize is based on the individual case characteristics. Most patients with persistent fever, pain, inability to take oral medicines, or a history of poor medication adherence should be managed as inpatients.(A1)
Management of simple cystitis is relatively straightforward. Urine cultures should be obtained before initiating therapy. The indications for urine culture are recommended in the following cases:
- For patients treated for cystitis in the past 3 months, urine culture and susceptibility testing should be obtained to guide antibiotic therapy due to the increased risk of antibiotic resistance.
- Patients with complicated cystitis or pyelonephritis should also have urine cultures before initiating empiric antibiotics.
Antibiotic therapy
The first-line options for empiric antibiotic therapy for uncomplicated cystitis are:
- Nitrofurantoin: Nitrofurantoin 100 mg twice daily orally for 5 to 7 days. This antibiotic should be avoided in suspected pyelonephritis (due to poor tissue penetration) or if the creatinine clearance is less than 30 mL/min.
- Sulfamethoxazole-trimethoprim: The recommended dosage for sulfamethoxazole-trimethoprim (SMX-TMP) is 160/800 mg twice daily orally for 3 to 14 days. The antibiotic should be avoided if the local resistance rate exceeds 20% or in patients with an estimated glomerular filtration rate (GFR) of <15 mL/min.
- Fosfomycin: This antibiotic should be taken as a single oral dose of 3 g. Fosfomycin is recommended as first-line therapy when other agents have failed or cannot be used.
- Pivmecillinam: This antibiotic, FDA-approved in April 2024, is now available in the US. Pivmecillinam converted to mecillinam, a unique extended-spectrum β-lactam oral antibiotic, is approved for first-line therapy in uncomplicated urinary tract infections.[26] While not indicated for systemic infections or sepsis due to inadequate tissue penetration, pivmecillinam is very effective in lower urinary tract infections due to susceptible strains of E. coli, Proteus mirabilis, and Staphylococcus saprophyticus.[26][27][28][29][30][31] This medication is recommended for susceptible organisms when other first-line antibiotics are not possible or clinically fail due to bacterial resistance. The standard recommended dose for acute simple cystitis is 185 mg 3 times daily for 3 to 7 days. A dose reduction is recommended if the GFR is <30 mL/min. It should not be used if the GFR is <10 mL/min.[6]
Oral β-lactams are the next best choice if first-line antibiotics cannot be prescribed. Amoxicillin-clavulanate 500 mg twice daily, cefdinir 300 mg twice daily, cefadroxil 500 mg twice daily, and cefpodoxime 100 mg twice daily are each given for 5 to 7 days. Ampicillin or amoxicillin should be avoided due to high rates of resistance.[32][33] If the β-lactams cannot be used, fluoroquinolones such as levofloxacin 250 to 500 mg daily, ciprofloxacin 250 to 500 mg twice daily, or norfloxacin 400 mg twice daily for 3 days are alternatives. Fluoroquinolones are contraindicated in pregnancy and avoided when possible to minimize the development of quinolone resistance. Please see StatPearls' companion resource, "Uncomplicated Urinary Tract Infections," for more information.
To manage inpatient risk factors for multidrug-resistant (MDR) pathogen infections, carbapenems (imipenem 500 mg IV Q6H, meropenem 1 g intravenously (IV), or doripenem 500 mg Q8H) are used. Oral pivmecillinam may also be considered for lower urinary tract infections due to susceptible organisms due to its effectiveness against multidrug-resistant and extended-spectrum beta-lactamase (ESBL)-producing microorganisms, especially E. coli.[26][27][28][29][30][31]
If no risk factors for multidrug resistance are present, ceftriaxone 1 gram IV daily or piperacillin-tazobactam 3.375 grams IV Q6H are prescribed. Fluoroquinolones (ciprofloxacin or levofloxacin), both oral and parenteral, are also alternatives. Carbapenems (as above) and vancomycin are typically prescribed only for critically ill patients. Aminoglycosides may also be prescribed selectively, depending on urine culture, sensitivity results, and local antibiotic susceptibility patterns.
Symptoms should respond to antibiotic therapy within 48 hours of initiation. If no improvement is noticed within the first 48 hours after starting treatment, a repeat urine culture should be obtained along with urologic imaging to rule out complications such as an obstructing urinary stone, hydronephrosis, urinary retention, renal abscess, or pyelonephritis. Clinicians should not generally perform a posttreatment test of cure urinalysis or urine culture in asymptomatic patients with uncomplicated urinary tract infections. Repeat urine cultures should be obtained to guide further management when UTI symptoms persist following antimicrobial therapy.
Preferred agents for UTIs in patients with renal failure include carbapenems, cephalosporins, doxycycline, fosfomycin, penicillins, and quinolones like norfloxacin. Intravesical instillations of an antibiotic solution, eg, gentamicin, may also be prescribed in patients with severe renal impairment.[34][35][36][37][38] For patients with end-stage renal failure, quinolones (ciprofloxacin, levofloxacin) are the first-line agents for UTIs, with cefdinir or cefpodoxime as second-line therapy.[39][40] For prophylaxis in patients with end-stage renal failure, the preferred antimicrobials are trimethoprim alone and fosfomycin.[41] Intravesical therapy may also be used in selected cases.(A1)
Treatment for Recurrent UTIs
Recommended treatments for recurrent UTIs include maximizing personal hygiene factors, avoiding spermicides, wiping correctly, increasing fluid intake and hydration, and using vaginal estrogens if appropriate. The effectiveness of lifestyle changes in personal hygiene in reducing recurrent UTIs is inconclusive. However, recommending improved hygiene has no negative consequences and might be of some benefit.[13][42] The use of probiotics is unclear, as clinical trials to date are inconclusive.[43][44][45][46][47][48][49](A1)
When conservative measures fail to control recurrent UTIs, commonly recommended initial nonantibiotic prophylactic therapies include the following:
- Cranberry products: Although recommended as first-line prophylactic agents, cranberry products' efficacy remains controversial, as a definitive benefit has not yet been established. Cranberries are thought to work by providing proanthocyanidins, which decrease bacterial adherence to the urothelium. While this sounds reasonable and is an attractive hypothesis, commercially available cranberry products have limited amounts of proanthocyanidins. The AUA guidelines suggest using this treatment but advise patients that effectiveness is uncertain and alternative measures may be necessary.
- D-mannose: Binding to bacterial surface ligands is thought to help reduce the adherence of infecting organisms to the urothelial mucosa in recurrent cystitis. However, evidence of a reduction in recurrent infections is conflicting, and definitive trials have not yet been conducted. The product is relatively costly, and optimal dosages are still undetermined, although 500 mg twice daily is commonly suggested. Recent randomized trials have failed to show any clinical benefit.
- Methenamine prophylaxis: Along with vitamin C, the treatment acidifies the urine. If the urinary pH remains acidic, preferably <5.5, the bladder converts the methenamine to formaldehyde. A recent systematic review found methenamine to be an effective and well-tolerated prophylactic antimicrobial agent, avoiding the need for systemic antibiotics and their potential adverse effects. A separate multi-institutional, clinical randomized trial study compared methenamine to trimethoprim for UTI prophylaxis and found the same rate of recurrences for both after 1 year. Although some studies have failed to prove a long-term benefit, the majority show efficacy, indicating that further use and research of methenamine is warranted, particularly given recent trends demonstrating increasing antibiotic resistance. A GFR is <10 mL/min is a contraindication.
- Estrogen vaginal cream: The topical treatment reduces recurrent UTIs in those who are postmenopausal and should be prescribed when appropriate in addition to other prophylactic measures.
- Lifestyle and behavioral modifications: A study of 47 patients followed for 6 months found probiotics, D-mannose, and cranberry products helpful. Women in the study had a reduced rate of UTIs by 76%, and antibiotic use dropped by over 90%. Such a combination of nonantibiotic therapy appears quite promising as being effective, avoiding the potential adverse effects of antibiotic use, and minimizing bacterial resistance. However, further research with larger sample sizes using different components is needed to confirm and determine the optimal ingredients and dosages.
