Introduction
Radiation safety is a concern for patients, physicians, and staff in many departments, including radiology, interventional cardiology, and surgery. Radiation emitted during fluoroscopic procedures is responsible for the greatest radiation dose for medical staff. Radiation from diagnostic imaging modalities, such as computed tomography, mammography, and nuclear imaging, are minor contributors to the cumulative dose exposures of healthcare personnel. However, any radiation exposure poses a potential risk to both patients and healthcare workers alike.[1]
Radiation protection aims to reduce unnecessary radiation exposure with a goal to minimize the harmful effects of ionizing radiation.[2] In the medical field, ionizing radiation has become an inescapable tool used for the diagnosis and treatment of a variety of medical conditions. As its use has evolved, so have the cumulative doses of lifetime radiation that both patients and medical providers receive. Most radiation exposure in medical settings arises from fluoroscopic imaging, which uses x-rays to obtain dynamic and cinematic functional imaging. Formal radiation protection training helps reduce radiation exposure to medical staff and patients.[3] However, enforcing radiation safety guidelines can be an arduous process, and many interventionalists do not receive formal training in either residency or fellowship on radiation dose reduction. In particular, clinicians or medical staff that use fluoroscopic imaging outside of dedicated radiology or interventional departments have low adherence to radiation safety guidelines. Fluoroscopy is used in many specialties, including orthopedics, urology, interventional radiology, interventional cardiology, vascular surgery, and gastroenterology. As radiation exposure becomes more prevalent, a thorough understanding of radiation exposure risks and dose reduction techniques will be of utmost importance.
There are three basic principles of radiation protection: justification, optimization, and dose limitation. Justification involves an appreciation for the benefits and risks of using radiation for procedures or treatments. Physicians, surgeons, and radiologic personnel all play a key role in educating patients on the potential adverse effects of radiation exposure. The benefits of exposure should be well known and accepted by the medical community. Often, procedures that expose patients to relatively higher doses of radiation—for example, interventional vascular procedures—are medically necessary, and thus the benefits outweigh the risks. The As Low as Reasonably Achievable (ALARA) principle, defined by the code of federal regulations, was created to ensure that all measures to reduce radiation exposure have been taken while acknowledging that radiation is an integral part of diagnosing and treating patients. Any amount of radiation exposure will increase the risk of stochastic effects, namely the chances of developing malignancy following radiation exposure. These effects are thought to occur as a linear model in which there is no specific threshold to predict whether or not malignancy will develop reliably. For these reasons, the radiologic community teaches protection practices under the ALARA principle.
Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Function
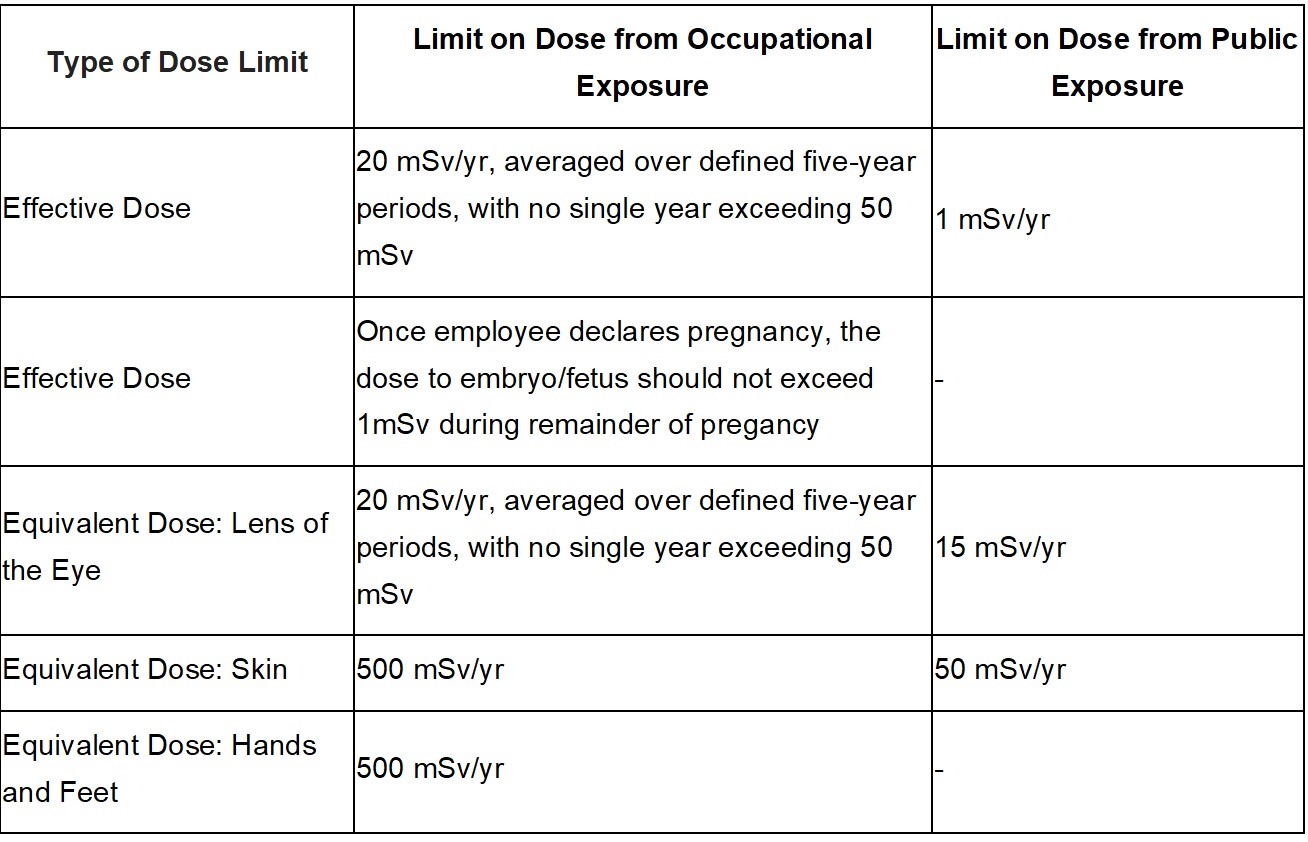
