Introduction
Pudendal nerve blocks are a preferred technique for diagnosing and managing chronic pelvic pain, particularly in cases of pudendal neuralgia often linked to nerve entrapment. This regional anesthetic technique is also widely employed in gynecologic, obstetric, and anorectal procedures. Pudendal nerve blocks are commonly used to reduce labor pain, provide localized anesthesia during surgery, and treat chronic pelvic pain conditions across various clinical settings.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
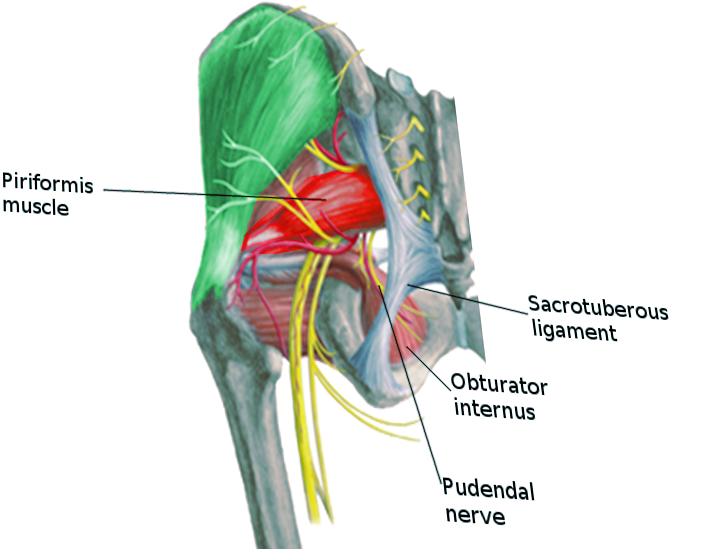
The pudendal nerve is a sensory and motor nerve arising from the sacral plexus and forms from the ventral S2-S4 spinal nerve roots.[1] The pudendal nerve passes through the greater sciatic foramen, traversing the sacrospinous and sacrotuberous ligaments (see Image. Pudendal Nerve).[1] The pudendal nerve then reenters the perineum through the lesser sciatic foramen along with the internal pudendal artery and vein.[1] The pudendal nerve courses through the ischiorectal fossa and Alcock canal, also known as the pudendal canal.[1][2] Inside the Alcock canal, the nerve initially divides into the inferior rectal nerve and then gives off the perineal nerve.[1]
Ultimately, the nerve continues as the dorsal nerve, which innervates the penis and clitoris.[1] The inferior rectal nerve innervates the external anal sphincter and the perianal skin. The perineal nerve innervates the bulbospongiosus, ischiocavernosus, and levator ani muscles and sends sensory branches to the skin of the labia majora and scrotum. The dorsal nerve branch is a sensory nerve that supplies the skin of the clitoris and penis.[1] Trauma and disorders that affect the pudendal nerve disproportionately affect the sensory portion of the nerve.[3] The areas affected by the sensory distribution of the pudendal nerve include the perineum, the lower buttocks, the anus, and the genitalia (vulva, labia, and clitoris in women; the scrotum and penis in men).[3]
The 4 common locations of pudendal nerve entrapment include:
- Type 1: Inferior to the piriformis muscle, where the pudendal nerve leaves the greater sciatic notch
- Type 2: Between the sacrotuberous and sacrospinous ligaments (the most common site of entrapment)
- Type 3: Inside Alcock canal
- Type 4: Terminal branches only (superficial and deep perineal nerves, inferior rectal nerves, and the penile or clitoral dorsal nerve)[4]
The most common causes of pudendal neuralgia are repetitive activities and overuse of the pelvic floor muscles, typically microtrauma from prolonged sitting. Pudendal neuralgia can also be caused by repetitive sports activities, primarily cycling, motor vehicle accidents, falls, pelvic surgeries (especially pelvic prolapse procedures that utilize mesh), radiation therapy, ischial spinal fractures, benign and malignant tumors, and obstetrical injuries.[4][5][6] The most frequent traumatic causes of pudendal neuralgia are obstetrical and post-pelvic prolapse surgery.[4][7] Diabetes, herpes zoster, human immunodeficiency virus, endometriosis, and multiple sclerosis can also cause pudendal neuralgia.[4][8]
Indications
A pudendal nerve block is historically a common regional anesthesia technique to provide perineal anesthesia during obstetric procedures, including vaginal birth during the second stage of labor, vaginal repairs, and anorectal surgeries such as hemorrhoidectomies.[9] Pudendal nerve blocks are infrequently utilized to provide anesthesia for urological procedures. However, the literature describes this technique as a safe and effective local analgesia for patients undergoing a transrectal ultrasound-guided prostate biopsy, transurethral prostatectomy, inflatable penile prosthesis implantation, and for patients with catheter-related bladder discomfort.[2][10][11][12] Pudendal nerve blocks have been shown to decrease pain and the need for postoperative opioid analgesics in patients undergoing inflatable penile prosthesis implants and should be considered as an adjunctive treatment, especially in patients where opioid use needs to be minimized.[10][13][14] The nerve blocks have also been used anecdotally for persistent genital arousal disorder with some success.[15]