- Vaccines: Immunizations to prevent recurrent UTIs are still mostly under development, but several appear promising. The oral vaccine, MV140, has shown good efficacy in preventing recurrent UTIs in several studies with safety data and minimal adverse effects. A preliminary long-term study of MV140 has recently demonstrated efficacy over 9 years following the initial administration. MV140 contains heat-inactivated strains of Escherichia coli, Klebsiella pneumoniae, Enterococcus faecalis, and Proteus vulgaris, which induce host antibody production and modify the bladder's local immune response. While not approved for use in the US or Canada, the vaccine is now available in several countries worldwide, including Australia, Chile, the Dominican Republic, Lithuania, Mexico, the Netherlands, New Zealand, Norway, Portugal, Spain, Sweden, and the United Kingdom.
- Antibiotic prophylaxis: Prophylaxis successfully controls recurrent UTIs, but alternative nonantibiotic means are usually recommended first. This approach limits the development of bacterial resistance, eliminates antibiotic-related adverse effects, and reduces costs. Prophylaxis is reasonable when other more conservative measures fail, or evidence of multiple rapid recurrences is apparent. However, use is inappropriate in patients who have permanent catheters or nephrostomies, as this will rapidly lead to highly resistant organisms.
- Postcoital prophylaxis is appropriate for women with frequent episodes of cystitis that are associated with sexual activity.
- Another option is self-directed therapy, where patients start a short course of antibiotics at the first sign or symptom of a UTI. Such an approach is reasonable if the patient is sufficiently educated about infection symptoms and will reliably follow instructions. If possible, a urine culture should still be obtained before starting treatment. Efficacy appears equal to continuous low-dose prophylaxis regimens with fewer gastrointestinal adverse effects. If this fails, then a continuous prophylactic treatment protocol is needed.
- Long-term low-dose antibiotic prophylaxis is the gold standard method of recurrent UTI prevention. This regimen requires the highest level of patient compliance, has a long duration of therapy (at least 6 months), and risks increasing antibiotic resistance. Prophylaxis is indicated in the most intractable cases where more conservative measures have failed or cannot be effectively utilized.[50][51][52][53][54][55][56]
(A1)
- Intravesical therapy: Patients with intractable recurrent urinary tract infections and those already on intermittent self-catheterization can benefit from periodic intravesical prophylactic treatment with gentamicin or other antimicrobial agents such as chlorhexidine, hyaluronic acid, Lactobacillus rhamnosus, Neosporin (but not Neomycin), povidone-iodine solution, and tobramycin may also be used as alternatives.[34][35][37][38][57][58][59][36][60][60][61] Gentamicin is the most commonly used agent for this purpose. The usual dose is 80 mg gentamicin with 50 to 60 cc of normal saline.[59] (A1)
Surveillance urine testing and cultures in asymptomatic patients are not recommended. Asymptomatic patients, high-risk patients in nursing homes, and patients with diabetes do not benefit from an additional evaluation, and any bacteriuria should not be treated without symptoms. This recommendation does not apply to pregnant women or patients undergoing urinary tract surgery.[62][63][64][65][66](A1)
If a patient with a recurrent UTI develops an acute UTI, a urine culture should be obtained, and an alternate antibiotic agent should be prescribed to treat the infection. The duration of treatment should generally be no longer than 1 week. If the urine cultures indicate resistance to all available oral agents, parenteral antibiotics may be required. Fosfomycin may be an acceptable agent in such circumstances. An infectious disease consultation is suggested in such situations. The duration of therapy should generally be no more than 1 week.[67][68][69][70][71]
Long-Term, Low-Dose Antibiotic Prophylaxis
Continuous long-term prophylactic antibiotics typically use lower dosages than acute cystitis therapy. Therefore, this approach is called the long-term, low-dose therapy protocol. The antibiotic selection is based on the patient's culture and sensitivity results. Initial evaluation of the effectiveness of prophylaxis is suggested at 3 months. If effective, a 6- to 12-month duration is typical. Unfortunately, many individuals will revert to their prior pattern of infections when prophylaxis stops.[72][73] Some experts will recommend continuing prophylaxis for up to 2 or more years in selected patients. In such cases, nitrofurantoin, SMX-TMP, and trimethoprim are preferred agents.(A1)
Fosfomycin and pivmecillinam may be used for long-term low-dose prophylaxis, when appropriate, for otherwise resistant organisms where preferred agents cannot be administered and to help avoid the overuse of fluoroquinolones.[74] Carnitine deficiency is possible with long-term pivmecillinam use.
Quinolones are not preferred for prophylaxis because of the risk of increasing bacterial resistance. If quinolones are the antibiotic of choice, norfloxacin is preferred due to less tissue penetration outside the urinary tract and maintenance of urinary levels. This antibiotic is only selected when other first-line agents cannot be prescribed.[75]
Some patients have continued low-dose prophylaxis for years, but this practice has not been scientifically studied or validated. Potential adverse effects of long-term, low-dose antibiotic usage include gastrointestinal, hepatic, and pulmonary issues. Beta-lactams can be prescribed but tend to rapidly change gastrointestinal flora, carry a risk of pseudomembranous colitis (Clostridia), provoke bacterial resistance, and stimulate yeast overgrowth.
Limited data is available on the use of fosfomycin for UTI prophylaxis, but it may be appropriate in selected situations.[76] Prophylactic regimens are not written in stone; agents can be changed to help maintain efficacy. In patients with chronic, permanent catheters, a short course of 1 to 3 days of antibiotic prophylaxis can reduce the incidence of symptomatic UTIs. This approach may suit severely immunocompromised patients and possibly those with persistent infections after catheter changes. However, prophylaxis is not recommended routinely due to the expected increase in antibiotic use, which will result in worsening bacterial resistance patterns.[77](A1)
Some negative aspects of antibiotic prophylaxis are recognized, including added cost, inconvenience, allergies, and drug-drug interactions. Yeast superinfections and Clostridia overgrowth in the gastrointestinal tract may increase, and continuous prophylaxis promotes the emergence of more resistant urinary pathogens.[78] Long-term, low-dose antibiotic prophylaxis is effective but requires high patient compliance and risks resistance. Patients may relapse when prophylaxis is discontinued, and no data is available on continuing prophylaxis over 1 year.(A1)
Extended full-dose therapy for one month was compared to standard long-term low-dose prophylaxis in 246 women with uncomplicated UTIs in a recent study. A significant risk reduction for recurrent infections was noted in the extended full-dose therapy cohort. This interesting study suggests a possible benefit to extended full-dose therapy but requires confirmation by randomized trials.[79]
Antibiotic Agents for Recurrent Urinary Tract Infection Prophylaxis
Preferred antibiotic agents for recurrent UTI prophylaxis include:
- Nitrofurantoin at 50 to 100 mg before bed (HS) daily
- SMX-TMP at 40/200 mg HS daily
- Trimethoprim at 100 mg HS daily
Second-line antibiotic agents for recurrent UTI prophylaxis include:
- Cephalexin at 125 mg or 250 mg HS daily
- Cefaclor at 250 mg HS daily
- Fosfomycin at 3 gm every 10 days
- Norfloxacin at 400 mg HS daily
- Pivmecillinam at 185 mg daily
Urinary Tract Infection Prophylaxis in Renal Failure
Patients with significant renal failure (GFR <30 mL/min) cannot take nitrofurantoin, methenamine, or sulfa medications for prophylaxis. Preferred agents for prophylaxis in such situations include:
- Trimethoprim at 100 mg HS daily
- Fosfomycin at 3 gm every 10 days
- Quinolone at a reduced dosage (less preferred)
- Consider intermittent intravesical gentamicin [59][80]
The AUA guidelines are evidence-based recommendations for recurrent UTIs reviewed by an interprofessional expert committee.[3] The current guidelines, published in 2019, have been developed after an exhaustive review of the current medical literature from peer-reviewed journals.[3] The only nonantibiotic-based therapies for recurrent UTIs currently recommended by the AUA guidelines are cranberry prophylaxis and vaginal estrogen.[3]
Differential Diagnosis
Differential diagnosis to consider when evaluating recurrent UTIs include:
- Atrophic vaginitis: Thinning, drying, and inflammation of the vaginal tissues, frequently leading to urinary symptoms due to loss of estrogen
- Overactive bladder: Frequency and urgency with no evidence of infection
- Painful bladder syndrome: Dysuria, frequency, urgency, but no evidence of infection; diagnosis of exclusion
- Pelvic inflammatory disorder: Lower abdominal or pelvic pain, fever, cervical discharge, and cervical motion tenderness
- Prostatitis: May present with pain during ejaculation and tender prostate on digital rectal examination
- Urethritis: Urinalysis shows pyuria, not bacteria (common in sexually active women)
- Urolithiasis: Bladder or distal ureteral calculi; nephrolithiasis may be an infected focus
- Vaginitis: Presence of vaginal discharge, odor, pruritus, or dyspareunia with no frequency or urgency
Prognosis
Most recurrent UTIs have no long-term sequelae, and patients recover fully. The mortality associated with acute uncomplicated cystitis in women is negligible. However, in terms of morbidity, each episode of UTI results in a loss of 1.2 days of class or work attendance. Younger patients without preexisting comorbidities have the best prognosis.
