Introduction
Pituitary apoplexy is a condition in which there is a hemorrhage or infarction of the pituitary gland. This disorder usually occurs in a pre-existing pituitary adenoma.[1][2][3] The term pituitary apoplexy or apoplexia refers to the "sudden death" of the pituitary gland, usually caused by an acute ischemic infarction or hemorrhage. Pearce Bailey described the first case of pituitary tumor-associated hemorrhage in 1898, but the term pituitary apoplexy referring to both necrosis and bleeding into pituitary tumors was first used in 1950 by Brougham et al.[4] Pituitary apoplexy is a medical and surgical emergency in many cases. Prompt identification and evaluation are imperative to improve outcomes.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
A pre-existing pituitary adenoma is usually found in cases of pituitary apoplexy. In the majority of the cases, the patients are unaware of the tumor.[5] Several predisposing or contributing factors for pituitary apoplexy include endocrine stimulation tests,[6] bromocriptine or cabergoline treatment,[7][8] gonadotropin-releasing hormone treatment,[9] lumbar fusion in the prone position,[10][11] pregnancy,[12][13] pituitary irradiation,[14] anticoagulation,[15] thrombocytopenia,[16][17] and erectile dysfunction medications.[18]
Sheehan syndrome occurs in postpartum women in which there is necrosis of the pituitary gland secondary to ischemia after significant bleeding during childbirth. It will present with adrenal insufficiency, hypothyroidism, and hypopituitarism, but rarely with visual changes. Most of the time, this entity is not included as a pituitary apoplexy as the gland did not have a pre-existing tumor, and visual symptoms are extremely rare.
Epidemiology
The reported incidence of pituitary apoplexy varies significantly from 1.5-27.7% in cases of pituitary adenoma, but many of them do not distinguish between symptomatic and asymptomatic patients. When symptomatic cases only are included, the incidence approaches 10%.[2][19][20][21] If non-symptomatic intratumoral hemorrhage detected by neuroimaging studies is considered, the incidence increases to 26%. Apoplexy in pituitary adenomas is rare and is estimated at 0.2% annually. Tumors larger than 10 cm have a higher risk, and those in which rapid growth has been documented.[22]
Most patients fall in the age range of 37-58 years.[23] There is a male-to-female ratio approaching 2:1.[21][23][24]
Pathophysiology
Hemorrhage produces an acute expansion of the tumor, which produces many of the symptoms. Visual symptoms are caused by direct compression of the optic nerves or chiasm, and hormonal dysfunction is caused by the sudden interruption of the release of the hormones.
Several theories had been proposed to explain the ischemic and hemorrhagic changes found in the tumor and the normal gland. Although they are proposed as separate mechanisms, probably each theory contributes to some process, and the combination of them is what ultimately produces the apoplexy. One theory postulates that the compression of the superior hypophyseal artery and its branches against the diaphragma sella leads to ischemia of the anterior pituitary gland and the tumor.[2][3][25] Another theory proposes that the thin pituitary vascular network is compressed as it is located inside the small intrasellar compartment causing ischemia, necrosis, and hemorrhage.[2][3][26] Lastly, another theory stipulates that the rapid expansion of the tumor outstrips its vascular supply, resulting in ischemia and necrosis.[2][3][27]
History and Physical
A sudden-onset headache located behind the eyes is the most common symptom.[3][28] Several mechanisms have been postulated to explain the headache in pituitary apoplexy and include involvement of the superior division of the trigeminal nerve inside the cavernous sinus, meningeal irritation, dura-mater compression, or enlargement of sellar walls. Other symptoms include decreased visual acuity, hemianopia, diplopia, ptosis, nausea and vomiting, altered mental status, and hormonal dysfunction.[2][28][29][30][31] Many patients complain of double vision, which is caused by extrinsic compression of one or several of the extraocular nerves. The oculomotor is the nerve most commonly affected.[23] Patients will have ptosis and lateral eye deviation, sometimes accompanied by pupillary dilation of the affected eye.
In pituitary apoplexy, the most impacting clinical problem is the lack of secretion of adrenocorticotropic hormone (ACTH), which occurs in more than two-thirds of the patients with apoplexy. The lack of secretion causes a cessation of cortisol secretion by the adrenal gland, which produces a variety of symptoms called "adrenal crisis."[2][3] The patient may have nausea and vomiting, abdominal pain, bradycardia and hypotension, hypothermia, lethargy, and sometimes coma.