Pudendal nerve blocks are also used to treat the pain associated with pudendal neuralgia and aid in its diagnosis. Patients describe the pudendal neuralgia pain as a burning sensation and hyperalgesia in the external genital and perineal region. The pain may also be described as a tingling, aching, stabbing, or an electric shock type of discomfort.[4][16] The pain is worsened by sitting and relieved while standing, is often worse after ejaculation, and urinary symptoms (urgency and frequency) and erectile dysfunction may occur.[4][16][17]
Most pudendal neuralgia is unilateral; however, there are reports of bilateral neuralgia in cyclists.[18] The diagnosis of pudendal neuralgia is often delayed due to its nonspecific nature. Misdiagnosis is common, as is delayed treatment. This scenario so frequently occurs that it is recommended that all patients with chronic pelvic pain not responding to treatment should be reevaluated for possible pudendal nerve entrapment.[19] A successful pudendal nerve block is a key test to help confirm a diagnosis of pudendal nerve entrapment and neuralgia.[4][16] If the test block is successful, it may be repeated monthly for longer-term pain control. Results from a randomized controlled study demonstrated that adding intravenous dexamethasone had a potentiating effect on pudendal nerve blocks for pain relief in children receiving hypospadias surgery.[20][21]
Contraindications
Pudendal blocks are considered very low risk with few contraindications. These contraindications include:
- Known allergic reactions to the specific local anesthetic used
- Active infection or sepsis
- Skin and soft tissue infections at the injection site
- Uncorrected coagulopathies and prior surgery in the area with altered local anatomy
Equipment
The equipment required for a pudendal nerve block consists of chlorhexidine or a povidone-iodine solution, disposable sterile drapes, sterile gloves, sterile gauze swabs, sterile syringes, and needles, and a local anesthetic solution of choice. A 20 cm 20-gauge spinal needle is often used. Lidocaine 1% and bupivacaine 0.25% are the most commonly used solutions. For longer-term therapy, a combination of lidocaine, bupivacaine, and a steroid such as triamcinolone is sometimes used, as this can provide 30 days or more of relief.[4] The block can be performed without image guidance, but ultrasound or fluoroscopy are recommended. Equipment for monitoring a patient’s hemodynamic status should also be available.
Personnel
Staff typically consists of a nurse and a physician trained in performing pudendal nerve blocks. Depending on the imaging modality used, a technician should also be present.
Preparation
The first step is to explain the procedure in detail, including the expected benefits, possible risks, and realistic alternatives. Next, the patient’s consent is obtained to perform the procedure. The equipment and medications required for the nerve block must be ready and present in the room prior to starting the procedure. After conducting the time-out, the patient is placed in the desired position. The targeted area is appropriately cleaned and covered by sterile drapes. Depending on the imaging modality of choice, the room should be equipped with that device.
Technique or Treatment
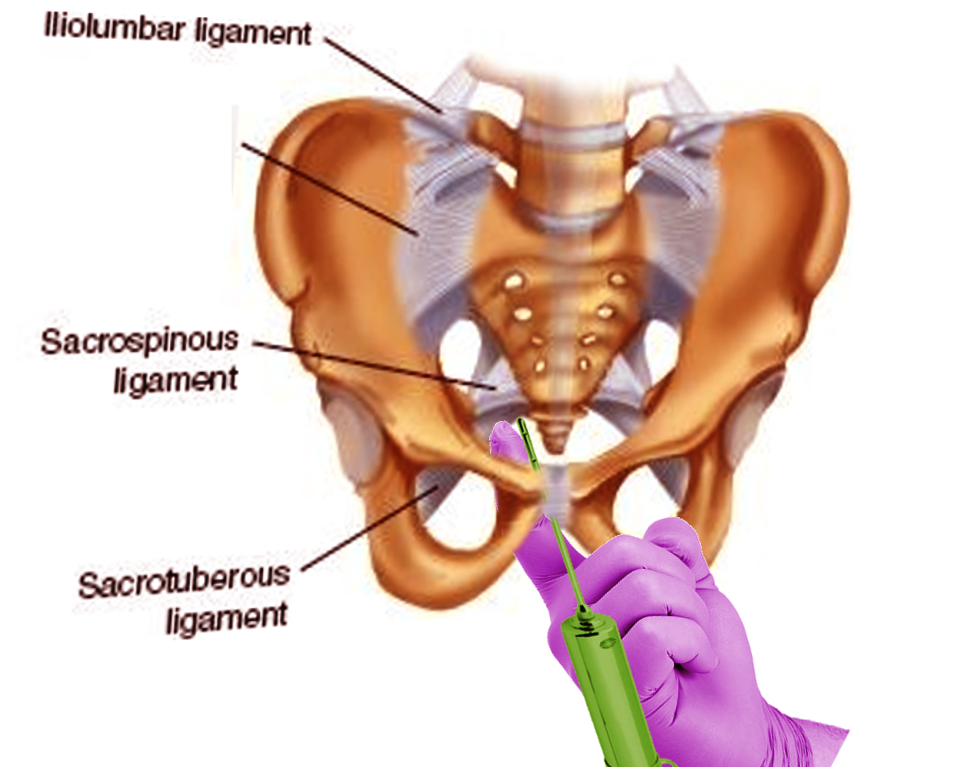
A pudendal nerve block aims to block the nerve as it enters the lesser sciatic foramen, 1 cm inferior and medial relative to the attachment of the sacrospinous ligament to the ischial spine (see Image. Pudendal Nerve Block). Different anatomical approaches are used to achieve successful pudendal nerve blocks, which may be administered unilaterally or bilaterally. The syringe is not attached until the needle has reached its final position immediately before the injection of the anesthetic agent.