Factors associated with a worse prognosis may include older age, recent urinary instrumentation, recent hospitalization or antibiotic therapy, preexisting diabetes mellitus, sickle cell anemia, or chronic renal disease.[81] UTIs occurring in the setting of specific anatomical abnormalities such as renal calculi, obstruction, hydronephrosis, colovesical fistula, neurogenic bladder, renal failure, or bladder exstrophy have a worse prognosis.
Complications
Risk factors for complications include urinary tract obstruction, recent urinary tract instrumentation, older age, and diabetes mellitus (particularly for emphysematous pyelonephritis and papillary necrosis). Acute pyelonephritis can also be complicated by the infection progressing to a renal abscess, perinephric abscess, papillary necrosis, or emphysematous pyelonephritis. This may present a lack of improvement in symptoms after 48 hours of appropriate antibiotic therapy and requires further evaluation with urological imaging. Patients with complicated UTIs can present directly with bacteremia, sepsis, multiple organ system failure, or acute renal failure.
Deterrence and Patient Education
Several preventive measures are recommended to reduce further recurrences of UTIs, although the proven benefit is marginal. Patients should be advised to increase fluid intake to at least 2 liters daily. In a study on 140 women, increased water intake resulted in decreased incidence of cystitis episodes by 1.5 (95% CI, 1.2-1.8) (mean 1.7 versus 3.2) episodes.[82]
Topical vaginal estrogen is recommended in women who are postmenopausal with vulvovaginal atrophy (ie, genitourinary syndrome of menopause) to reduce the risk of future UTIs, provided no contraindications are noted. Other behavioral modifications include wiping from front to back, using clean liquid soap, avoiding reusable luffas and sponges for soap application when bathing, and early postcoital voiding.[83] Evidence is inconclusive about the beneficial role of cranberry juice in reducing episodes of recurrent UTI.[84]
Antibiotic prophylaxis should be offered only after other preventive modalities and only in women with a confirmed diagnosis of recurrent cystitis. In some situations, the adverse effects of antibiotic prophylaxis may outweigh the risk of recurrent UTIs, as cystitis rarely results in a poor outcome. These may include direct drug toxicity, development of resistance, alteration of the microbiome, and Clostridioides difficile infection.
In women with cystitis episodes associated with sexual activity, postcoital antibiotics may be advised to reduce the risk of adverse effects without compromising the drug’s efficacy or promoting antibiotic resistance.[74] In other cases, continuous prophylaxis is recommended. The drugs prescribed in continuous and postcoital prophylaxis are largely similar. The need for antibiotic prophylaxis should be reevaluated after 6 months.
Summary of Personal Hygiene Recommendations
In many women, recurrent UTIs are caused by inadequate or suboptimal personal hygiene. Controlled studies have not proven significant efficacy in reducing recurrent UTIs from lifestyle modifications. Patient education from female clinicians may be more accepted by female patients who feel uncomfortable hearing this advice from male clinicians.[13][32]
The following information reviews the recommendations for conservative management that clinicians should encourage patients to practice:
- Proper wiping practices
- Wash hands before wiping: Patients should wash their hands before urinating or using the toilet. They should also wash their hands before they get into the shower to avoid passing germs from their hands back to their body near the vaginal area.
- Wipe front to back: Always wipe from the front to the back after urinating. The patient should start from the front and push down and away towards the rectum. Most urinary infections are from bacteria that normally live around the rectum and anus. Therefore, any wiping motion that starts near the rectum and then approaches the urethral area will move potentially dangerous bacteria closer to the bladder and urinary tract. Patients should also wipe the same way, front to back, after a bowel movement.
- When wiping, only wipe once: Using toilet paper after urination is acceptable. However, the patient must wipe once, or they may add more bacteria to the urethral area. Sterile baby wipes are cleaner than toilet paper and can be carried in their purse outside the home. As a general rule, anything safe for babies can also be utilized in the delicate area around the vagina and urethral opening.
- Bathing practices
- Avoid baths: Bathwater is full of dirt and bacteria from the skin. Sitting in a tub allows the bacteria to reach the urethra. Remind the patient that the water they wouldn’t drink shouldn’t be used to clean their urethra. If a patient absolutely must take a bath instead of a shower, they should avoid any bubble baths or other cosmetic bath additives, which tend to be irritating to the delicate skin of the vaginal mucosa. Instruct the patient to take showers instead.
- Avoid luffas and all reusable sponges: Luffas and other reusable sponges, including nylon, cannot be adequately cleaned or sterilized, so they retain bacteria. They are also utilized repeatedly for days, weeks, or months, during which they can accumulate more and more bacteria and germs. Women susceptible to infections, particularly UTIs, should avoid using reusable items that are heavily contaminated.
- Use a gentle liquid soap when washing: Bar soap will always have bacteria due to exposure to the air and bathroom environment. A body wash is fine for regular skin cleaning, but regular body wash is too harsh for the gentle tissue of the vagina and urethral area. Avoid using products with unnecessary perfumes, astringents, creams, or other irritating chemicals. The patient may use gentle baby soap or shampoo for the urethral area.
- Use washcloths: The best and cleanest way to apply soap is to use a clean, soft cotton or microfiber washcloth. The washcloths can be placed into a clean, resealable plastic bag immediately after they are washed and dried, as they are cleanest from the dryer. The patient may want a second washcloth to finish their shower after adequately cleaning the urethral area.
- Clean the urethral area first: Without proper cleaning, the bladder is the only body area that could become infected. The bladder should be washed before a washcloth or hands pick up dirt, germs, or bacteria from other body parts. When surgeons perform surgery, they clean the surgical site before moving to the surrounding area. The same principle applies to cleaning the bladder area.
- How to wash: Hands should be washed before showering. Wet the washcloth, add some clean liquid soap, and wipe the urethral area first with a single front-to-back wipe. Rinse well without directly spraying the area. The washcloth to clean the urethral area should be used only once before laundering and not for any other purpose.
- Douches and other personal hygiene products: In most cases, a vinegar and water douche or a douche with iodine or benzalkonium chloride is helpful if carried out correctly at appropriate intervals. The patient should not use any feminine hygiene sprays, cosmetics, perfumes, medicated towelettes, or similar products in the vagina or urethral area unless approved by the clinician.
- Use tampons for periods: Tampons are advised rather than sanitary napkins or pads during menstrual periods. Compared to a sanitary pad, a tampon can help maintain better hygiene and reduce bacterial growth.
- Avoid long intervals between urinations: The patient should try to empty their bladder every 4 hours during the day, even if they don’t feel the urge to void. If possible, the urge to void should be promptly answered.
- Don’t wear tight clothes: Patients should avoid wearing pantyhose, bathing suits, or tight slacks for prolonged periods. All of these can cause the skin around the vagina to fold into the body, introducing more bacteria around the urethra.