Evaluation
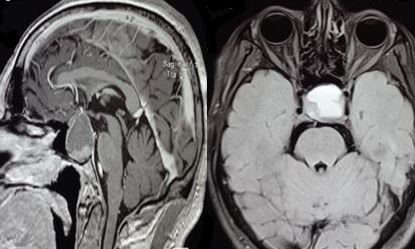
Computed tomographic (CT) scan: Non-contrast head CT scan is usually performed first as it is easier to obtain. It will show a sellar/suprasellar mass associated with intralesional hemorrhage. Ischemia or necrosis of the gland/tumor can not be identified. Contrast examination is done afterward to delimit the size of the tumor as the hemorrhagic products, and contrast-enhancing areas are hyperdense to the brain.
Magnetic resonance imaging (MRI): Brain MRI is performed to improve the definition of the lesion. MRI is the diagnostic imaging modality of choice.[2][23] It can easily identify hemorrhagic and necrotic areas. The characteristic brain MRI finding in an ischemic pituitary apoplexy is an enlarged sellar/suprasellar mass with peripheral enhancement surrounding a hypointense center. Diffusion-weighted imaging provides information about the consistency of the tumor and is very useful to identify ischemic tissue after arterial occlusion has occurred.[2] For a hemorrhagic apoplexy, T1-weighted MRI shows a sellar/suprasellar lesion with intralesional areas of high signal intensity, suggesting the presence of blood.[3] The MRI gradient-echo sequence T2-star weighted (T2*W), is very sensitive to detect deposits of hemosiderin.[2]
Hormonal evaluation: Pituitary hormonal evaluation is required, as nearly 80% of patients present with a deficiency of at least one of the anterior pituitary hormones.[1] The most common deficiencies are growth hormone deficit in 90% of the patients and ACTH deficit in 70% of them.[2][32]
Grading system: A 5-grade classification based on the clinical presentation spectrum had been recently proposed for treatment decisions and outcomes.[33]
Treatment / Management
Immediate medical management of patients with pituitary apoplexy includes a careful assessment of fluids and electrolyte balance, ensure hemodynamic stability, and replacement with corticosteroids.[32] All patients should receive corticosteroids even if they do not present symptoms of adrenal crisis. The recommended dose is an intravenous 100–200 mg bolus of hydrocortisone. Additional administration of 50-100 mg every 6 hours should be continued. Alternatively, a continuous intravenous infusion of 2-4 mg/hour can be started after the initial bolus.[3]
Management of the mass is controversial as some advocate early transsphenoidal surgical decompression in all patients, whereas others adopt a conservative approach for those patients without visual acuity or field defects and with normal consciousness. Emergency surgery should be reserved for patients with progressive deterioration of consciousness, hypothalamic involvement, and progressive visual worsening. It has been demonstrated that a significant postoperative clinical improvement is a consequence of a surgical procedure performed as soon as possible.[23] Decompressive surgery can be delayed but performed within 1 week when visual acuity defects appear stable. If ophthalmoplegia is improving or stable, a conservative strategy could be considered.[34][35] Microscopic endonasal or sublabial transsphenoidal surgery is commonly used. For very large tumors and those extending over the chiasm or laterally to the temporal fossa, a craniotomy should be used to achieve complete resection. Endoscopic endonasal approaches for pituitary apoplexy are effective.[30][36][37] Patients operated using the endoscopic approach have a similar visual outcome, but a better endocrinological outcome as the viable tumoral component can be removed from restricted areas like the cavernous sinus.[38] Sometimes, an endoscopic approach can prove difficult to perform if required at late night hours as it needs the collaboration of an otolaryngologist with the neurosurgeon. (B2)
Pediatric pituitary tumor apoplexy has a more aggressive natural history in comparison to adults, and early surgery may reduce its occurrence and improve outcomes.[39][40](B2)
Differential Diagnosis
Several conditions have to be excluded as they can present with similar visual, ophthalmoplegic, and headache symptoms that occur in pituitary apoplexy. Some of the conditions will only require medical treatment, while in others, the surgical treatment is completely different.
Prognosis
Pituitary apoplexy can be a life-threatening condition if not detected and treated. The overall mortality is 1.6% to 1.9%.