The transvaginal approach to a pudendal nerve block is common for obstetric and gynecological procedures (see Image. Female Perineum). Typically, 10 mL of anesthetic is used per side, but this is variable.
- The patient is placed in the lithotomy position, and the vaginal area is prepped.
- The ischial spines can be identified by palpation along the posterolateral vaginal sidewalls. If, for any reason, the ischial spines cannot be palpated directly, the firm band of the sacrospinous ligament should be identified. This can be followed laterally from the sacrum to the respective ischial spine.
- A needle guide is gently introduced so it lies on the vaginal mucosa along the sacrospinous ligament, approximately 1 cm medial and inferior to the ischial spine. A needle guide such as the Iowa trumpet is recommended to limit penetration depth and minimize tissue injury.
- The sacrospinous ligament is punctured.
- Injecting 3 mL of a local anesthetic directly into the sacrospinous ligament near its ischial insertion before advancing the spinal needle to its final position is optional but suggested to minimize patient discomfort.
- The needle is passed 1 cm caudal from the ischial spine until a loss of resistance is noticed or its position is confirmed by imaging.[22]
- Upon negative aspiration, the local anesthetic is injected just posteriorly to the ischial spine at the attachment of the sacrospinous ligament.
- Alternatively, the injection can be performed just medial to the ischial spine.[23] The nerve is located just behind the ligament in the loose areolar tissue. This area can be identified by imaging and by the loss of resistance to the advancement of the needle as the ligamentous tissue is completely penetrated.
- Aspiration to confirm positioning outside a vascular space is again performed as the inferior gluteal and pudendal vessels are immediately adjacent to the pudendal nerve.
- A pinprick or similar sensory test in the anogenital area ensures adequate regional anesthesia.
- The procedure is repeated on the opposite side to achieve a bilateral block.
The transperineal approach is used for anorectal and urological procedures as well as for pudendal neuralgia in men (see Image. Perineal Arteries and Nerves, Male Perineum). Imaging guidance, such as ultrasound, is recommended for this approach.
- The patient is placed in the lithotomy position.
- The skin is prepped.
- The clinician's index finger will be inserted into the rectum (or vagina) to palpate the ischial spine.
- The skin entry point is selected 1 inch (2.5 cm) posteromedial to the ischial tuberosity as determined by palpation or imaging.
- After identifying the ischial spine, the needle will puncture the skin transperineally, medial to the ischial tuberosity.
- The needle is advanced lateral to the clinician's finger in the posterolateral direction until it reaches the ischial spine.
- Injecting 3 mL of a local anesthetic directly into the sacrospinous ligament near its ischial insertion before advancing the spinal needle to its final position is optional.
- The needle is then advanced through the sacrospinous ligament 1 cm medial and inferior to the ischial spine.
- The final position of the needle can be identified by imaging or by the loss of resistance to the advancement of the needle as the ligamentous tissue is completely penetrated.
- After negative aspiration, the local anesthetic of choice is injected.
- A pinprick or similar sensory test in the anogenital area is performed to ensure adequate anesthesia in the region.
- The procedure is repeated on the opposite side to achieve a bilateral block.
A perirectal approach to a pudendal nerve block has also been described using a nerve stimulator to elicit contractions of the external anal sphincter.[24]
- The patient is positioned in a recumbent position.
- The skin is prepped.
- The clinician's index finger will be inserted into the rectum (or vagina) to palpate the ischial spine.