- Dietary modifications
- Drink more water: Recommend starting with 1 extra glass with each meal. If the patient’s urine appears any darker than a very pale yellow, this could mean that they are not drinking enough and should increase their fluid intake. Cranberry juice is helpful in patients with UTIs but can be substituted with other beverages.
- Take vitamin C and drink cranberry juice: Recommend additional vitamin C. This may help increase the body’s resistance to infection. Extra vitamin C that the system cannot use immediately is released into the urine, which blocks bacterial growth. As noted earlier, cranberry juice or pills may be of benefit in reducing UTIs.
- Avoid irritating foods like caffeine: Symptoms of bladder irritation may be aggravated by caffeine, regular coffee, tea, alcohol, “hot” spices, aspartame, chocolate, cola drinks, and high-potassium foods like bananas and oranges.
- Lifestyle modifications
- Avoid activities that increase the risk of bladder infections: Prolonged bicycling, motorcycling, horseback riding, and similar physical activities and exercises may increase the risk of bladder infections. When engaging in physical activity and exercise, patients should frequently empty their bladders and drink plenty of water and other fluids. Sexual activity may also increase the risk.
- Take special precautions after sexual activity: After intercourse, instruct the patient to empty their bladder and drink 2 extra glasses of water. After sexual activity, clinicians may advise some patients to take a urinary antiseptic or antibiotic.
- Medications
- An estrogen vaginal cream may increase resistance to bladder infections: Clinicians may suggest an estrogen cream for the vagina if the patient is in menopause. The vaginal cream will help keep the tissues around the urethra healthy and more resistant to infection.
- Take antibiotics only as prescribed: If the clinician has prescribed medication or antibiotics as prophylaxis, patients should follow their instructions carefully. They must be aware that medications may be necessary for up to 1 year or more, depending on the nature and severity of the UTI. For some patients, a small amount of a urinary antibiotic or antiseptic taken daily at bedtime will prevent most urinary infections, give the bladder a chance to heal, and restore the natural resistance. Other patients may only need antibiotics when they think they are getting an infection.
If patients follow these suggestions and still get an infection, they should seek medical help promptly if they have an infection. A clinician typically requests a urine specimen. Patients should seek prompt help for excessive vaginal discharge or other signs of vaginal inflammation and infection. Patients may begin an antibiotic at this time, and compliance is crucial. Sometimes, the clinician may request additional tests such as kidney x-rays or a direct bladder examination with a telescope (cystoscopy). Sterilization of washcloths may be the next step where more straightforward measures are inadequate.
Sterilizing Washcloths for Home Use
The clinician may recommend sterilizing washcloths for washing and personal hygiene to help prevent recurrent UTIs. This extra step is probably unnecessary for most patients with recurrent infections but can benefit the more severe or resistant cases. Patients should use only those washcloths purchased for this purpose and remember to wipe correctly from front to back. The following are recommended steps for sterilization:
- Wash the washcloths with hot water and soap or detergent. If the patient doesn’t have a washer, they can use soap and hot water in a sink.
- Boil the washcloths in water for at least 20 minutes.
- Take the washcloths out of the water and allow them to dry, or use the clothes dryer.
- When dry, place each washcloth in a separate, sealable, microwave-safe plastic bag such as a ziplock bag.
- Leave the bags open and unsealed.
- Place the bags in the microwave. In the center of the microwave, put a large glass of cold water. The washcloths should not be placed in the water.
- Put the microwave on high for 5 minutes. Replace the glass of cold water (now very hot) with a new glass of cold water and microwave on high for 5 minutes.
- Let the bags cool, then close them. The washcloths are now sterile inside a sterile bag.
This technique kills the germs and bacteria on the washcloths by sterilizing them with microwave radiation. Without the glass of cold water to absorb the heat, the bags would melt, and the washcloths would catch fire.
Pearls and Other Issues
Consider using fosfomycin or pivmecillinam in patients with a history of multidrug-resistant or ESBL-producing infections or when urine cultures show microorganisms. Also, consider intermittent intravesical therapy with gentamicin solution in otherwise intractable cases or for patients with end-stage renal failure.[34][35][37][38][57][58][59]
Experimentally, vaccines to reduce the recurrence of UTIs have been developed from whole bacterial cells. Most have been at least marginally successful, but the beneficial effect disappears after just a few weeks.[85][86] Sublingual mucosal polybacterial vaccines were recently studied in immunocompromised patients and provided promising results in reducing recurrent infections.[87] A bioconjugate vaccine from various E. coli genotypes works better and has a longer-lasting effect. Yet, another promising experimental vaccine focuses on E. coli type 1 fimbrial adhesion protein.[54]
MV140 is an oral vaccine for the prophylaxis of recurrent UTIs that has shown good efficacy over 9 years in a preliminary study and is now clinically available in many countries but not the US or Canada.[63][65][66][67][69] The vaccine should be considered if available. Pilicides and mannosides are also designed to interfere with bacterial adhesion to the urothelium and may be particularly useful in patients with chronic Foley catheters.[88] Another approach uses oral immunostimulants for E coli. This therapy is already commercially available in Europe but not the US and has demonstrated a reduction in E coli recurrences of 95%.[89]
Nonsteroidal anti-inflammatory agents to modify host defenses are being studied experimentally to reduce recurrent UTIs.[90][91] Fecal microbiota transfer, which transplants metabolites and microorganisms from the fecal material of a healthy donor, appears promising, and bacteriophage therapy, which targets pathogenic bacteria with specific viruses, is also being explored as a possible therapy in the future.[71]
Summary of Preventing Infections
A summary of key practices to prevent urinary infections include:
- Wipe in the correct direction, from front to back.
- Wash hands before using washcloths, tissues, or toilet paper for wiping or washing.
- Use a clean, gentle liquid soap because that is cleaner than bar soap.
- Only wipe once with each washcloth or tissue.
- When washing, clean the bladder area first to prevent bacteria contamination from other body parts.
- Don’t use these washcloths for anything except to clean the area around the urethra.
- Drink extra water and take vitamin C. Drink cranberry juice or take cranberry pills.
- Consider using an estrogen cream twice a week (or as prescribed by the clinician) if postmenopausal.
Enhancing Healthcare Team Outcomes
Effective management of recurrent UTIs requires an interprofessional approach, where healthcare professionals collaborate to provide patient-centered care, enhance outcomes, and ensure safety. Physicians and advanced practitioners serve as the primary point of contact, conducting thorough history-taking, physical exams, and initiating diagnostic tests like urinalyses and urine cultures. Collaboration with specialists such as urologists, infectious disease experts, and radiologists is essential for evaluating complex cases, particularly when urinary obstruction or atypical presentations are suspected. Obstetricians may manage cases involving pregnant patients, where symptoms can overlap with obstetrical pain.
Nurses play a pivotal role in monitoring vital signs, educating patients and families, and supporting adherence to treatment plans. Pharmacists contribute by ensuring appropriate antibiotic selection, preventing resistance, and managing medication safety. Clear interprofessional communication is vital to bridging gaps in symptom perception and addressing misconceptions, fostering patient trust, and empowering patients to engage in their care. In select cases, motivated and reliable patients may benefit from self-diagnosis and treatment under professional guidance, streamlining care while maintaining efficacy. By coordinating efforts and sharing case information, the team ensures timely, accurate treatment while avoiding unnecessary interventions, promoting optimal outcomes and team performance.