Visual acuity, visual field defects, and ophthalmoplegia improve in the majority of the patients after both conservative and surgical decompression. After surgery, such improvement can be observed in the immediate postoperative period and often continues for several weeks after surgery. Visual recovery has been reported to be less likely in patients presenting with monocular or binocular blindness. Although visual outcome appears to be better with early intervention as compared to late,[48] others found that visual deficits, resolution of oculomotor palsy, recovery from hypopituitarism, or non-neuroendocrine signs and symptoms such as headache and encephalopathy do not depend on the timing of surgery.[49] A complete restoration of the oculomotor palsy usually needs 3 months, while abducens nerve palsy usually needs 6 months.[23] Overall, visual improvement is seen in 75 to 85% of patients, recovery of normal vision in 38% of patients, and rectification of preoperative oculomotor palsies in 81% of patients.[30]
Gross total resection and short duration of preoperative headaches are predictors for improvement in postoperative headaches.[50] Hormonal replacement therapy is needed in 80% of the patients.[1][21][49] In some cases that are treated conservatively, spontaneous remission of the tumor has occurred, and surgery is not required.[51][52] This may be caused by ischemic necrosis of the tumoral tissue.
Complications
Consultations
- Neurosurgery
- Hospitalist
- Ophthalmology
- Endocrinology
Deterrence and Patient Education
Patients with pituitary apoplexy may have a long residual endocrine deficiency and should have an assessment of pituitary function at 4 to 8 weeks after the event. Assessment of visual acuity, eye movements, and visual fields is mandatory. An MRI scan is recommended at 3 to 6 months after an episode to evaluate for residual tumor, and thereafter an annual MRI scan should be considered for the next 5 years.
Those patients with a known tumor should be educated about the possibility of hemorrhage. They should be encouraged to attend their endocrinologist and neurosurgeon scheduled visits. Any acute visual change or significant headache should alert them to seek immediate medical evaluation.
Enhancing Healthcare Team Outcomes
Pituitary apoplexy frequently poses a diagnostic dilemma. These patients may exhibit non-specific signs and symptoms such as headache, vomiting, and nausea. Sometimes, visual problems alert the patient of a more serious problem. The diagnosis is difficult to recognize without proper imaging studies.
While the neurosurgeon is almost always involved in the care of patients with pituitary apoplexy, it is important to consult with an interprofessional team of specialists that include an endocrinologist and ophthalmologist. The nurses are also vital members of the interprofessional team as they will monitor the patient's vital signs and assist with the education of the patient and family. Those patients with adrenal crisis have to be monitored in an intensive care unit until hemodynamically stable. In the postoperative period for pain, wound infection prophylaxis, and hormonal replacement, the pharmacist will ensure that the patient is on the right analgesics, hormonal replacements, and appropriate antibiotics. The neuroradiologist also plays a vital role in determining if pituitary apoplexy is secondary to hemorrhage or ischemia. Without providing a proper history, the neuroradiologist may not be sure what to look for or what additional radiologic exams may be needed.