- The needle is advanced lateral to the rectum, and the clinician's finger is in the posterolateral direction until it reaches the ischial spine.[24]
- Injecting 3 mL of a local anesthetic directly into the sacrospinous ligament near its ischial insertion before advancing the spinal needle to its final position is optional.
- The needle is then advanced through the sacrospinous ligament 1 cm medial and inferior to the ischial spine.
- The final position of the needle can be identified by imaging, by maximal anal sphincteric tone on nerve stimulation of the needle, or by the loss of resistance to advancement of the needle as the ligamentous tissue is completely penetrated.
- After negative aspiration, the local anesthetic of choice is injected.
- A pinprick or similar sensory test in the anogenital area is performed to ensure adequate anesthesia in the region.
- The procedure is repeated on the opposite side to achieve a bilateral block.
A transgluteal approach has also been described, with or without fluoroscopic guidance, and is similar to the techniques reviewed above.[25][26][27] A pudendal block test injection directly into the Alcock canal is sometimes performed using contrast under image guidance to help indicate if surgical decompression surgery is likely to be successful.[16][25] The effect of a pudendal nerve block is usually immediate, within 5 minutes, but it may take up to 20 minutes to be fully effective.[28]
Pudendal nerve blocks can take place with or without ultrasound guidance in women. However, in men, pudendal nerve blocks are typically performed using ultrasound guidance due to challenges in identifying the anatomical landmarks.[29] Pudendal nerve blocks under magnetic resonance imaging, fluoroscopy, or computed tomography have also been described but are less commonly used methods. Ultrasound avoids ionizing radiation exposure to the patient and is ideal for patients needing repeated nerve blocks.
The most common cause of pudendal block failure is not giving the anesthetic sufficient time to take effect. If a bilateral block is only effective on 1 side, an additional 5 mL of anesthetic can be administered to the unaffected side. Up to 50% of all pudendal nerve blocks may fail on at least 1 side, although the median failure rate averages about 20%.[30][31] This is often due to poor technique or a lack of physician training or experience.[31][32][33]
Pudendal nerve blocks can effectively anesthetize the posterior perineum, the anus, the lower vagina, the vulva/scrotum, and the penis.[3] However, successful pudendal nerve blocks will not affect sensation in the anterior perineum, which is supplied by branches of the genitofemoral and ilioinguinal nerves. These blocks will also not affect the cervix or upper vaginal vault and are ineffective in controlling pain from uterine manipulations.[34] The upper vaginal, cervical, and lower uterine sensation is through the ureterovaginal plexus, which can be anesthetized through a paracervical nerve block.[35][36] Local anesthetic is given submucosally, just posterolateral to the uterocervical junction.[37] This effectively blocks sensory and pain nerve transmission at the paracervical ganglia.[38] As it may cause fetal bradycardia, paracervical blocks are not generally performed in the United States; epidural and other pain control methods are widely available.[39][40]
Long-term intermittent (typically monthly or as-needed) pudendal nerve blocks can successfully relieve pudendal neuralgia. Still, there is evidence that they may lose efficacy after 2 years.[41] At that point, alternative therapies, such as decompressive surgery, can be utilized. Endovascular blockage of the pudendal nerve using a hexapolar electrode catheter introduced into the immediately adjacent internal pudendal artery has been performed experimentally.[42] Endovascular pudendal nerve blocks may provide an alternative solution to treating bladder-sphincter dyssynergia in managing patients with a spinal cord injury.[42]
Complications
The most common adverse event of a pudendal nerve block is discomfort at the injection site. The risk of bleeding and infection is less common. The more serious adverse events occur rarely and include pudendal nerve damage or structural injury of the organs in the proximity of the pudendal nerve, such as the bladder and rectum. Pudendal artery puncture with the intravascular injection of local anesthetics can cause systemic local anesthetic toxicity, which is potentially fatal.
Clinical Significance
A pudendal nerve block can serve as a diagnostic method to reveal underlying pudendal neuralgia and is performed primarily with local anesthetics for testing. Patients who report significant pain relief are candidates for pudendal nerve block performed with corticosteroids and local anesthetic combinations for possible long-term pain relief. The effect of the block is variable and reported to last from weeks to months. Pudendal nerve block testing should be considered in all patients with pelvic pain who do not respond to initial therapy.[19]
Pudendal nerve blocks have been shown to achieve a high level of pain control compared to general or neuraxial anesthetic methods, and patients require fewer systemic analgesics.[43] In line with other regional anesthesia techniques, pudendal nerve blocks can minimize the risk of complications associated with general anesthesia, such as cardiopulmonary depression, and adverse events associated with neuraxial anesthesia, such as urinary retention. However, due to patient discomfort associated with the local injections, the perceived risk of injuring critical structures, and a lack of sufficient training in urology and gynecology residency programs, pudendal nerve blocks are underutilized, especially in men.[29]
Enhancing Healthcare Team Outcomes
The interprofessional healthcare team should educate the patient before the procedure to ensure that they are fully informed about the risks, benefits, and alternatives to a pudendal nerve block. A pudendal nerve block is a safe and cost-effective method of obtaining regional anesthesia in the targeted area; however, patients require counseling that the response to the block is somewhat unpredictable, and they might not experience complete pain relief. Setting realistic expectations is essential.
