Introduction
Pseudomyxoma peritonei (PMP) is a rare clinical entity, characterized by diffuse intra-abdominal gelatinous ascites, the so-called “jelly belly,” with mucinous implants on peritoneal surfaces.[1] Werth first introduced the term pseudomyxoma peritonei in 1884. It was initially believed to arise from a perforated cystadenoma of the appendix. However, currently, it has been more widely used to describe peritoneal dissemination of mucus-producing neoplasm most frequently from the appendix, but also small and large bowel, stomach, pancreas, lung, breast, gallbladder, fallopian tubes, and ovaries.[2][3] Due to its indolent behavior, pseudomyxoma peritonei is often discovered incidentally with a relatively advanced stage during laparoscopy, laparotomy or imaging studies for other medical concerns. Pseudomyxoma peritonei merits consideration as a ‘borderline malignancy’ with changing prognosis based on the site of origin.[4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Patients with familial adenomatous polyposis (FAP) demonstrate an increased risk of developing mucinous adenocarcinoma of the appendix. KRAS mutation has also been present in 70 % of appendiceal adenomas.[5]
Epidemiology
The estimated incidence of pseudomyxoma peritonei is approximately 1 to 4 out of a million annually.[3] The primary site is identified predominantly as mucinous appendiceal adenocarcinoma.[6] Patients have an average age of 53 years at the time of diagnosis. Females are affected more frequently than males.[7]
Pathophysiology
There are several steps involved in the pathogenesis of pseudomyxoma peritonei. Initially, tumor cells originating from the mucinous epithelium of the appendix continuously produce mucus into the appendiceal lumen and form a mucocele, which eventually ruptures. Free-floating mucinous epithelial tumor cells then implant in various parts of peritoneal cavity following the intraperitoneal fluid current and gravity, thanks to their absence of adhesive properties. It is termed as the so-called ‘redistribution phenomenon.’[8] The intraperitoneal fluid is most frequently reabsorbed through the right paracolic gutter toward the right hemidiaphragm and the greater and lesser omentum, thus becoming the major sites of tumor deposits when cells get trapped in small lymphatic systems. Gravity is another important redistribution mechanism, which facilitates the accumulation of tumor cells in the pelvis, such as the rectovesical pouch or the pouch of Douglas.
Mobile organs such as the small bowel and its mesentery are usually less likely to be involved compared to more fixed parts such as antrum, duodenojejunal flexure, ligament of Treitz, ileocecal and rectosigmoid region, early in the disease process. But in the end-stage disease, the entire peritoneal cavity could be engulfed.[9] The implanted tumor cells continue to proliferate and produce a large amount of mucus and eventually form mucinous ascites over months or even years. The excessive tumor burden and subsequent high intra-abdominal pressure can further limit bowel movement and even result in small bowel obstruction that requires surgical resection. The extra-peritoneal invasion has been reported mainly in the pleural cavity.[10] Lymphatic or hematogenic metastasis are rare occurrences.[3][7][11][12]
Histopathology
Macroscopic Findings:
Macroscopic examination often reveals abundant gelatinous pelvic or abdominal mucin or mucinous ascites accompanied by cystic epithelial implants on peritoneal surfaces. These lesions vary in size from a few mm to a few centimeters. A large ‘omental cake’ is also frequently found.[13]
Histopathology:
Multiple histological grading systems have been proposed for pseudomyxoma peritonei. Ronnett et al. first divided pseudomyxoma peritonei into two groups: disseminated peritoneal adenomucinosis (DPAM) and peritoneal mucinous carcinomatosis (PMCA).[14] DPAM is characterized by abundant mucus containing scanty mucinous epithelial cells with minimal cytological atypia and mitotic activity, while PMCA is featured by more abundant mucinous epithelial cells with high-grade cytological atypia and mitotic activity. In 2010, the World Health Organization (WHO) further refined the grading system.[15][16]
- Acellular mucin: Mucin within the peritoneal cavity without neoplastic epithelial cells.