A basic understanding of the science behind the damaging effects of radiation is crucial in evaluating the different strategies to protect medical professionals and patients. X-rays are composed of high-energy photons within the electromagnetic spectrum. X-rays are notable in comparison to lower energy photons since they are powerful enough to break molecular bonds and ionize atoms.[4] This ionization produces free radicals, chemically active compounds that can indirectly damage DNA.[5] Medical staff and patients can be exposed to x-ray radiation either as scattered x-rays or by direct exposure to the x-ray beam. Scattered x-rays give up part of their energy during the scattering process, and thus energy deposited in tissues from scattered x-rays is lower than directly from the x-ray source. Radiation doses can be expressed in three different ways. The absorbed dose is the radiation deposited in an object and is measured in milligrays (mGy). The equivalent dose is calculated, taking into account the organ-specific radiation exposure, as well as the organ's sensitivity to radiation, and is expressed in millisieverts (mSv). The effective dose is the sum over the entire body of the individual organ equivalent doses and is expressed in millisieverts (mSv). An understanding of these definitions is critical to interpreting dose recommendations. The ICRP's dose recommendations are shown in fig 1.[3] For reference, 20 mSv/year roughly equates to 2 to 3 abdominal and pelvic computed tomography (CT) scans or 7 TO 9 years of background radiation. Exposure surpassing this threshold averaged over five years has been associated with a 1 in 1000 lifetime risk of fatal cancer.[6][7][5]
Issues of Concern
Radiation exposure can produce biological effects as either a dose-dependent effect or a dose-dependent probability.[8] Dose-dependent effects are referred to as deterministic effects and occur when a specific exposure threshold has been exceeded. A dose-dependent probability is referred to as a stochastic effect and represents an outcome that occurs with a certain probability but without a defined threshold at which these effects are triggered.[9] Examples of deterministic effects that have been documented in the fields of interventional radiology, cardiology, and radiation treatment include radiation-induced thyroiditis, dermatitis, and hair loss.[10] Stochastic effects are discovered many years after radiation exposure and include the development of cancer.[3] It is important to note that deterministic effects are determined by the cumulative amount of radiation exposure an organ or tissue experiences over time (the lifetime equivalent dose). In comparison, there is a chance that a specific x-ray causes DNA damage that later develops into cancer, a stochastic effect. As the number of x-rays a patient is exposed to increases, the chance of a stochastic effect increases; however, the lifetime equivalent radiation dose does not play a role in stochastic effects. Researching the effects of long-term low-dose exposure to ionizing radiation is difficult because literature is based on epidemiologic data from large radiation exposures at doses that are much higher than is used in the medical setting. Current literature suggests that medical radiation may result in a modest increase in the risk of cataracts, cancer, and possibly hereditary diseases.[6]
Clinical Significance
The duration of radiation exposure, distance from the radiation source, and physical shielding are the key facets in reducing exposure. The exposure duration can be minimized in several ways. When exposing a patient to radiation, the technician or physician should preplan the required images to avoid unnecessary and redundant exposure. Magnification significantly increases the exposure to the patient; therefore, magnification should be used judiciously.[11] Continuous or live fluoroscopy may be helpful to understand anatomy during procedures better, but standard fluoroscopy machines capture roughly 35 images per second. Decreased exposure can be achieved instead by using pulsed fluoroscopy, which obtains about five images per second without sacrificing imaging quality. Lastly, exposure duration should be limited whenever possible.