Physicians and advanced clinicians must have advanced knowledge of pelvic anatomy, proficiency in performing pudendal nerve blocks, and the ability to utilize ultrasound guidance effectively; they should be skilled in patient assessment, selecting appropriate candidates, and managing potential complications. The nursing staff will play a vital role throughout the process, from preparing the patient for the procedure to monitoring them during the block while assisting the clinician and providing post-injection care, patient education, and support. Pharmacists need expertise in the pharmacodynamics and pharmacokinetics of local anesthetics, managing drug interactions, and advising on appropriate dosing, especially in complex cases. Regular team debriefings and reviews of pudendal nerve block procedures can help identify areas for improvement, enhance team performance, and ensure the adoption of best practices. With an interprofessional team approach, pudendal nerve blocks can achieve more successful patient outcomes.
Nursing, Allied Health, and Interprofessional Team Interventions
Interprofessional team interventions include the following:
- Obtain consent
- Make sure the necessary supplies are available, including the medications used for the injection
- Educate the patient about the procedure and answer their questions
- Explain to the patient what to expect during the procedure
- Act as a chaperone
- Assist the clinician in performing the nerve block
- Have all monitoring and imaging equipment in the room
- Drape and prep the patient
- Supply post-procedure informational guides or pamphlets
- Explain and arrange post-procedural follow-up
Nursing, Allied Health, and Interprofessional Team Monitoring
Interprofessional team monitoring includes the following:
- Monitor the patient during the procedure
- Comfort the patient
Media
(Click Image to Enlarge)
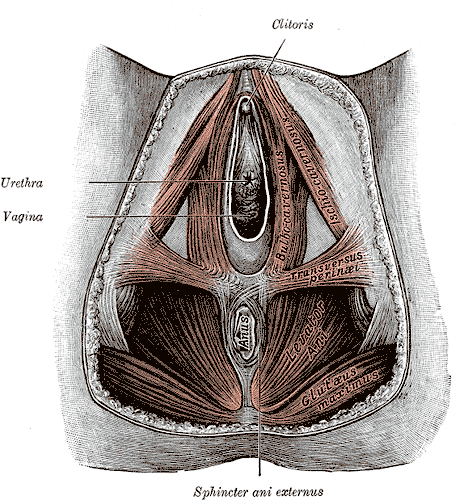
Anatomy of the Female Perineum. The female perineum comprises key anatomical structures, including the clitoris, urethra, vagina, sphincter ani externus, anus, gluteus maximus, levator ani, and transversus perinei.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
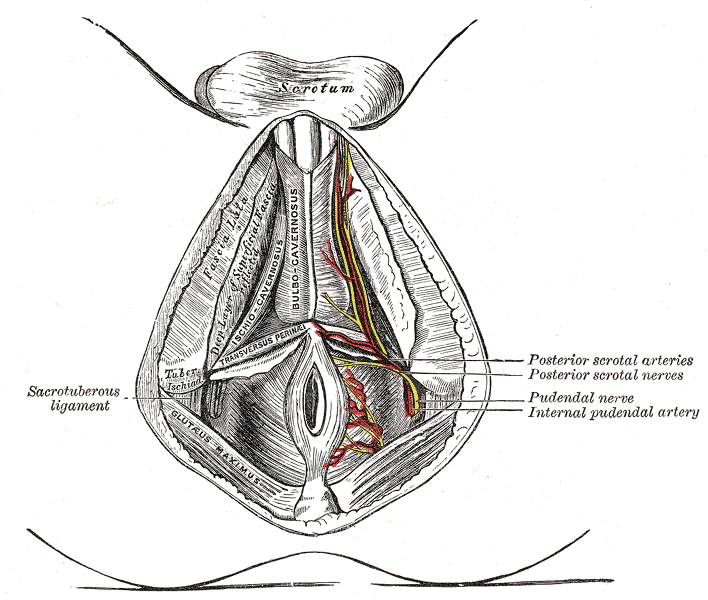
Perineal Arteries and Nerves, Male Perineum. Perineal arteries and nerves in the male perineum include the posterior scrotal arteries, the posterior scrotal nerve, the pudendal nerve, and the internal pudendal artery.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Kinter KJ, Newton BW. Anatomy, Abdomen and Pelvis, Pudendal Nerve. StatPearls. 2024 Jan:(): [PubMed PMID: 32134612]
Oelhafen K, Shayota BJ, Muhleman M, Klaassen Z, Tubbs RS, Loukas M. Benjamin Alcock (1801-?) and his canal. Clinical anatomy (New York, N.Y.). 2013 Sep:26(6):662-6. doi: 10.1002/ca.22080. Epub 2012 Apr 9 [PubMed PMID: 22488487]
Leslie SW, Antolak S, Feloney MP, Soon-Sutton TL. Pudendal Neuralgia. StatPearls. 2024 Jan:(): [PubMed PMID: 32965917]
Kaur J, Leslie SW, Singh P. Pudendal Nerve Entrapment Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 31334992]
Benson JT, Griffis K. Pudendal neuralgia, a severe pain syndrome. American journal of obstetrics and gynecology. 2005 May:192(5):1663-8 [PubMed PMID: 15902174]
Level 2 (mid-level) evidenceNehme-Schuster H, Youssef C, Roy C, Brettes JP, Martin T, Pasquali JL, Korganow AS. Alcock's canal syndrome revealing endometriosis. Lancet (London, England). 2005 Oct 1:366(9492):1238 [PubMed PMID: 16198773]