- Low-grade mucinous carcinoma peritonei (synonymous with DPAM) presents as mucin pools with low cellularity (less than 10%), bland cytology and non-stratified cuboidal epithelium. Tumor cells are arranged in strips or gland-like structures. Infiltrative growth is not present.
- High-grade mucinous carcinoma peritonei (synonymous with PMCA): Mucin pools with high cellularity, moderate/severe cytological atypia, numerous mitoses, and cribriform growth pattern. Destructive infiltrative invasion of underlying organs is often present.
- High-grade mucinous carcinoma peritonei with signet ring cells: Any lesion with a component of signet ring cells, classified separately because of their worse prognosis.[17][18]
Immunohistochemistry:
Researchers have suggested MUC 2 over-expression as a molecular marker for PMP of intestinal origin.[19] Appendiceal tumors also express CK20, CEA, and CDX2, and are usually negative for CK7 and CA 125.[15] There are also reports of loss of protein expression of the repair genes MLH1 and PMS2.[20]
History and Physical
At the initial stage, pseudomyxoma peritonei is often asymptomatic or presents with non-specific signs and symptoms sometimes misdiagnosed as irritable bowel syndrome. As the disease progresses, patients may present with appendicitis-like symptoms, increased abdominal girth, the presence of pelvic masses or new-onset hernia. More advanced disease may result in abdominal distension, ascites, bowel obstruction, and nutritional compromise. Reports also exist of superinfected pseudomyxoma peritonei and subsequent sepsis.[21]
Physical examination may reveal a distended abdomen with a palpable omental cake. A rectal exam may reveal deposits in the pouch of Douglas or the rectovesical pouch. Ovarian masses may be palpable in females.
Evaluation
Imaging studies:
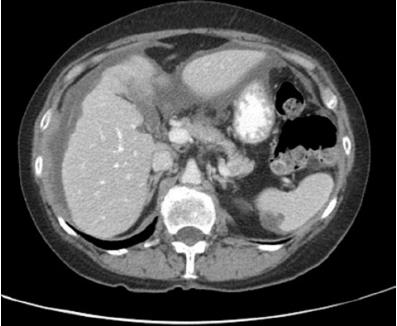
CT scan with contrast of the chest, abdomen, and pelvis is currently the imaging modality of choice for the diagnosis of pseudomyxoma peritonei. Typical CT appearance is ‘scalloping’ of the surface of the liver and spleen caused by loculated accumulations of mucin, which distinguishes mucin from fluid ascites. The mucinous material is similar in density to water. There are also islands of higher attenuation due to scattered solid elements and calcification within mucinous material. However, the primary appendiceal lesion might be absent or hard to identify on imaging. Compared to CT, gadolinium-enhanced MRI is more sensitive in localizing the tumor, and in assessing the small bowel as well as the hepatoduodenal ligament. PET/CT scan might be helpful in more aggressive variants by detecting extra-abdominal disease.[3]
Circulating tumor markers:
Tumor markers are found to have prognostic value and are useful for follow up of patients after treatment. CEA and CA 19.9 are found to have a high level in PMP with an appendiceal origin. CA 125 is also found to be high but with ovarian involvement.[15]
Histopathology:
The final diagnosis relies on histopathological examination of the biopsy and surgical specimen through laparoscopy or laparotomy, especially when the clinical and radiological manifestations are not specific. Percutaneous image-guided biopsies are of limited value since the resultant material may be acellular mucin.[22]
Treatment / Management