Increasing the distance between the x-ray beam and the part that is being imaged is another way to minimize exposure. The image intensifier or x-ray plate should be as close to the patient as possible, with the x-ray tube positioned as far away as possible while maintaining adequate image resolution. A similar approach can be used to minimize exposure to medical professionals. Scattered radiation—the type of radiation that surgeons, interventionalists, and operating room staff commonly encounter during procedures requiring fluoroscopy—follows an inverse square law. Scattering exposure levels decrease proportionally with the inverse of the distance squared from the x-ray source. Staff can lower their exposure levels by a factor of four by doubling their distance from the source. Through this simple concept, occupational radiation exposure can be dramatically reduced.
Physical radiation shielding can be accomplished with different forms of personal protective equipment (PPE). Some fluoroscopy suites contain ceiling-suspended lead acrylic shields, which can reduce doses to the head and neck by a factor of 10. Portable rolling shields, which do not require installation, can protect staff in operating rooms and interventional settings. These mobile shields have been shown to decrease the effective radiation dose to staff by more than 90% when used correctly.[12] In cases where it is not feasible to shield oneself behind a physical barrier, all personnel should wear leaded aprons for protection. Leaded aprons, which are required in most states, commonly come in thicknesses of 0.25 mm, 0.35 mm, and 0.5 mm. Aprons that wrap circumferentially around the body are preferred to front aprons, given their increased surface area coverage. In general, transmission through leaded aprons is typically between 0.5% and 5%. Leaded aprons should always be companied by a thyroid shield. Personal protective equipment also protects our patients. Patients should wear protective gowns in areas not being imaged, whether in plain radiographs, fluoroscopy, or CT scans. Leaded eyeglasses and should be at least 0.25 mm lead equivalents to provide adequate protection for the lens of the eye. Leaded glasses are commonly cited as the least worn piece of PPE in multiple studies, with compliance rates ranging from 2.5% to 5%.[13] Studies have shown a relationship between occupational radiation doses and cataract development before 50 in a large cohort of radiation technologists, specifically the posterior lens.[14] Interestingly, the opacification of the posterior lens, in comparison to the other locations, is relatively specific to radiation exposure. Regular use of leaded eyeglasses can reduce radiation exposure to the lens by 90%. The low compliance rate for wearing leaded eyeglasses demonstrates an area for improvement. Beyond the appropriate use of leaded aprons, proper storage and testing of the equipment are critical to ensuring its effectiveness. Lead garments should be checked every six months to assure their integrity, and leaded aprons should be hung rather than folded to prevent cracking.
Dosimeters are devices that measure cumulative radiation exposure. These devices should be worn by all hospital staff who encounter planned ionizing radiation. Unfortunately, in a significant number of healthcare settings, there is a paucity of monitoring and, thus, a lack of reliable data. Sanchez et al. reported that as much as 50% of physicians do not wear or incorrectly wear dosimeters.[15] Dosimeters should be worn both outside and inside the leaded apron for comparison of doses, and the readings should be analyzed by the facility’s radiation safety department. Raising awareness of the importance of dosimetry should be a priority for the occupational safety or radiation safety departments in health systems. Staff who comply with dosimeter regulations can receive feedback about where and when they are receiving radiation doses, which can help audit behaviors and promote increased safety awareness.