Media
(Click Image to Enlarge)
References
Aydin A, Ahmed K, Zaman I, Khan MS, Dasgupta P. Recurrent urinary tract infections in women. International urogynecology journal. 2015 Jun:26(6):795-804. doi: 10.1007/s00192-014-2569-5. Epub 2014 Nov 20 [PubMed PMID: 25410372]
Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. The American journal of medicine. 2002 Jul 8:113 Suppl 1A():5S-13S [PubMed PMID: 12113866]
Anger J, Lee U, Ackerman AL, Chou R, Chughtai B, Clemens JQ, Hickling D, Kapoor A, Kenton KS, Kaufman MR, Rondanina MA, Stapleton A, Stothers L, Chai TC. Recurrent Uncomplicated Urinary Tract Infections in Women: AUA/CUA/SUFU Guideline. The Journal of urology. 2019 Aug:202(2):282-289. doi: 10.1097/JU.0000000000000296. Epub 2019 Jul 8 [PubMed PMID: 31042112]
Hooton TM, Roberts PL, Cox ME, Stapleton AE. Voided midstream urine culture and acute cystitis in premenopausal women. The New England journal of medicine. 2013 Nov 14:369(20):1883-91. doi: 10.1056/NEJMoa1302186. Epub [PubMed PMID: 24224622]
Mody L, Juthani-Mehta M. Urinary tract infections in older women: a clinical review. JAMA. 2014 Feb 26:311(8):844-54. doi: 10.1001/jama.2014.303. Epub [PubMed PMID: 24570248]
Bono MJ, Leslie SW, Reygaert WC. Uncomplicated Urinary Tract Infections. StatPearls. 2025 Jan:(): [PubMed PMID: 29261874]
Lo E, Nicolle LE, Coffin SE, Gould C, Maragakis LL, Meddings J, Pegues DA, Pettis AM, Saint S, Yokoe DS. Strategies to prevent catheter-associated urinary tract infections in acute care hospitals: 2014 update. Infection control and hospital epidemiology. 2014 May:35(5):464-79. doi: 10.1086/675718. Epub [PubMed PMID: 24709715]
Larcombe J. Urinary tract infection in children: recurrent infections. BMJ clinical evidence. 2015 Jun 12:2015():. pii: 0306. Epub 2015 Jun 12 [PubMed PMID: 26067232]
Lotfollahzadeh S, Leslie SW, Aeddula NR. Vesicoureteral Reflux. StatPearls. 2025 Jan:(): [PubMed PMID: 33085409]
Meštrović T, Matijašić M, Perić M, Čipčić Paljetak H, Barešić A, Verbanac D. The Role of Gut, Vaginal, and Urinary Microbiome in Urinary Tract Infections: From Bench to Bedside. Diagnostics (Basel, Switzerland). 2020 Dec 22:11(1):. doi: 10.3390/diagnostics11010007. Epub 2020 Dec 22 [PubMed PMID: 33375202]
Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, Moran GJ, Nicolle LE, Raz R, Schaeffer AJ, Soper DE, Infectious Diseases Society of America, European Society for Microbiology and Infectious Diseases. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2011 Mar 1:52(5):e103-20. doi: 10.1093/cid/ciq257. Epub [PubMed PMID: 21292654]
Level 1 (high-level) evidenceHooton TM, Roberts PL, Stamm WE. Effects of recent sexual activity and use of a diaphragm on the vaginal microflora. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 1994 Aug:19(2):274-8 [PubMed PMID: 7986899]
Scholes D, Hawn TR, Roberts PL, Li SS, Stapleton AE, Zhao LP, Stamm WE, Hooton TM. Family history and risk of recurrent cystitis and pyelonephritis in women. The Journal of urology. 2010 Aug:184(2):564-9. doi: 10.1016/j.juro.2010.03.139. Epub 2010 Jun 19 [PubMed PMID: 20639019]
Level 2 (mid-level) evidenceZhong YH, Fang Y, Zhou JZ, Tang Y, Gong SM, Ding XQ. Effectiveness and safety of patient initiated single-dose versus continuous low-dose antibiotic prophylaxis for recurrent urinary tract infections in postmenopausal women: a randomized controlled study. The Journal of international medical research. 2011:39(6):2335-43 [PubMed PMID: 22289552]
Level 1 (high-level) evidenceGlover M, Moreira CG, Sperandio V, Zimmern P. Recurrent urinary tract infections in healthy and nonpregnant women. Urological science. 2014 Mar:25(1):1-8 [PubMed PMID: 27499825]
Bent S, Nallamothu BK, Simel DL, Fihn SD, Saint S. Does this woman have an acute uncomplicated urinary tract infection? JAMA. 2002 May 22-29:287(20):2701-10 [PubMed PMID: 12020306]
Pat JJ, Steffens MG, Witte LPW, Marcelissen TAT, Blanker MH. Comparison of the diagnostic yield of routine versus indicated flowmetry, ultrasound and cystoscopy in women with recurrent urinary tract infections. International urogynecology journal. 2022 Aug:33(8):2283-2289. doi: 10.1007/s00192-021-04871-2. Epub 2021 Jun 14 [PubMed PMID: 34125244]
Stein R, Dogan HS, Hoebeke P, Kočvara R, Nijman RJ, Radmayr C, Tekgül S, European Association of Urology, European Society for Pediatric Urology. Urinary tract infections in children: EAU/ESPU guidelines. European urology. 2015 Mar:67(3):546-58. doi: 10.1016/j.eururo.2014.11.007. Epub 2014 Dec 2 [PubMed PMID: 25477258]
Bremnor JD, Sadovsky R. Evaluation of dysuria in adults. American family physician. 2002 Apr 15:65(8):1589-96 [PubMed PMID: 11989635]
Lim Y, Leslie SW, O'Rourke S. Interstitial Cystitis/Bladder Pain Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 34033350]
Mehta P, Leslie SW, Reddivari AKR. Dysuria. StatPearls. 2025 Jan:(): [PubMed PMID: 31751108]
Lawrentschuk N, Ooi J, Pang A, Naidu KS, Bolton DM. Cystoscopy in women with recurrent urinary tract infection. International journal of urology : official journal of the Japanese Urological Association. 2006 Apr:13(4):350-3 [PubMed PMID: 16734849]
Level 2 (mid-level) evidenceArnold JJ, Hehn LE, Klein DA. Common Questions About Recurrent Urinary Tract Infections in Women. American family physician. 2016 Apr 1:93(7):560-9 [PubMed PMID: 27035041]
Siff LN, Unger CA, Jelovsek JE, Paraiso MF, Ridgeway BM, Barber MD. Assessing ureteral patency using 10% dextrose cystoscopy fluid: evaluation of urinary tract infection rates. American journal of obstetrics and gynecology. 2016 Jul:215(1):74.e1-6. doi: 10.1016/j.ajog.2016.02.006. Epub 2016 Feb 12 [PubMed PMID: 26875949]
Barry HC, Hickner J, Ebell MH, Ettenhofer T. A randomized controlled trial of telephone management of suspected urinary tract infections in women. The Journal of family practice. 2001 Jul:50(7):589-94 [PubMed PMID: 11485707]
Level 1 (high-level) evidenceGraninger W. Pivmecillinam--therapy of choice for lower urinary tract infection. International journal of antimicrobial agents. 2003 Oct:22 Suppl 2():73-8 [PubMed PMID: 14527775]
Hawser S, Morrissey I, Kothari N, Monti F, Henriksen AS. Activity of mecillinam against USA urinary tract clinical isolates from 2017 to 2020 including isolates resistant to comparator antibiotics. Journal of global antimicrobial resistance. 2024 Dec:39():137-143. doi: 10.1016/j.jgar.2024.08.013. Epub 2024 Sep 13 [PubMed PMID: 39278462]
Lodise TP, Kaye KS, Santerre Henriksen A, Kahlmeter G. Review of the In Vitro Microbiological Activity of Mecillinam Against Common Uropathogens in Uncomplicated Urinary Tract Infection: Focus on Resistant Pathogens. Open forum infectious diseases. 2024 Jun:11(6):ofae296. doi: 10.1093/ofid/ofae296. Epub 2024 May 24 [PubMed PMID: 38868308]