Traditional periodic surgical debulking has been less favored because of inevitable disease recurrence and a higher risk of repeated surgeries.[23] Current recommended standard treatment for PMP consists of complete cytoreduction surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC). The goal of CRS is to remove all visible tumors. Resection is considered complete if no masses larger than 2.5 mm are left.[24] HIPEC aims at eradicating any macroscopic or microscopic tumor residues. The most commonly used chemotherapeutic agent is mitomycin C (MMC), and the rationale for heating is to increase drug penetration. A baseline CT scan, as well as tumor markers, are recommended to be completed 3 months postoperatively and then every 6 months to monitor recurrence. Elective second look surgery when recurrence is considered for selected patients.[22][25] However, since CRS/HIPEC is an aggressive treatment, medical comorbidities should be carefully assessed preoperatively. And patients with high-grade lesions or signet ring cell components with an ECOG (Eastern Co-operative Oncology Group) performance score of 2 to 3 have significantly poorer overall survival after the surgery. Those patients may benefit from a major palliative resection to improve quality of life.[26] Postoperative systemic chemotherapy has been shown to benefit patients with high-grade neoplasm after CRS/HIPEC, but not those with low-grade neoplasm. However, there’s currently no widely accepted standardized plan. Preoperative systemic chemotherapy is generally not helpful.[27](B2)
Differential Diagnosis
- Ascites from another origin (cirrhosis, CHF)
- Ruptured mucinous cystadenomas of appendix or ovary
- Endometriosis with myxoid change
- Ruptured viscus with mucus extravasation
- Soft tissue neoplasms with myxoid changes
Prognosis
Prognosis of pseudomyxoma peritonei correlates closely to histopathological classification. The ten-year survival rate of patients with low-grade tumors/DPAM is 63% compared to 40.1% in patients with high-grade tumors/PMCA and 0% in patients with high-grade tumors with signet ring cells following the treatment of CRS/HIPEC in one recent study. [28] However data varies between different studies. [29][30][31][32] Above all, patients who are undergoing CRS/HIPEC present with a better long-term outcome than those undergoing debulking surgery.[33]
Complications
Major complications after CRS/HIPEC include thromboembolism, anastomotic leak, bowel perforation, fistula formation, abscess, and wound dehiscence. There is also a high risk for neutropenia, sepsis, pleural effusion, and respiratory insufficiency.[24][34]
Deterrence and Patient Education
Patient with a newly diagnosed pseudomyxoma peritonei is recommended to undergo CRS/HIPEC if medically fit with the goal of achieving complete cytoreduction. Even though the long-term outcomes after treatment are impressive for patients with low-grade histology, there’s still a significant recurrence of the disease. Regular follow-up is essential to monitor disease progression.
Enhancing Healthcare Team Outcomes
Most cases of pseudomyxoma peritonei are discovered in an advanced stage due to its indolent behavior. Pathological diagnosis is crucial to determine the treatment plan. When suspicious lesions are encountered incidentally during laparoscopy or laparotomy, the best strategy is to take generous biopsies, remove appendix if accessible, and only proceed with further treatment after pathological confirmation of the diagnosis and clinical assessment of the patient. During follow-up, the primary care provider, nurse practitioner or internist should be aware of recurrence and consider imaging studies and referral to the oncologist. Pseudomyxoma peritonei treatment is best in an interprofessional team approach including specialists, oncology trained specialty nursing, and when necessary, pharmacists, collaborating for optimal patient care and outcomes. [Level V]