Media
References
Ranabir S, Baruah MP. Pituitary apoplexy. Indian journal of endocrinology and metabolism. 2011 Sep:15 Suppl 3(Suppl3):S188-96. doi: 10.4103/2230-8210.84862. Epub [PubMed PMID: 22029023]
Briet C, Salenave S, Bonneville JF, Laws ER, Chanson P. Pituitary Apoplexy. Endocrine reviews. 2015 Dec:36(6):622-45. doi: 10.1210/er.2015-1042. Epub 2015 Sep 28 [PubMed PMID: 26414232]
Briet C, Salenave S, Chanson P. Pituitary apoplexy. Endocrinology and metabolism clinics of North America. 2015 Mar:44(1):199-209. doi: 10.1016/j.ecl.2014.10.016. Epub 2014 Nov 5 [PubMed PMID: 25732655]
BROUGHAM M,HEUSNER AP,ADAMS RD, Acute degenerative changes in adenomas of the pituitary body--with special reference to pituitary apoplexy. Journal of neurosurgery. 1950 Sep; [PubMed PMID: 14774761]
Biousse V, Newman NJ, Oyesiku NM. Precipitating factors in pituitary apoplexy. Journal of neurology, neurosurgery, and psychiatry. 2001 Oct:71(4):542-5 [PubMed PMID: 11561045]
Kuzu F, Unal M, Gul S, Bayraktaroglu T. Pituitary Apoplexy due to the Diagnostic Test in a Cushing"s Disease Patient. Turkish neurosurgery. 2018:28(2):323-325. doi: 10.5137/1019-5149.JTN.16730-15.1. Epub [PubMed PMID: 27593808]
Ghadirian H, Shirani M, Ghazi-Mirsaeed S, Mohebi S, Alimohamadi M. Pituitary Apoplexy during Treatment of Prolactinoma with Cabergoline. Asian journal of neurosurgery. 2018 Jan-Mar:13(1):93-95. doi: 10.4103/1793-5482.181130. Epub [PubMed PMID: 29492132]
Aydin B,Aksu O,Asci H,Kayan M,Korkmaz H, A RARE CAUSE OF PITUITARY APOPLEXY: CABERGOLINE THERAPY. Acta endocrinologica (Bucharest, Romania : 2005). 2018 Jan-Mar; [PubMed PMID: 31149244]
Keane F, Egan AM, Navin P, Brett F, Dennedy MC. Gonadotropin-releasing hormone agonist-induced pituitary apoplexy. Endocrinology, diabetes & metabolism case reports. 2016:2016():160021. doi: 10.1530/EDM-16-0021. Epub 2016 Jun 8 [PubMed PMID: 27284452]
Joo C, Ha G, Jang Y. Pituitary apoplexy following lumbar fusion surgery in prone position: A case report. Medicine. 2018 May:97(19):e0676. doi: 10.1097/MD.0000000000010676. Epub [PubMed PMID: 29742711]
Level 3 (low-level) evidenceAkakın A, Yılmaz B, Ekşi MŞ, Kılıç T. A case of pituitary apoplexy following posterior lumbar fusion surgery. Journal of neurosurgery. Spine. 2015 Nov:23(5):598-601. doi: 10.3171/2015.3.SPINE14792. Epub 2015 Aug 7 [PubMed PMID: 26252784]
Level 3 (low-level) evidenceJemel M, Kandara H, Riahi M, Gharbi R, Nagi S, Kamoun I. Gestational pituitary apoplexy: Case series and review of the literature. Journal of gynecology obstetrics and human reproduction. 2019 Dec:48(10):873-881. doi: 10.1016/j.jogoh.2019.05.005. Epub 2019 May 3 [PubMed PMID: 31059861]
Level 2 (mid-level) evidenceAnnamalai AK, Jeyachitra G, Jeyamithra A, Ganeshkumar M, Srinivasan KG, Gurnell M. Gestational Pituitary Apoplexy. Indian journal of endocrinology and metabolism. 2017 May-Jun:21(3):484-485. doi: 10.4103/ijem.IJEM_8_17. Epub [PubMed PMID: 28553611]
Yu J, Li Y, Quan T, Li X, Peng C, Zeng J, Liang S, Huang M, He Y, Deng Y. Initial Gamma Knife radiosurgery for nonfunctioning pituitary adenomas: results from a 26-year experience. Endocrine. 2020 May:68(2):399-410. doi: 10.1007/s12020-020-02260-1. Epub 2020 Mar 11 [PubMed PMID: 32162186]
Ly S,Naman A,Chaufour-Higel B,Patey M,Arndt C,Delemer B,Litre CF, Pituitary apoplexy and rivaroxaban. Pituitary. 2017 Dec; [PubMed PMID: 28831662]