Montelin H, Camporeale A, Hallgren A, Angelin M, Hogvall J, Östholm Balkhed Å, Vading M, Giske CG, Tängdén T, Swedish ESBL study group. Treatment, outcomes and characterization of pathogens in urinary tract infections caused by ESBL-producing Enterobacterales: a prospective multicentre study. The Journal of antimicrobial chemotherapy. 2024 Mar 1:79(3):531-538. doi: 10.1093/jac/dkad402. Epub [PubMed PMID: 38197416]
Frimodt-Møller N, Bjerrum L. Treating urinary tract infections in the era of antibiotic resistance. Expert review of anti-infective therapy. 2023 Jul-Dec:21(12):1301-1308. doi: 10.1080/14787210.2023.2279104. Epub 2023 Nov 24 [PubMed PMID: 37922147]
Frimodt-Møller N, Simonsen GS, Larsen AR, Kahlmeter G. Pivmecillinam, the paradigm of an antibiotic with low resistance rates in Escherichia coli urine isolates despite high consumption. The Journal of antimicrobial chemotherapy. 2022 Dec 23:78(1):289-295. doi: 10.1093/jac/dkac396. Epub [PubMed PMID: 36441168]
Zhanel GG, Hisanaga TL, Laing NM, DeCorby MR, Nichol KA, Weshnoweski B, Johnson J, Noreddin A, Low DE, Karlowsky JA, NAUTICA Group, Hoban DJ. Antibiotic resistance in Escherichia coli outpatient urinary isolates: final results from the North American Urinary Tract Infection Collaborative Alliance (NAUTICA). International journal of antimicrobial agents. 2006 Jun:27(6):468-75 [PubMed PMID: 16713191]
Kahlmeter G. Prevalence and antimicrobial susceptibility of pathogens in uncomplicated cystitis in Europe. The ECO.SENS study. International journal of antimicrobial agents. 2003 Oct:22 Suppl 2():49-52 [PubMed PMID: 14527771]
Cameron AP, Castrodad PM, Troost J, Forchheimer M, Tate DG. Effectiveness and patient perspective on the use of intravesical gentamicin instillations to treat recurrent urinary tract infections in neurogenic lower urinary tract dysfunction. Neurourology and urodynamics. 2024 Nov:43(8):1916-1923. doi: 10.1002/nau.25513. Epub 2024 Jun 11 [PubMed PMID: 38860440]
Level 3 (low-level) evidenceReddy M, Zimmern PE. Efficacy of antimicrobial intravesical treatment for uncomplicated recurrent urinary tract infections: a systematic review. International urogynecology journal. 2022 May:33(5):1125-1143. doi: 10.1007/s00192-021-05042-z. Epub 2022 Jan 4 [PubMed PMID: 34982189]
Level 1 (high-level) evidenceZiadeh T, Chebel R, Labaki C, Saliba G, Helou EE. Bladder instillation for urinary tract infection prevention in neurogenic bladder patients practicing clean intermittent catheterization: A systematic review. Urologia. 2022 May:89(2):261-267. doi: 10.1177/03915603211049883. Epub 2021 Oct 6 [PubMed PMID: 34612750]
Level 1 (high-level) evidenceChernyak S, Salamon C. Intravesical Antibiotic Administration in the Treatment of Recurrent Urinary Tract Infections: Promising Results From a Case Series. Female pelvic medicine & reconstructive surgery. 2020 Feb:26(2):152-154. doi: 10.1097/SPV.0000000000000810. Epub [PubMed PMID: 31990805]
Level 2 (mid-level) evidenceHuen KH, Nik-Ahd F, Chen L, Lerman S, Singer J. Neomycin-polymyxin or gentamicin bladder instillations decrease symptomatic urinary tract infections in neurogenic bladder patients on clean intermittent catheterization. Journal of pediatric urology. 2019 Apr:15(2):178.e1-178.e7. doi: 10.1016/j.jpurol.2018.12.001. Epub 2018 Dec 12 [PubMed PMID: 30611650]
Yamashita K, Ishiyama Y, Yoshino M, Tachibana H, Toki D, Konda R, Kondo T. Urinary Tract Infection in Hemodialysis-Dependent End-Stage Renal Disease Patients. Research and reports in urology. 2022:14():7-15. doi: 10.2147/RRU.S346020. Epub 2022 Jan 16 [PubMed PMID: 35079597]
Behzadi P, Urbán E, Matuz M, Benkő R, Gajdács M. The Role of Gram-Negative Bacteria in Urinary Tract Infections: Current Concepts and Therapeutic Options. Advances in experimental medicine and biology. 2021:1323():35-69. doi: 10.1007/5584_2020_566. Epub [PubMed PMID: 32596751]
Level 3 (low-level) evidenceBono MJ, Leslie SW, Doerr C. Uncomplicated Urinary Tract Infections (Nursing). StatPearls. 2025 Jan:(): [PubMed PMID: 33760460]
Scholes D, Hooton TM, Roberts PL, Stapleton AE, Gupta K, Stamm WE. Risk factors for recurrent urinary tract infection in young women. The Journal of infectious diseases. 2000 Oct:182(4):1177-82 [PubMed PMID: 10979915]
Level 2 (mid-level) evidenceCooper TE, Teng C, Howell M, Teixeira-Pinto A, Jaure A, Wong G. D-mannose for preventing and treating urinary tract infections. The Cochrane database of systematic reviews. 2022 Aug 30:8(8):CD013608. doi: 10.1002/14651858.CD013608.pub2. Epub 2022 Aug 30 [PubMed PMID: 36041061]
Level 1 (high-level) evidenceBarrons R, Tassone D. Use of Lactobacillus probiotics for bacterial genitourinary infections in women: a review. Clinical therapeutics. 2008 Mar:30(3):453-68. doi: 10.1016/j.clinthera.2008.03.013. Epub [PubMed PMID: 18405785]
Barea BM, Veeratterapillay R, Harding C. Nonantibiotic treatments for urinary cystitis: an update. Current opinion in urology. 2020 Nov:30(6):845-852. doi: 10.1097/MOU.0000000000000821. Epub [PubMed PMID: 33009152]
Level 3 (low-level) evidenceSong G, Koro M, Leung V, Loh G. Literature Review of Ascorbic Acid, Cranberry, and D-mannose for Urinary Tract Infection Prophylaxis in Older People. The Senior care pharmacist. 2023 Aug 1:38(8):315-328. doi: 10.4140/TCP.n.2023.315. Epub [PubMed PMID: 37496168]
Kranjčec B, Papeš D, Altarac S. D-mannose powder for prophylaxis of recurrent urinary tract infections in women: a randomized clinical trial. World journal of urology. 2014 Feb:32(1):79-84. doi: 10.1007/s00345-013-1091-6. Epub 2013 Apr 30 [PubMed PMID: 23633128]
Level 1 (high-level) evidenceHayward G, Mort S, Hay AD, Moore M, Thomas NPB, Cook J, Robinson J, Williams N, Maeder N, Edeson R, Franssen M, Grabey J, Glogowska M, Yang Y, Allen J, Butler CC. d-Mannose for Prevention of Recurrent Urinary Tract Infection Among Women: A Randomized Clinical Trial. JAMA internal medicine. 2024 Jun 1:184(6):619-628. doi: 10.1001/jamainternmed.2024.0264. Epub [PubMed PMID: 38587819]
Level 1 (high-level) evidenceWagenlehner F, Lorenz H, Ewald O, Gerke P. Why d-Mannose May Be as Efficient as Antibiotics in the Treatment of Acute Uncomplicated Lower Urinary Tract Infections-Preliminary Considerations and Conclusions from a Non-Interventional Study. Antibiotics (Basel, Switzerland). 2022 Feb 25:11(3):. doi: 10.3390/antibiotics11030314. Epub 2022 Feb 25 [PubMed PMID: 35326777]