Media
(Click Image to Enlarge)
References
Moran BJ, Cecil TD. The etiology, clinical presentation, and management of pseudomyxoma peritonei. Surgical oncology clinics of North America. 2003 Jul:12(3):585-603 [PubMed PMID: 14567019]
Darr U, Renno A, Alkully T, Khan Z, Tiwari A, Zeb W, Purdy J, Nawras A. Diagnosis of Pseudomyxoma peritonei via endoscopic ultrasound guided fine needle aspiration: a case report and review of literature. Scandinavian journal of gastroenterology. 2017 May:52(5):609-612. doi: 10.1080/00365521.2017.1284896. Epub 2017 Feb 3 [PubMed PMID: 28155576]
Level 3 (low-level) evidenceMittal R, Chandramohan A, Moran B. Pseudomyxoma peritonei: natural history and treatment. International journal of hyperthermia : the official journal of European Society for Hyperthermic Oncology, North American Hyperthermia Group. 2017 Aug:33(5):511-519. doi: 10.1080/02656736.2017.1310938. Epub [PubMed PMID: 28540829]
Baratti D, Kusamura S, Milione M, Pietrantonio F, Caporale M, Guaglio M, Deraco M. Pseudomyxoma Peritonei of Extra-Appendiceal Origin: A Comparative Study. Annals of surgical oncology. 2016 Dec:23(13):4222-4230 [PubMed PMID: 27352203]
Level 2 (mid-level) evidenceShih IM, Yan H, Speyrer D, Shmookler BM, Sugarbaker PH, Ronnett BM. Molecular genetic analysis of appendiceal mucinous adenomas in identical twins, including one with pseudomyxoma peritonei. The American journal of surgical pathology. 2001 Aug:25(8):1095-9 [PubMed PMID: 11474297]
Level 3 (low-level) evidenceSmeenk RM, van Velthuysen ML, Verwaal VJ, Zoetmulder FA. Appendiceal neoplasms and pseudomyxoma peritonei: a population based study. European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2008 Feb:34(2):196-201 [PubMed PMID: 17524597]
Level 2 (mid-level) evidenceGarcía KM, Flores KM, Ruiz A, González FL, Rodríguez ÁM. Pseudomyxoma Peritonei: Case Report and Literature Review. Journal of gastrointestinal cancer. 2019 Dec:50(4):1037-1042. doi: 10.1007/s12029-018-00192-8. Epub [PubMed PMID: 30618002]
Level 3 (low-level) evidenceSugarbaker PH. Pseudomyxoma peritonei. A cancer whose biology is characterized by a redistribution phenomenon. Annals of surgery. 1994 Feb:219(2):109-11 [PubMed PMID: 8129480]
Sulkin TV, O'Neill H, Amin AI, Moran B. CT in pseudomyxoma peritonei: a review of 17 cases. Clinical radiology. 2002 Jul:57(7):608-13 [PubMed PMID: 12096860]
Level 2 (mid-level) evidencePestieau SR, Esquivel J, Sugarbaker PH. Pleural extension of mucinous tumor in patients with pseudomyxoma peritonei syndrome. Annals of surgical oncology. 2000 Apr:7(3):199-203 [PubMed PMID: 10791850]
Level 2 (mid-level) evidenceSmeenk RM, Bruin SC, van Velthuysen ML, Verwaal VJ. Pseudomyxoma peritonei. Current problems in surgery. 2008 Aug:45(8):527-75. doi: 10.1067/j.cpsurg.2008.04.003. Epub [PubMed PMID: 18590843]
Rizvi SA, Syed W, Shergill R. Approach to pseudomyxoma peritonei. World journal of gastrointestinal surgery. 2018 Aug 27:10(5):49-56. doi: 10.4240/wjgs.v10.i5.49. Epub [PubMed PMID: 30190782]
Sugarbaker PH, Ronnett BM, Archer A, Averbach AM, Bland R, Chang D, Dalton RR, Ettinghausen SE, Jacquet P, Jelinek J, Koslowe P, Kurman RJ, Shmookler B, Stephens AD, Steves MA, Stuart OA, White S, Zahn CM, Zoetmulder FA. Pseudomyxoma peritonei syndrome. Advances in surgery. 1996:30():233-80 [PubMed PMID: 8960339]