Other Issues
Since 1941 when I-131 was used for the treatment of thyrotoxicosis, the use of nuclear medicine for imaging and therapeutic procedures has increased at an exponential rate.[16] Nuclear medicine uses radioactive material to help diagnose and treat conditions such as cancer or cardiac disease. PET scans are an example of diagnostic imaging that involves injecting a small dosage of radiopharmaceutical material to image and measure the function of an organ. Medical administration of radiopharmaceuticals or external beam radiation therapy is used under the prescription of an authorized physician. Internal radiation therapy, or brachytherapy, is a form of nuclear medicine treatment where radiation is released from inside the body for treatment of cancer, such as non-Hodgkin lymphoma.[16] Brachytherapy comes with its side effects, which differ from ionizing radiation from medical imaging. The most common adverse reactions are thrombocytopenia, neutropenia, fatigue, nausea, vomiting, diarrhea.
Radiation exposure from various nuclear power plants has allowed us to develop basic principles of radiation protection to ensure the safety of employees and how to handle unplanned exposures. If an employee encounters a scenario where radioactive material has been spilled, it must be dealt with according to specific regulations. For example, radioactive materials should not be flushed down normal sanitation drains. They should be allowed to decay in an adequately shielded facility when they have half-lives less than 90 days.[17] Radioactive waste tags should be labeled and disposed of to radioactive waste departments. The secure storage of the waste should be maintained at all times.
Enhancing Healthcare Team Outcomes
As medical imaging evolves, so does the medical community’s understanding of how to protect people from ionizing radiation. The first step to optimizing safe radiation practice is educating hospital staff on radiation best practices. Each institution’s radiation safety department is responsible for educating and enforcing protective strategies. Protocol development and education strategies have been effective in multiple specialties. Simple interventions can play a major role in radiation dose optimization. For example, after a 20-minute video was used to educate physicians on radiation best practices, it was found to reduce median fluoroscopy time by 30% to 50%.[18] Justification, optimization, and adherence to dose limits can significantly decrease exposure when followed. Following the ALARA principle, health care workers should confirm that the benefits of the exposure outweigh the risks and strive to decrease radiation exposure as far below the dose limits as practical.
Media
References
Mitchell EL, Furey P. Prevention of radiation injury from medical imaging. Journal of vascular surgery. 2011 Jan:53(1 Suppl):22S-27S. doi: 10.1016/j.jvs.2010.05.139. Epub 2010 Sep 16 [PubMed PMID: 20843625]
Tsapaki V, Balter S, Cousins C, Holmberg O, Miller DL, Miranda P, Rehani M, Vano E. The International Atomic Energy Agency action plan on radiation protection of patients and staff in interventional procedures: Achieving change in practice. Physica medica : PM : an international journal devoted to the applications of physics to medicine and biology : official journal of the Italian Association of Biomedical Physics (AIFB). 2018 Aug:52():56-64. doi: 10.1016/j.ejmp.2018.06.634. Epub 2018 Jun 21 [PubMed PMID: 30139610]
. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Annals of the ICRP. 2007:37(2-4):1-332 [PubMed PMID: 18082557]
Frane N, Megas A, Stapleton E, Ganz M, Bitterman AD. Radiation Exposure in Orthopaedics. JBJS reviews. 2020 Jan:8(1):e0060. doi: 10.2106/JBJS.RVW.19.00060. Epub [PubMed PMID: 31899700]
Hayda RA, Hsu RY, DePasse JM, Gil JA. Radiation Exposure and Health Risks for Orthopaedic Surgeons. The Journal of the American Academy of Orthopaedic Surgeons. 2018 Apr 15:26(8):268-277. doi: 10.5435/JAAOS-D-16-00342. Epub [PubMed PMID: 29570497]