Level 3 (low-level) evidenceSnooks SJ, Swash M, Henry MM, Setchell M. Risk factors in childbirth causing damage to the pelvic floor innervation. The British journal of surgery. 1985 Sep:72 Suppl():S15-7 [PubMed PMID: 4041752]
Howard EJ. Postherpetic pudendal neuralgia. JAMA. 1985 Apr 19:253(15):2196 [PubMed PMID: 3974113]
Level 3 (low-level) evidenceMongelli F, Lucchelli M, La Regina D, Christoforidis D, Saporito A, Vannelli A, Di Giuseppe M. Ultrasound-Guided Pudendal Nerve Block in Patients Undergoing Open Hemorrhoidectomy: A Post-Hoc Cost-Effectiveness Analysis from a Double-Blind Randomized Controlled Trial. ClinicoEconomics and outcomes research : CEOR. 2021:13():299-306. doi: 10.2147/CEOR.S306138. Epub 2021 Apr 28 [PubMed PMID: 33953578]
Level 1 (high-level) evidenceAbdi S, Shenouda P, Patel N, Saini B, Bharat Y, Calvillo O. A novel technique for pudendal nerve block. Pain physician. 2004 Jul:7(3):319-22 [PubMed PMID: 16858468]
Olgun Keleş B, Tekir Yılmaz E, Altınbaş A. Comparison between the Efficacy of Sacral Erector Spina Plane Block and Pudendal Block on Catheter-Related Bladder Discomfort: A Prospective Randomized Study. Journal of clinical medicine. 2024 Jun 20:13(12):. doi: 10.3390/jcm13123617. Epub 2024 Jun 20 [PubMed PMID: 38930146]
Level 1 (high-level) evidenceLiu T, Wang S, Song J, Zhu H, Zhang J, Zhang P. Application of Periprostatic Nerve Block and Pudendal Nerve Block in Transrectal Ultrasound-Guided Prostate Biopsy. Alternative therapies in health and medicine. 2024 Mar:30(3):140-145 [PubMed PMID: 37883755]
Zhu M, Labagnara K, Loloi J, Babar M, Harandi AA, Salami A, Bernstein A, Davila J, Davuluri M, Chalouhy C, Maria P. Pudendal nerve block decreases narcotic requirements and time spent in post-anesthesia care units in patients undergoing primary inflatable penile prosthesis implantation. International journal of impotence research. 2024 May 17:():. doi: 10.1038/s41443-024-00870-1. Epub 2024 May 17 [PubMed PMID: 38760570]
Sayyid RK, Taylor NS, Owens-Walton J, Oberle MD, Fratino KL, Terris MK, Klaassen Z, King SA. Pudendal nerve block prior to inflatable penile prosthesis implantation: decreased intra-operative narcotic requirements. International journal of impotence research. 2023 Jun:35(4):1-5. doi: 10.1038/s41443-021-00495-8. Epub 2021 Nov 24 [PubMed PMID: 34819658]
Gyorfi MJ, Abd-Elsayed A. Pudendal nerve blockade for persistent genital arousal disorder (PGAD): A clinical review and case report. Pain practice : the official journal of World Institute of Pain. 2024 Jul:24(6):852-855. doi: 10.1111/papr.13362. Epub 2024 Mar 10 [PubMed PMID: 38462787]
Level 3 (low-level) evidenceLevesque A, Bautrant E, Quistrebert V, Valancogne G, Riant T, Beer Gabel M, Leroi AM, Jottard K, Bruyninx L, Amarenco G, Quintas L, Picard P, Vancaillie T, Leveque C, Mohy F, Rioult B, Ploteau S, Labat JJ, Guinet-Lacoste A, Quinio B, Cosson M, Haddad R, Deffieux X, Perrouin-Verbe MA, Garreau C, Robert R. Recommendations on the management of pudendal nerve entrapment syndrome: A formalised expert consensus. European journal of pain (London, England). 2022 Jan:26(1):7-17. doi: 10.1002/ejp.1861. Epub 2021 Oct 13 [PubMed PMID: 34643963]
Level 3 (low-level) evidencePopeney C, Ansell V, Renney K. Pudendal entrapment as an etiology of chronic perineal pain: Diagnosis and treatment. Neurourology and urodynamics. 2007:26(6):820-7 [PubMed PMID: 17480033]