Level 3 (low-level) evidenceRonnett BM, Zahn CM, Kurman RJ, Kass ME, Sugarbaker PH, Shmookler BM. Disseminated peritoneal adenomucinosis and peritoneal mucinous carcinomatosis. A clinicopathologic analysis of 109 cases with emphasis on distinguishing pathologic features, site of origin, prognosis, and relationship to "pseudomyxoma peritonei". The American journal of surgical pathology. 1995 Dec:19(12):1390-408 [PubMed PMID: 7503361]
Level 3 (low-level) evidenceRamaswamy V. Pathology of Mucinous Appendiceal Tumors and Pseudomyxoma Peritonei. Indian journal of surgical oncology. 2016 Jun:7(2):258-67. doi: 10.1007/s13193-016-0516-2. Epub 2016 Mar 19 [PubMed PMID: 27065718]
Carr NJ, Cecil TD, Mohamed F, Sobin LH, Sugarbaker PH, González-Moreno S, Taflampas P, Chapman S, Moran BJ, Peritoneal Surface Oncology Group International. A Consensus for Classification and Pathologic Reporting of Pseudomyxoma Peritonei and Associated Appendiceal Neoplasia: The Results of the Peritoneal Surface Oncology Group International (PSOGI) Modified Delphi Process. The American journal of surgical pathology. 2016 Jan:40(1):14-26. doi: 10.1097/PAS.0000000000000535. Epub [PubMed PMID: 26492181]
Level 3 (low-level) evidenceShetty S, Natarajan B, Thomas P, Govindarajan V, Sharma P, Loggie B. Proposed classification of pseudomyxoma peritonei: influence of signet ring cells on survival. The American surgeon. 2013 Nov:79(11):1171-6 [PubMed PMID: 24165252]
Level 2 (mid-level) evidenceCarr NJ, Bibeau F, Bradley RF, Dartigues P, Feakins RM, Geisinger KR, Gui X, Isaac S, Milione M, Misdraji J, Pai RK, Rodriguez-Justo M, Sobin LH, van Velthuysen MF, Yantiss RK. The histopathological classification, diagnosis and differential diagnosis of mucinous appendiceal neoplasms, appendiceal adenocarcinomas and pseudomyxoma peritonei. Histopathology. 2017 Dec:71(6):847-858. doi: 10.1111/his.13324. Epub 2017 Sep 19 [PubMed PMID: 28746986]
Ferreira CR, Carvalho JP, Soares FA, Siqueira SA, Carvalho FM. Mucinous ovarian tumors associated with pseudomyxoma peritonei of adenomucinosis type: immunohistochemical evidence that they are secondary tumors. International journal of gynecological cancer : official journal of the International Gynecological Cancer Society. 2008 Jan-Feb:18(1):59-65 [PubMed PMID: 17511804]
Level 2 (mid-level) evidenceFernandes ACO, Rocha GRMD, Oliveira AD, Guimarães MD, Carvalho SC, Chojniak R. Pseudomyxoma peritonei in a pediatric patient: A case report and literature review. Revista da Associacao Medica Brasileira (1992). 2018 Feb:64(2):195-199. doi: 10.1590/1806-9282.64.02.195. Epub [PubMed PMID: 29641675]
Level 3 (low-level) evidenceSullivan BJ, Bolton N, Sarpel U, Magge D. A unique presentation of superinfected pseudomyxoma peritonei secondary to a low-grade appendiceal mucinous neoplasm. World journal of surgical oncology. 2019 Feb 18:17(1):34. doi: 10.1186/s12957-019-1578-8. Epub 2019 Feb 18 [PubMed PMID: 30777068]
Bevan KE, Mohamed F, Moran BJ. Pseudomyxoma peritonei. World journal of gastrointestinal oncology. 2010 Jan 15:2(1):44-50. doi: 10.4251/wjgo.v2.i1.44. Epub [PubMed PMID: 21160816]
Hinson FL, Ambrose NS. Pseudomyxoma peritonei. The British journal of surgery. 1998 Oct:85(10):1332-9 [PubMed PMID: 9782010]
Chua TC, Moran BJ, Sugarbaker PH, Levine EA, Glehen O, Gilly FN, Baratti D, Deraco M, Elias D, Sardi A, Liauw W, Yan TD, Barrios P, Gómez Portilla A, de Hingh IH, Ceelen WP, Pelz JO, Piso P, González-Moreno S, Van Der Speeten K, Morris DL. Early- and long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2012 Jul 10:30(20):2449-56. doi: 10.1200/JCO.2011.39.7166. Epub 2012 May 21 [PubMed PMID: 22614976]