Matityahu A, Duffy RK, Goldhahn S, Joeris A, Richter PH, Gebhard F. The Great Unknown-A systematic literature review about risk associated with intraoperative imaging during orthopaedic surgeries. Injury. 2017 Aug:48(8):1727-1734. doi: 10.1016/j.injury.2017.04.041. Epub 2017 Apr 21 [PubMed PMID: 28648410]
Level 1 (high-level) evidenceZielinski JM, Shilnikova NS, Krewski D. Canadian National Dose Registry of radiation workers: overview of research from 1951 through 2007. International journal of occupational medicine and environmental health. 2008:21(4):269-75. doi: 10.2478/v10001-008-0037-5. Epub [PubMed PMID: 19228574]
Level 3 (low-level) evidenceHamada N, Fujimichi Y. Classification of radiation effects for dose limitation purposes: history, current situation and future prospects. Journal of radiation research. 2014 Jul:55(4):629-40. doi: 10.1093/jrr/rru019. Epub 2014 May 3 [PubMed PMID: 24794798]
López M, Martín M. Medical management of the acute radiation syndrome. Reports of practical oncology and radiotherapy : journal of Greatpoland Cancer Center in Poznan and Polish Society of Radiation Oncology. 2011 Jul 13:16(4):138-46. doi: 10.1016/j.rpor.2011.05.001. Epub 2011 Jul 13 [PubMed PMID: 24376971]
Rehani MM, Ciraj-Bjelac O, Vañó E, Miller DL, Walsh S, Giordano BD, Persliden J. ICRP Publication 117. Radiological protection in fluoroscopically guided procedures performed outside the imaging department. Annals of the ICRP. 2010 Dec:40(6):1-102. doi: 10.1016/j.icrp.2012.03.001. Epub [PubMed PMID: 22732420]
Srinivasan D, Than KD, Wang AC, La Marca F, Wang PI, Schermerhorn TC, Park P. Radiation safety and spine surgery: systematic review of exposure limits and methods to minimize radiation exposure. World neurosurgery. 2014 Dec:82(6):1337-43. doi: 10.1016/j.wneu.2014.07.041. Epub 2014 Aug 1 [PubMed PMID: 25088230]
Level 1 (high-level) evidenceLópez PO, Dauer LT, Loose R, Martin CJ, Miller DL, Vañó E, Doruff M, Padovani R, Massera G, Yoder C, Authors on Behalf of ICRP. ICRP Publication 139: Occupational Radiological Protection in Interventional Procedures. Annals of the ICRP. 2018 Mar:47(2):1-118. doi: 10.1177/0146645317750356. Epub [PubMed PMID: 29532669]
Kaplan DJ, Patel JN, Liporace FA, Yoon RS. Intraoperative radiation safety in orthopaedics: a review of the ALARA (As low as reasonably achievable) principle. Patient safety in surgery. 2016:10():27. doi: 10.1186/s13037-016-0115-8. Epub 2016 Dec 12 [PubMed PMID: 27999617]
Chodick G, Bekiroglu N, Hauptmann M, Alexander BH, Freedman DM, Doody MM, Cheung LC, Simon SL, Weinstock RM, Bouville A, Sigurdson AJ. Risk of cataract after exposure to low doses of ionizing radiation: a 20-year prospective cohort study among US radiologic technologists. American journal of epidemiology. 2008 Sep 15:168(6):620-31. doi: 10.1093/aje/kwn171. Epub 2008 Jul 29 [PubMed PMID: 18664497]
Level 2 (mid-level) evidenceSánchez RM, Vano E, Fernández JM, Rosales F, Sotil J, Carrera F, García MA, Soler MM, Hernández-Armas J, Martínez LC, Verdú JF. Staff doses in interventional radiology: a national survey. Journal of vascular and interventional radiology : JVIR. 2012 Nov:23(11):1496-501. doi: 10.1016/j.jvir.2012.05.056. Epub 2012 Jul 24 [PubMed PMID: 22832138]
Level 3 (low-level) evidenceLin Y. Internal radiation therapy: a neglected aspect of nuclear medicine in the molecular era. Journal of biomedical research. 2015 Sep:29(5):345-55. doi: 10.7555/JBR.29.20140069. Epub 2015 Jan 12 [PubMed PMID: 26445567]
Leonard RB, Ricks RC. Emergency department radiation accident protocol. Annals of emergency medicine. 1980 Sep:9(9):462-70 [PubMed PMID: 7425419]
Barakat MT, Thosani NC, Huang RJ, Choudhary A, Kochar R, Kothari S, Banerjee S. Effects of a Brief Educational Program on Optimization of Fluoroscopy to Minimize Radiation Exposure During Endoscopic Retrograde Cholangiopancreatography. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2018 Apr:16(4):550-557. doi: 10.1016/j.cgh.2017.08.008. Epub 2017 Aug 10 [PubMed PMID: 28804031]