Silbert PL, Dunne JW, Edis RH, Stewart-Wynne EG. Bicycling induced pudendal nerve pressure neuropathy. Clinical and experimental neurology. 1991:28():191-6 [PubMed PMID: 1821826]
Level 3 (low-level) evidenceLuesma MJ, Galé I, Fernando J. Diagnostic and therapeutic algorithm for pudendal nerve entrapment syndrome. Medicina clinica. 2021 Jul 23:157(2):71-78. doi: 10.1016/j.medcli.2021.02.012. Epub 2021 Apr 6 [PubMed PMID: 33836860]
Khalifa SB, Slimene AB, Blaiti H, Kaddour R, Hassen AF, Pardessus P, Brasher C, Dahmani S. The potentiating effect of intravenous dexamethasone upon preemptive pudendal block analgesia for hypospadias surgery in children managed with Snodgrass technique: a randomized controlled study : Dexamethasone for pain management in children. BMC anesthesiology. 2024 Apr 16:24(1):145. doi: 10.1186/s12871-024-02536-3. Epub 2024 Apr 16 [PubMed PMID: 38627668]
Level 1 (high-level) evidenceHayaran N, Kaushik P, Yadav S, Hage A. A Prospective Observational Study Analyzing the Analgesic Efficacy of Caudal Block and Nerve Stimulator-Guided Pudendal Nerve Block in Children Undergoing Hypospadias Repair. Cureus. 2023 Sep:15(9):e44649. doi: 10.7759/cureus.44649. Epub 2023 Sep 4 [PubMed PMID: 37671076]
Level 2 (mid-level) evidenceVancaillie T, Eggermont J, Armstrong G, Jarvis S, Liu J, Beg N. Response to pudendal nerve block in women with pudendal neuralgia. Pain medicine (Malden, Mass.). 2012 Apr:13(4):596-603. doi: 10.1111/j.1526-4637.2012.01343.x. Epub 2012 Mar 5 [PubMed PMID: 22390343]
Level 2 (mid-level) evidenceChoi SS, Lee PB, Kim YC, Kim HJ, Lee SC. C-arm-guided pudendal nerve block: a new technique. International journal of clinical practice. 2006 May:60(5):553-6 [PubMed PMID: 16700853]
Kim SH, Song SG, Paek OJ, Lee HJ, Park DH, Lee JK. Nerve-stimulator-guided pudendal nerve block by pararectal approach. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland. 2012 May:14(5):611-5. doi: 10.1111/j.1463-1318.2011.02720.x. Epub [PubMed PMID: 21752174]
Ricci P, Wash A. Pudendal nerve block by transgluteal way guided by computed tomography in a woman with refractory pudendal neuralgia expressed like chronic perineal and pelvic pain. Archivos espanoles de urologia. 2014 Jul:67(6):565-71 [PubMed PMID: 25048589]
Level 3 (low-level) evidencePloteau S, Perrouin-Verbe MA, Labat JJ, Riant T, Levesque A, Robert R. Anatomical Variants of the Pudendal Nerve Observed during a Transgluteal Surgical Approach in a Population of Patients with Pudendal Neuralgia. Pain physician. 2017 Jan-Feb:20(1):E137-E143 [PubMed PMID: 28072805]
Levin D, Van Florcke D, Schmitt M, Kendall LK, Patel A, Doan LV, Kirpekar M. Fluoroscopy-Guided Transgluteal Pudendal Nerve Block for Pudendal Neuralgia: A Retrospective Case Series. Journal of clinical medicine. 2024 Apr 30:13(9):. doi: 10.3390/jcm13092636. Epub 2024 Apr 30 [PubMed PMID: 38731163]
Level 2 (mid-level) evidenceZador G, Lindmark G, Nilsson BA. Pudendal block in normal vaginal deliveries. Clinical efficacy, lidocaine concentrations in maternal and foetal blood, foetal and maternal acid-base values and influence on uterine activity. Acta obstetricia et gynecologica Scandinavica. Supplement. 1974:(34):51-64 [PubMed PMID: 4531162]
Kalava A, Pribish AM, Wiegand LR. Pudendal nerve blocks in men undergoing urethroplasty: a case series. Romanian journal of anaesthesia and intensive care. 2017 Oct:24(2):159-162. doi: 10.21454/rjaic.7518.242.klv. Epub [PubMed PMID: 29090268]