Smeenk RM, Verwaal VJ, Antonini N, Zoetmulder FA. Progression of pseudomyxoma peritonei after combined modality treatment: management and outcome. Annals of surgical oncology. 2007 Feb:14(2):493-9 [PubMed PMID: 17103067]
Level 2 (mid-level) evidenceStewart JH 4th, Shen P, Levine EA. Intraperitoneal hyperthermic chemotherapy for peritoneal surface malignancy: current status and future directions. Annals of surgical oncology. 2005 Oct:12(10):765-77 [PubMed PMID: 16132375]
Level 3 (low-level) evidenceBlackham AU, Swett K, Eng C, Sirintrapun J, Bergman S, Geisinger KR, Votanopoulos K, Stewart JH, Shen P, Levine EA. Perioperative systemic chemotherapy for appendiceal mucinous carcinoma peritonei treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Journal of surgical oncology. 2014 Jun:109(7):740-5. doi: 10.1002/jso.23547. Epub 2013 Dec 28 [PubMed PMID: 24375188]
Level 2 (mid-level) evidenceBaratti D, Kusamura S, Milione M, Bruno F, Guaglio M, Deraco M. Validation of the Recent PSOGI Pathological Classification of Pseudomyxoma Peritonei in a Single-Center Series of 265 Patients Treated by Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy. Annals of surgical oncology. 2018 Feb:25(2):404-413. doi: 10.1245/s10434-017-6252-1. Epub 2017 Nov 20 [PubMed PMID: 29159742]
Level 1 (high-level) evidencePallas N, Karamveri C, Kyziridis D, Hristakis C, Kyriakopoulos V, Kalakonas A, Vaikos D, Tentes AK. Cytoreductive surgery and hyperthermic intraperitenoal chemotherapy (HIPEC) for colorectal and appendiceal carcinomas with peritoneal carcinomatosis. Journal of B.U.ON. : official journal of the Balkan Union of Oncology. 2017 Nov-Dec:22(6):1547-1553 [PubMed PMID: 29332351]
McQuellon RP, Russell GB, Shen P, Stewart JH 4th, Saunders W, Levine EA. Survival and health outcomes after cytoreductive surgery with intraperitoneal hyperthermic chemotherapy for disseminated peritoneal cancer of appendiceal origin. Annals of surgical oncology. 2008 Jan:15(1):125-33 [PubMed PMID: 18030535]
Moran B, Cecil T, Chandrakumaran K, Arnold S, Mohamed F, Venkatasubramaniam A. The results of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in 1200 patients with peritoneal malignancy. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland. 2015 Sep:17(9):772-8. doi: 10.1111/codi.12975. Epub [PubMed PMID: 25880479]
Chua TC, Yan TD, Saxena A, Morris DL. Should the treatment of peritoneal carcinomatosis by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy still be regarded as a highly morbid procedure?: a systematic review of morbidity and mortality. Annals of surgery. 2009 Jun:249(6):900-7. doi: 10.1097/SLA.0b013e3181a45d86. Epub [PubMed PMID: 19474692]
Level 1 (high-level) evidenceJärvinen P, Ristimäki A, Kantonen J, Aronen M, Huuhtanen R, Järvinen H, Lepistö A. Comparison of serial debulking and cytoreductive surgery with hyperthermic intraperitoneal chemotherapy in pseudomyxoma peritonei of appendiceal origin. International journal of colorectal disease. 2014 Aug:29(8):999-1007. doi: 10.1007/s00384-014-1933-8. Epub 2014 Jun 26 [PubMed PMID: 24965858]
Sugarbaker PH, Ryan DP. Cytoreductive surgery plus hyperthermic perioperative chemotherapy to treat peritoneal metastases from colorectal cancer: standard of care or an experimental approach? The Lancet. Oncology. 2012 Aug:13(8):e362-9. doi: 10.1016/S1470-2045(12)70210-3. Epub [PubMed PMID: 22846841]