Li JM, Cosler LE, Harausz EP, Myers CE, Kufel WD. Methenamine for urinary tract infection prophylaxis: A systematic review. Pharmacotherapy. 2024 Feb:44(2):197-206. doi: 10.1002/phar.2895. Epub 2023 Nov 28 [PubMed PMID: 37986168]
Level 1 (high-level) evidenceStair SL, Palmer CJ, Lee UJ. Evidence-based review of nonantibiotic urinary tract infection prevention strategies for women: a patient-centered approach. Current opinion in urology. 2023 May 1:33(3):187-192. doi: 10.1097/MOU.0000000000001082. Epub 2023 Mar 2 [PubMed PMID: 36862100]
Level 3 (low-level) evidenceVenturini S, Reffo I, Avolio M, Basaglia G, Del Fabro G, Callegari A, Tonizzo M, Sabena A, Rondinella S, Mancini W, Conte C, Crapis M. The Management of Recurrent Urinary Tract Infection: Non-Antibiotic Bundle Treatment. Probiotics and antimicrobial proteins. 2024 Oct:16(5):1857-1865. doi: 10.1007/s12602-023-10141-y. Epub 2023 Aug 16 [PubMed PMID: 37584833]
Chen YC, Lee WC, Chuang YC. Emerging Non-Antibiotic Options Targeting Uropathogenic Mechanisms for Recurrent Uncomplicated Urinary Tract Infection. International journal of molecular sciences. 2023 Apr 11:24(8):. doi: 10.3390/ijms24087055. Epub 2023 Apr 11 [PubMed PMID: 37108218]
Eldridge GR, Hughey H, Rosenberger L, Martin SM, Shapiro AM, D'Antonio E, Krejci KG, Shore N, Peterson J, Lukes AS, Starks CM. Safety and immunogenicity of an adjuvanted Escherichia coli adhesin vaccine in healthy women with and without histories of recurrent urinary tract infections: results from a first-in-human phase 1 study. Human vaccines & immunotherapeutics. 2021 May 4:17(5):1262-1270. doi: 10.1080/21645515.2020.1834807. Epub 2020 Dec 16 [PubMed PMID: 33325785]
Huttner A, Hatz C, van den Dobbelsteen G, Abbanat D, Hornacek A, Frölich R, Dreyer AM, Martin P, Davies T, Fae K, van den Nieuwenhof I, Thoelen S, de Vallière S, Kuhn A, Bernasconi E, Viereck V, Kavvadias T, Kling K, Ryu G, Hülder T, Gröger S, Scheiner D, Alaimo C, Harbarth S, Poolman J, Fonck VG. Safety, immunogenicity, and preliminary clinical efficacy of a vaccine against extraintestinal pathogenic Escherichia coli in women with a history of recurrent urinary tract infection: a randomised, single-blind, placebo-controlled phase 1b trial. The Lancet. Infectious diseases. 2017 May:17(5):528-537. doi: 10.1016/S1473-3099(17)30108-1. Epub 2017 Feb 24 [PubMed PMID: 28238601]
Level 1 (high-level) evidencePrattley S, Geraghty R, Moore M, Somani BK. Role of Vaccines for Recurrent Urinary Tract Infections: A Systematic Review. European urology focus. 2020 May 15:6(3):593-604. doi: 10.1016/j.euf.2019.11.002. Epub 2019 Dec 2 [PubMed PMID: 31806578]
Level 1 (high-level) evidencePatel D. Intravesical Therapies for Recurrent Urinary Tract Infections: A Systematic Review. Cureus. 2024 Oct:16(10):e72175. doi: 10.7759/cureus.72175. Epub 2024 Oct 23 [PubMed PMID: 39507191]
Level 1 (high-level) evidenceOchoa DC, Healy R. Intravesical Agents for Prevention of Recurrent Urinary Tract Infections. European urology focus. 2024 Sep:10(5):726-730. doi: 10.1016/j.euf.2024.08.001. Epub 2024 Aug 19 [PubMed PMID: 39164132]
Andretta E, Longo R, Balladelli M, Sgarabotto C, Sgarabotto D. Intravesical Gentamicin: An Option for Therapy and Prophylaxis against Recurrent UTIs and Resistant Bacteria in Neurogenic Bladder Patients on Intermittent Catheterization. Antibiotics (Basel, Switzerland). 2022 Sep 30:11(10):. doi: 10.3390/antibiotics11101335. Epub 2022 Sep 30 [PubMed PMID: 36289993]
Moussa M, Chakra MA, Papatsoris AG, Dellis A, Dabboucy B, Fares Y. Bladder irrigation with povidone-iodine prevent recurrent urinary tract infections in neurogenic bladder patients on clean intermittent catheterization. Neurourology and urodynamics. 2021 Feb:40(2):672-679. doi: 10.1002/nau.24607. Epub 2021 Jan 21 [PubMed PMID: 33476092]
Miles BJ, Skoog S. Treatment of malakoplakia of bladder with intravesical neosporin irrigation. Urology. 1986 Jan:27(1):32-3 [PubMed PMID: 3001994]
Level 3 (low-level) evidenceBenito-Villalvilla C, Cirauqui C, Diez-Rivero CM, Casanovas M, Subiza JL, Palomares O. MV140, a sublingual polyvalent bacterial preparation to treat recurrent urinary tract infections, licenses human dendritic cells for generating Th1, Th17, and IL-10 responses via Syk and MyD88. Mucosal immunology. 2017 Jul:10(4):924-935. doi: 10.1038/mi.2016.112. Epub 2016 Dec 14 [PubMed PMID: 27966556]
Kovacic J, Canagasingham A, Zhong W, Lockhart K, Dhar A, Shepherd A, Chung A. Evaluation of MV140 in preventing recurrent urinary tract infections: a multicentre double-blind randomized controlled trial protocol. BJU international. 2024 Apr:133 Suppl 4():37-43. doi: 10.1111/bju.16247. Epub 2023 Dec 26 [PubMed PMID: 38060333]
Level 1 (high-level) evidenceGupta K, Hooton TM, Roberts PL, Stamm WE. Patient-initiated treatment of uncomplicated recurrent urinary tract infections in young women. Annals of internal medicine. 2001 Jul 3:135(1):9-16 [PubMed PMID: 11434727]
Ramírez-Sevilla C, Gómez-Lanza E, Llopis-Manzanera J, Cetina-Herrando A, Puyol-Pallàs JM. Effectiveness and health cost analysis between immunoprophylaxis with MV140 autovaccine, MV140 vaccine and continuous treatment with antibiotics to prevent recurrent urinary tract infections. Actas urologicas espanolas. 2023 Jan-Feb:47(1):27-33. doi: 10.1016/j.acuroe.2022.08.016. Epub 2022 Aug 12 [PubMed PMID: 36470711]
. Sublingual MV140 for Prevention of Recurrent Urinary Tract Infections. NEJM evidence. 2022 May:1(5):EVIDx2200081. doi: 10.1056/EVIDx2200081. Epub 2022 Mar 7 [PubMed PMID: 38319208]
Nickel JC, Doiron RC. An Effective Sublingual Vaccine, MV140, Safely Reduces Risk of Recurrent Urinary Tract Infection in Women. Pathogens (Basel, Switzerland). 2023 Feb 21:12(3):. doi: 10.3390/pathogens12030359. Epub 2023 Feb 21 [PubMed PMID: 36986281]
Lorenzo-Gómez MF, Foley S, Nickel JC, García-Cenador MB, Padilla-Fernández BY, González-Casado I, Martínez-Huélamo M, Yang B, Blick C, Ferreira F, Caballero R, Saz-Leal P, Casanovas M. Sublingual MV140 for Prevention of Recurrent Urinary Tract Infections. NEJM evidence. 2022 Apr:1(4):EVIDoa2100018. doi: 10.1056/EVIDoa2100018. Epub 2022 Jan 21 [PubMed PMID: 38319200]
Saz-Leal P, Ligon MM, Diez-Rivero CM, García-Ayuso D, Mohanty S, Conejero L, Brauner A, Subiza JL, Mysorekar IU. MV140 mucosal bacterial vaccine improves uropathogenic E. coli clearance in an experimental model of urinary tract infection. Research square. 2023 Jun 7:():. pii: rs.3.rs-2992611. doi: 10.21203/rs.3.rs-2992611/v1. Epub 2023 Jun 7 [PubMed PMID: 37333312]