Thomas M, Robert A, Rajole P, Robert P. A Rare Case of Pituitary Apoplexy Secondary to Dengue Fever-induced Thrombocytopenia. Cureus. 2019 Aug 5:11(8):e5323. doi: 10.7759/cureus.5323. Epub 2019 Aug 5 [PubMed PMID: 31428546]
Level 3 (low-level) evidenceBalaparameswara Rao SJ, Savardekar AR, Nandeesh BN, Arivazhagan A. Management dilemmas in a rare case of pituitary apoplexy in the setting of dengue hemorrhagic fever. Surgical neurology international. 2017:8():4. doi: 10.4103/2152-7806.198731. Epub 2017 Jan 19 [PubMed PMID: 28217383]
Level 3 (low-level) evidenceUneda A, Hirashita K, Yunoki M, Yoshino K, Date I. Pituitary adenoma apoplexy associated with vardenafil intake. Acta neurochirurgica. 2019 Jan:161(1):129-131. doi: 10.1007/s00701-018-3763-x. Epub 2018 Dec 12 [PubMed PMID: 30542775]
Mohr G,Hardy J, Hemorrhage, necrosis, and apoplexy in pituitary adenomas. Surgical neurology. 1982 Sep; [PubMed PMID: 7179072]
Level 3 (low-level) evidenceMohanty S, Tandon PN, Banerji AK, Prakash B. Haemorrhage into pituitary adenomas. Journal of neurology, neurosurgery, and psychiatry. 1977 Oct:40(10):987-91 [PubMed PMID: 591978]
Level 3 (low-level) evidenceMurad-Kejbou S, Eggenberger E. Pituitary apoplexy: evaluation, management, and prognosis. Current opinion in ophthalmology. 2009 Nov:20(6):456-61. doi: 10.1097/ICU.0b013e3283319061. Epub [PubMed PMID: 19809320]
Level 3 (low-level) evidenceFernández-Balsells MM, Murad MH, Barwise A, Gallegos-Orozco JF, Paul A, Lane MA, Lampropulos JF, Natividad I, Perestelo-Pérez L, Ponce de León-Lovatón PG, Erwin PJ, Carey J, Montori VM. Natural history of nonfunctioning pituitary adenomas and incidentalomas: a systematic review and metaanalysis. The Journal of clinical endocrinology and metabolism. 2011 Apr:96(4):905-12. doi: 10.1210/jc.2010-1054. Epub [PubMed PMID: 21474687]
Level 1 (high-level) evidenceRicciuti R, Nocchi N, Arnaldi G, Polonara G, Luzi M. Pituitary Adenoma Apoplexy: Review of Personal Series. Asian journal of neurosurgery. 2018 Jul-Sep:13(3):560-564. doi: 10.4103/ajns.AJNS_344_16. Epub [PubMed PMID: 30283505]
Nawar RN, AbdelMannan D, Selman WR, Arafah BM. Pituitary tumor apoplexy: a review. Journal of intensive care medicine. 2008 Mar-Apr:23(2):75-90. doi: 10.1177/0885066607312992. Epub [PubMed PMID: 18372348]
Cardoso ER, Peterson EW. Pituitary apoplexy: a review. Neurosurgery. 1984 Mar:14(3):363-73 [PubMed PMID: 6369168]
Rovit RL, Fein JM. Pituitary apoplexy: a review and reappraisal. Journal of neurosurgery. 1972 Sep:37(3):280-8 [PubMed PMID: 5069376]
Epstein S, Pimstone BL, De Villiers JC, Jackson WP. Pituitary apoplexy in five patients with pituitary tumours. British medical journal. 1971 May 1:2(5756):267-70 [PubMed PMID: 5572390]
Grzywotz A, Kleist B, Möller LC, Hans VH, Göricke S, Sure U, Müller O, Kreitschmann-Andermahr I. Pituitary apoplexy - A single center retrospective study from the neurosurgical perspective and review of the literature. Clinical neurology and neurosurgery. 2017 Dec:163():39-45. doi: 10.1016/j.clineuro.2017.10.006. Epub 2017 Oct 10 [PubMed PMID: 29055223]
Level 2 (mid-level) evidenceWichlińska-Lubińska M, Kozera G. Pituitary apoplexy. Neurologia i neurochirurgia polska. 2019:53(6):413-420. doi: 10.5603/PJNNS.a2019.0054. Epub 2019 Nov 20 [PubMed PMID: 31745969]