Level 2 (mid-level) evidenceScudamore JH, Yates MJ. Pudendal block--a misnomer? Lancet (London, England). 1966 Jan 1:1(7427):23-4 [PubMed PMID: 4159157]
Schierup L, Schmidt JF, Torp Jensen A, Rye BA. Pudendal block in vaginal deliveries. Mepivacaine with and without epinephrine. Acta obstetricia et gynecologica Scandinavica. 1988:67(3):195-7 [PubMed PMID: 3051873]
Level 1 (high-level) evidenceAntolak S Jr, Antolak C, Lendway L. Measuring the Quality of Pudendal Nerve Perineural Injections. Pain physician. 2016 May:19(4):299-306 [PubMed PMID: 27228517]
Level 2 (mid-level) evidenceFord JM, Owen DJ, Coughlin LB, Byrd LM. A critique of current practice of transvaginal pudendal nerve blocks: a prospective audit of understanding and clinical practice. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology. 2013 Jul:33(5):463-5. doi: 10.3109/01443615.2013.771155. Epub [PubMed PMID: 23815197]
Level 3 (low-level) evidenceAnderson D. Pudendal nerve block for vaginal birth. Journal of midwifery & women's health. 2014 Nov-Dec:59(6):651-659. doi: 10.1111/jmwh.12222. Epub 2014 Oct 7 [PubMed PMID: 25294258]
Level 3 (low-level) evidenceSaloheimo AM. Paracervical block anesthesia in labor. Acta obstetricia et gynecologica Scandinavica. 1968:47(S5):1-21 [PubMed PMID: 5704597]
Aksoy H, Aksoy U, Ozyurt S, Ozoglu N, Acmaz G, Aydın T, İdem Karadağ Ö, Tayyar AT. Comparison of lidocaine spray and paracervical block application for pain relief during first-trimester surgical abortion: A randomised, double-blind, placebo-controlled trial. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology. 2016 Jul:36(5):649-53. doi: 10.3109/01443615.2016.1148681. Epub 2016 Feb 29 [PubMed PMID: 26926158]
Level 1 (high-level) evidenceChanrachakul B, Likittanasombut P, O-Prasertsawat P, Herabutya Y. Lidocaine versus plain saline for pain relief in fractional curettage: a randomized controlled trial. Obstetrics and gynecology. 2001 Oct:98(4):592-5 [PubMed PMID: 11576573]
Level 1 (high-level) evidenceGad C. Paracervical block. Acta obstetricia et gynecologica Scandinavica. 1967:46(1):7-18 [PubMed PMID: 6025358]
NYIRJESY I, HAWKS BL, HEBERT JE, HOPWOOD HG Jr, FALLS HC. HAZARDS OF THE USE OF PARACERVICAL BLOCK ANESTHESIA IN OBSTETRICS. American journal of obstetrics and gynecology. 1963 Sep 15:87():231-5 [PubMed PMID: 14077620]
Palomäki O, Huhtala H, Kirkinen P. A comparative study of the safety of 0.25% levobupivacaine and 0.25% racemic bupivacaine for paracervical block in the first stage of labor. Acta obstetricia et gynecologica Scandinavica. 2005 Oct:84(10):956-61 [PubMed PMID: 16167911]
Level 3 (low-level) evidenceBasol G, Kale A, Gurbuz H, Gundogdu EC, Baydilli KN, Usta T. Transvaginal pudendal nerve blocks in patients with pudendal neuralgia: 2-year follow-up results. Archives of gynecology and obstetrics. 2022 Oct:306(4):1107-1116. doi: 10.1007/s00404-022-06621-1. Epub 2022 May 28 [PubMed PMID: 35633372]
Liu J, Grayden DB, Keast JR, John SE. Endovascular stimulation of the pudendal nerve using a stent-mounted electrode array. Journal of neural engineering. 2024 Aug 13:21(4):. doi: 10.1088/1741-2552/ad6590. Epub 2024 Aug 13 [PubMed PMID: 39029495]
Naja MZ, Al-Tannir MA, Maaliki H, El-Rajab M, Ziade MF, Zeidan A. Nerve-stimulator-guided repeated pudendal nerve block for treatment of pudendal neuralgia. European journal of anaesthesiology. 2006 May:23(5):442-4 [PubMed PMID: 16573866]
Level 3 (low-level) evidence