Martín-Cruz L, Angelina A, Baydemir I, Bulut Ö, Subiza JL, Netea MG, Domínguez-Andrés J, Palomares O. Candida albicans V132 induces trained immunity and enhances the responses triggered by the polybacterial vaccine MV140 for genitourinary tract infections. Frontiers in immunology. 2022:13():1066383. doi: 10.3389/fimmu.2022.1066383. Epub 2022 Nov 24 [PubMed PMID: 36505433]
Zare M, Vehreschild MJGT, Wagenlehner F. Management of uncomplicated recurrent urinary tract infections. BJU international. 2022 Jun:129(6):668-678. doi: 10.1111/bju.15630. Epub 2021 Nov 17 [PubMed PMID: 34741796]
Albert X, Huertas I, Pereiró II, Sanfélix J, Gosalbes V, Perrota C. Antibiotics for preventing recurrent urinary tract infection in non-pregnant women. The Cochrane database of systematic reviews. 2004:2004(3):CD001209 [PubMed PMID: 15266443]
Level 1 (high-level) evidenceSmith AL, Brown J, Wyman JF, Berry A, Newman DK, Stapleton AE. Treatment and Prevention of Recurrent Lower Urinary Tract Infections in Women: A Rapid Review with Practice Recommendations. The Journal of urology. 2018 Dec:200(6):1174-1191. doi: 10.1016/j.juro.2018.04.088. Epub 2018 Jun 22 [PubMed PMID: 29940246]
Jodal U, Larsson P, Hansson S, Bauer CA. Pivmecillinam in long-term prophylaxis to girls with recurrent urinary tract infection. Scandinavian journal of infectious diseases. 1989:21(3):299-302 [PubMed PMID: 2756342]
Al-Badr A, Al-Shaikh G. Recurrent Urinary Tract Infections Management in Women: A review. Sultan Qaboos University medical journal. 2013 Aug:13(3):359-67 [PubMed PMID: 23984019]
Taich L, Zhao H, Cordero C, Anger JT. New paradigms in the management of recurrent urinary tract infections. Current opinion in urology. 2020 Nov:30(6):833-837. doi: 10.1097/MOU.0000000000000823. Epub [PubMed PMID: 32941258]
Level 3 (low-level) evidenceMarschall J, Carpenter CR, Fowler S, Trautner BW, CDC Prevention Epicenters Program. Antibiotic prophylaxis for urinary tract infections after removal of urinary catheter: meta-analysis. BMJ (Clinical research ed.). 2013 Jun 11:346():f3147. doi: 10.1136/bmj.f3147. Epub 2013 Jun 11 [PubMed PMID: 23757735]
Level 1 (high-level) evidenceFisher H, Oluboyede Y, Chadwick T, Abdel-Fattah M, Brennand C, Fader M, Harrison S, Hilton P, Larcombe J, Little P, McClurg D, McColl E, N'Dow J, Ternent L, Thiruchelvam N, Timoney A, Vale L, Walton K, von Wilamowitz-Moellendorff A, Wilkinson J, Wood R, Pickard R. Continuous low-dose antibiotic prophylaxis for adults with repeated urinary tract infections (AnTIC): a randomised, open-label trial. The Lancet. Infectious diseases. 2018 Sep:18(9):957-968. doi: 10.1016/S1473-3099(18)30279-2. Epub 2018 Jun 28 [PubMed PMID: 30037647]
Level 1 (high-level) evidenceLuchristt D, Siddiqui NY, Bruton Y, Visco AG. Extended treatment-dose antibiotic therapy versus low-dose prophylaxis for the management of recurrent uncomplicated urinary tract infections in peri- and postmenopausal women. Urology. 2024 Dec 20:():. pii: S0090-4295(24)01218-4. doi: 10.1016/j.urology.2024.12.029. Epub 2024 Dec 20 [PubMed PMID: 39710076]
Scherberich JE, Fünfstück R, Naber KG. Urinary tract infections in patients with renal insufficiency and dialysis - epidemiology, pathogenesis, clinical symptoms, diagnosis and treatment. GMS infectious diseases. 2021:9():Doc07. doi: 10.3205/id000076. Epub 2021 Dec 21 [PubMed PMID: 35106269]
Sabih A, Leslie SW. Complicated Urinary Tract Infections. StatPearls. 2025 Jan:(): [PubMed PMID: 28613784]
Hooton TM, Vecchio M, Iroz A, Tack I, Dornic Q, Seksek I, Lotan Y. Effect of Increased Daily Water Intake in Premenopausal Women With Recurrent Urinary Tract Infections: A Randomized Clinical Trial. JAMA internal medicine. 2018 Nov 1:178(11):1509-1515. doi: 10.1001/jamainternmed.2018.4204. Epub [PubMed PMID: 30285042]
Level 1 (high-level) evidenceAl Demour S, Ababneh MA. Evaluation of Behavioral and Susceptibility Patterns in Premenopausal Women with Recurrent Urinary Tract Infections: A Case Control Study. Urologia internationalis. 2018:100(1):31-36. doi: 10.1159/000485568. Epub 2017 Dec 14 [PubMed PMID: 29241191]
Level 2 (mid-level) evidenceJepson RG, Williams G, Craig JC. Cranberries for preventing urinary tract infections. The Cochrane database of systematic reviews. 2012 Oct 17:10(10):CD001321. doi: 10.1002/14651858.CD001321.pub5. Epub 2012 Oct 17 [PubMed PMID: 23076891]
Level 1 (high-level) evidenceUehling DT, Hopkins WJ, Elkahwaji JE, Schmidt DM, Leverson GE. Phase 2 clinical trial of a vaginal mucosal vaccine for urinary tract infections. The Journal of urology. 2003 Sep:170(3):867-9 [PubMed PMID: 12913718]
Level 1 (high-level) evidenceHopkins WJ, Elkahwaji J, Beierle LM, Leverson GE, Uehling DT. Vaginal mucosal vaccine for recurrent urinary tract infections in women: results of a phase 2 clinical trial. The Journal of urology. 2007 Apr:177(4):1349-53; quiz 1591 [PubMed PMID: 17382730]
Level 1 (high-level) evidenceSánchez-Ramón S, Fernández-Paredes L, Saz-Leal P, Diez-Rivero CM, Ochoa-Grullón J, Morado C, Macarrón P, Martínez C, Villaverde V, de la Peña AR, Conejero L, Hernández-Llano K, Cordero G, Fernández-Arquero M, Gutierrez BF, Candelas G. Sublingual Bacterial Vaccination Reduces Recurrent Infections in Patients With Autoimmune Diseases Under Immunosuppressant Treatment. Frontiers in immunology. 2021:12():675735. doi: 10.3389/fimmu.2021.675735. Epub 2021 Jun 4 [PubMed PMID: 34149711]
Spaulding CN, Klein RD, Schreiber HL 4th, Janetka JW, Hultgren SJ. Precision antimicrobial therapeutics: the path of least resistance? NPJ biofilms and microbiomes. 2018:4():4. doi: 10.1038/s41522-018-0048-3. Epub 2018 Feb 27 [PubMed PMID: 29507749]
Beerepoot MA, Geerlings SE, van Haarst EP, van Charante NM, ter Riet G. Nonantibiotic prophylaxis for recurrent urinary tract infections: a systematic review and meta-analysis of randomized controlled trials. The Journal of urology. 2013 Dec:190(6):1981-9. doi: 10.1016/j.juro.2013.04.142. Epub 2013 Jul 15 [PubMed PMID: 23867306]
Level 1 (high-level) evidenceHannan TJ, Roberts PL, Riehl TE, van der Post S, Binkley JM, Schwartz DJ, Miyoshi H, Mack M, Schwendener RA, Hooton TM, Stappenbeck TS, Hansson GC, Stenson WF, Colonna M, Stapleton AE, Hultgren SJ. Inhibition of Cyclooxygenase-2 Prevents Chronic and Recurrent Cystitis. EBioMedicine. 2014 Nov:1(1):46-57. doi: 10.1016/j.ebiom.2014.10.011. Epub 2014 Oct 24 [PubMed PMID: 26125048]
Gágyor I, Bleidorn J, Kochen MM, Schmiemann G, Wegscheider K, Hummers-Pradier E. Ibuprofen versus fosfomycin for uncomplicated urinary tract infection in women: randomised controlled trial. BMJ (Clinical research ed.). 2015 Dec 23:351():h6544. doi: 10.1136/bmj.h6544. Epub 2015 Dec 23 [PubMed PMID: 26698878]
Level 1 (high-level) evidence