Zoli M, Milanese L, Faustini-Fustini M, Guaraldi F, Asioli S, Zenesini C, Righi A, Frank G, Foschini MP, Sturiale C, Pasquini E, Mazzatenta D. Endoscopic Endonasal Surgery for Pituitary Apoplexy: Evidence On a 75-Case Series From a Tertiary Care Center. World neurosurgery. 2017 Oct:106():331-338. doi: 10.1016/j.wneu.2017.06.117. Epub 2017 Jun 30 [PubMed PMID: 28669873]
Level 2 (mid-level) evidenceBarkhoudarian G, Kelly DF. Pituitary Apoplexy. Neurosurgery clinics of North America. 2019 Oct:30(4):457-463. doi: 10.1016/j.nec.2019.06.001. Epub 2019 Aug 7 [PubMed PMID: 31471052]
Veldhuis JD, Hammond JM. Endocrine function after spontaneous infarction of the human pituitary: report, review, and reappraisal. Endocrine reviews. 1980 Winter:1(1):100-7 [PubMed PMID: 6785084]
Jho DH, Biller BM, Agarwalla PK, Swearingen B. Pituitary apoplexy: large surgical series with grading system. World neurosurgery. 2014 Nov:82(5):781-90. doi: 10.1016/j.wneu.2014.06.005. Epub 2014 Jun 8 [PubMed PMID: 24915069]
Level 2 (mid-level) evidenceAlmeida JP, Sanchez MM, Karekezi C, Warsi N, Fernández-Gajardo R, Panwar J, Mansouri A, Suppiah S, Nassiri F, Nejad R, Kucharczyk W, Ridout R, Joaquim AF, Gentili F, Zadeh G. Pituitary Apoplexy: Results of Surgical and Conservative Management Clinical Series and Review of the Literature. World neurosurgery. 2019 Oct:130():e988-e999. doi: 10.1016/j.wneu.2019.07.055. Epub 2019 Jul 11 [PubMed PMID: 31302273]
Seo Y, Kim YH, Dho YS, Kim JH, Kim JW, Park CK, Kim DG. The Outcomes of Pituitary Apoplexy with Conservative Treatment: Experiences at a Single Institution. World neurosurgery. 2018 Jul:115():e703-e710. doi: 10.1016/j.wneu.2018.04.139. Epub 2018 Apr 27 [PubMed PMID: 29709755]
Pangal DJ, Chesney K, Memel Z, Bonney PA, Strickland BA, Carmichael J, Shiroishi M, Jason Liu CS, Zada G. Pituitary Apoplexy Case Series: Outcomes After Endoscopic Endonasal Transsphenoidal Surgery at a Single Tertiary Center. World neurosurgery. 2020 May:137():e366-e372. doi: 10.1016/j.wneu.2020.01.204. Epub 2020 Feb 4 [PubMed PMID: 32032792]
Level 2 (mid-level) evidenceZhan R, Li X, Li X. Endoscopic Endonasal Transsphenoidal Approach for Apoplectic Pituitary Tumor: Surgical Outcomes and Complications in 45 Patients. Journal of neurological surgery. Part B, Skull base. 2016 Feb:77(1):54-60. doi: 10.1055/s-0035-1560046. Epub 2015 Aug 20 [PubMed PMID: 26949589]
Teixeira JC, Lavrador J, Simão D, Miguéns J. Pituitary Apoplexy: Should Endoscopic Surgery Be the Gold Standard? World neurosurgery. 2018 Mar:111():e495-e499. doi: 10.1016/j.wneu.2017.12.103. Epub 2017 Dec 26 [PubMed PMID: 29288106]
Culpin E, Crank M, Igra M, Connolly DJA, Dimitri P, Mirza S, Sinha S. Pituitary tumour apoplexy within prolactinomas in children: a more aggressive condition? Pituitary. 2018 Oct:21(5):474-479. doi: 10.1007/s11102-018-0900-8. Epub [PubMed PMID: 30014342]
Zhang N, Zhou P, Meng Y, Ye F, Jiang S. A retrospective review of 34 cases of pediatric pituitary adenoma. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2017 Nov:33(11):1961-1967. doi: 10.1007/s00381-017-3538-3. Epub 2017 Jul 18 [PubMed PMID: 28721598]
Level 2 (mid-level) evidenceMartinez Santos J, Hannay M, Olar A, Eskandari R. Rathke's Cleft Cyst Apoplexy in Two Teenage Sisters. Pediatric neurosurgery. 2019:54(6):428-435. doi: 10.1159/000503112. Epub 2019 Oct 21 [PubMed PMID: 31634887]
Jung HN, Kim ST, Kong DS, Suh SI, Ryoo I. Rathke Cleft Cysts with Apoplexy-Like Symptoms: Clinicoradiologic Comparisons with Pituitary Adenomas with Apoplexy. World neurosurgery. 2020 Oct:142():e1-e9. doi: 10.1016/j.wneu.2020.03.086. Epub 2020 Mar 23 [PubMed PMID: 32217176]
Schooner L, Wedemeyer MA, Bonney PA, Lin M, Hurth K, Mathew A, Liu CJ, Shiroishi M, Carmichael JD, Weiss MH, Zada G. Hemorrhagic Presentation of Rathke Cleft Cysts: A Surgical Case Series. Operative neurosurgery (Hagerstown, Md.). 2020 May 1:18(5):470-479. doi: 10.1093/ons/opz239. Epub [PubMed PMID: 31504863]
Level 2 (mid-level) evidencePedro B, Patrícia T, Aldomiro F. Pituitary Apoplexy May Be Mistaken for Temporal Arteritis. European journal of case reports in internal medicine. 2019:6(11):001261. doi: 10.12890/2019_001261. Epub 2019 Oct 16 [PubMed PMID: 31890705]
Level 3 (low-level) evidenceChoudhury M, Eligar V, DeLloyd A, Davies JS. A case of pituitary apoplexy masquerading as subarachnoid hemorrhage. Clinical case reports. 2016 Mar:4(3):255-7. doi: 10.1002/ccr3.488. Epub 2016 Jan 22 [PubMed PMID: 27014446]
Level 3 (low-level) evidenceLaw-Ye B, Pyatigorskaya N, Leclercq D. Pituitary Apoplexy Mimicking Bacterial Meningitis with Intracranial Hypertension. World neurosurgery. 2017 Jan:97():748.e3-748.e5. doi: 10.1016/j.wneu.2016.10.032. Epub 2016 Oct 15 [PubMed PMID: 27756666]
Shabas D, Sheikh HU, Gilad R. Pituitary Apoplexy Presenting as Status Migrainosus. Headache. 2017 Apr:57(4):641-642. doi: 10.1111/head.13046. Epub 2017 Feb 9 [PubMed PMID: 28181226]
Abdulbaki A, Kanaan I. The impact of surgical timing on visual outcome in pituitary apoplexy: Literature review and case illustration. Surgical neurology international. 2017:8():16. doi: 10.4103/2152-7806.199557. Epub 2017 Feb 6 [PubMed PMID: 28217395]
Level 3 (low-level) evidenceRutkowski MJ, Kunwar S, Blevins L, Aghi MK. Surgical intervention for pituitary apoplexy: an analysis of functional outcomes. Journal of neurosurgery. 2018 Aug:129(2):417-424. doi: 10.3171/2017.2.JNS1784. Epub 2017 Sep 15 [PubMed PMID: 28946177]
Suri H, Dougherty C. Presentation and Management of Headache in Pituitary Apoplexy. Current pain and headache reports. 2019 Jul 29:23(9):61. doi: 10.1007/s11916-019-0798-5. Epub 2019 Jul 29 [PubMed PMID: 31359174]
Eichberg DG, Di L, Shah AH, Kaye WA, Komotar RJ. Spontaneous preoperative pituitary adenoma resolution following apoplexy: a case presentation and literature review. British journal of neurosurgery. 2020 Oct:34(5):502-507. doi: 10.1080/02688697.2018.1529737. Epub 2018 Nov 19 [PubMed PMID: 30450986]
Level 3 (low-level) evidenceSouteiro P, Belo S, Carvalho D. A rare case of spontaneous Cushing disease remission induced by pituitary apoplexy. Journal of endocrinological investigation. 2017 May:40(5):555-556. doi: 10.1007/s40618-017-0645-7. Epub 2017 Mar 1 [PubMed PMID: 28251551]
Level 3 (low-level) evidenceGambaracci G,Rondoni V,Guercini G,Floridi P, Pituitary apoplexy complicated by vasospasm and bilateral cerebral infarction. BMJ case reports. 2016 Jun 21; [PubMed PMID: 27329099]
Level 3 (low-level) evidenceAbbas MS, AlBerawi MN, Al Bozom I, Shaikh NF, Salem KY. Unusual Complication of Pituitary Macroadenoma: A Case Report and Review. The American journal of case reports. 2016 Oct 6:17():707-711 [PubMed PMID: 27708253]
Level 3 (low-level) evidenceZou Z, Liu C, Sun B, Chen C, Xiong W, Che C, Huang H. Surgical treatment of pituitary apoplexy in association with hemispheric infarction. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2015 Oct:22(10):1550-4. doi: 10.1016/j.jocn.2015.03.049. Epub 2015 Jul 23 [PubMed PMID: 26213287]