Anatomy, Bony Pelvis and Lower Limb: Calf Peroneus Longus Muscle
Anatomy, Bony Pelvis and Lower Limb: Calf Peroneus Longus Muscle
Introduction
The peroneus longus muscle is one of two muscles in the lateral compartment of the lower limb, along with the peroneus brevis muscle.[1] The lateral compartment receives innervation from the superficial peroneal nerve (L5-S2), supplied by the anterior tibial and peroneal arteries. It is important in plantar flexion and eversion of the foot and ankle. The peroneus longus muscle is susceptible to several pathologies, including tendonitis, tendon dislocation, subluxation, rupture, and acute and chronic compartment syndrome.[2][3]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
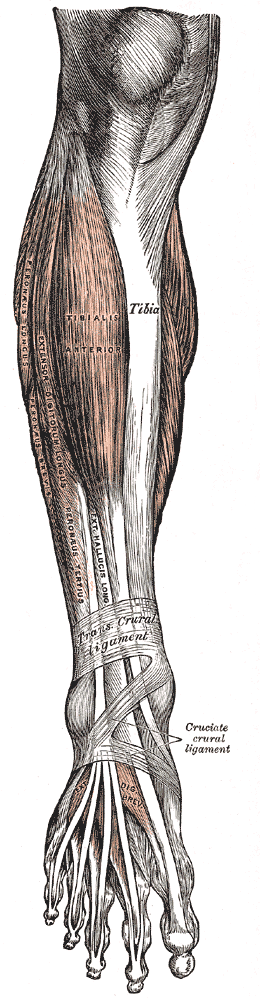
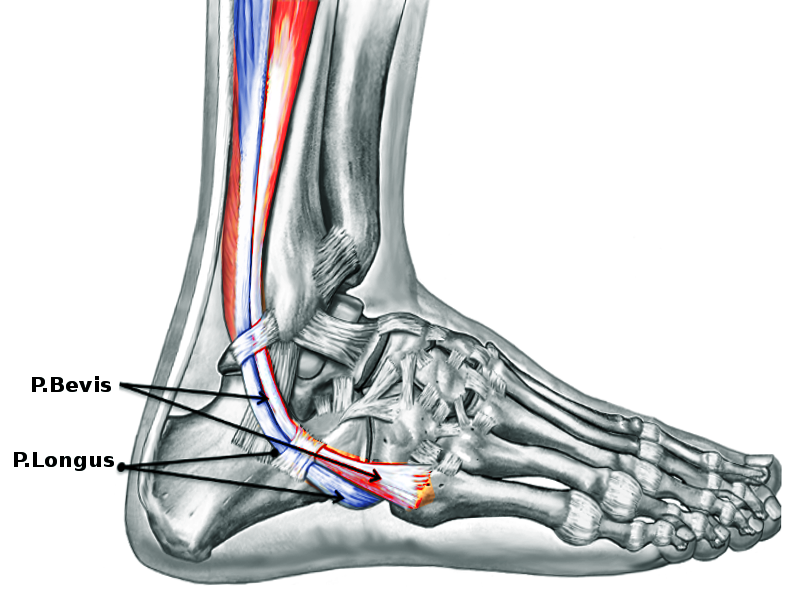
The peroneus longus muscle arises from the head and proximal and lateral side of the fibula and inserts on the base of the first metatarsal and medial cuneiform. Its location is adjacent to the peroneus brevis muscle on the lateral side of the lower limb coursing inferiorly and tapering into a long, slender tendinous portion that descends into the foot posterior to the lateral malleolus before crossing under the foot and attaching to the bones on the medial side of the foot.[4]
The primary function of the peroneus longus muscle is to plantarflex and evert the foot at the ankle. Due to its insertion on the medial aspect of the foot and course down the lateral part of the leg, muscle contraction lifts the foot upward (plantar flexion) and outward (eversion). This movement is critical to the eversion of the foot and can be injured commonly from forced inversion and dorsiflexion of the ankle in the setting of trauma.[4]
Embryology
The limb buds of the embryo start forming about five weeks after fertilization as the mesoderm migrates into the limb bud and forms a posterior condensation and an anterior condensation to eventually create the muscular and skeletal components of the lower limb. The posterior condensation will develop into the extensor and abductor musculature of the lower limb, and the anterior condensation will develop into the flexor and adductor musculature of the lower limb.[5][6][7]
Several factors influence the formation of the limb bud musculature, including retinoic acid, sonic hedgehog (SHH), HOX genes, apical ectodermal ridge (AER), and the zone of polarizing activity (ZPA). Retinoic acid is a global organizing gradient that initiates the production of transcription factors that specify regional differentiation and limb polarization. The apical ectodermal ridge (AER) produces a fibroblast growth factor (Fgf), promoting outgrowth of the limb buds by stimulating mitosis.[5][6][7]
The specific fibroblast growth factor involved in hindlimb development is Fgf10, which is stimulated by Tbx4.[8] The zone of polarizing activity (ZPA) produces SHH, which promotes the organization of the limb bud along the anterior-posterior axis. SHH activates specific HOX genes–Hoxd-9, Hoxd-10, Hoxd-11, Hoxd-12, and Hoxd-13, which are essential in limb polarization and regional specification.[5][6][7] These genes control patterning and, consequently, the morphology of the developing limb in the human embryo.[8] Errors in Hox gene expression can lead to malformations in the limbs.[8]
Blood Supply and Lymphatics
The anterior tibial artery and peroneal artery supply the peroneus longus muscle. The anterior tibial artery arises from the popliteal artery, which originates from the superficial femoral artery, a branch of the common femoral artery of the external iliac artery.[9] As the superficial femoral artery passes through the adductor hiatus into the popliteal fossa, it becomes the popliteal artery. The popliteal artery then divides toward the distal end of the popliteal fossa to give rise to the anterior tibial artery and tibioperoneal trunk. The tibioperoneal trunk then bifurcates into the posterior tibial and peroneal arteries. The posterior tibial artery continues inferiorly to supply the posterior leg muscles, while the peroneal artery descends posteriorly to the fibula within the posterior compartment of the leg. It then divides into perforating branches, which penetrate the intermuscular septum to supply the muscles of the lateral compartment of the leg.[4][5]
The lymphatic vessels of the lower limb can subdivide into two major groups: superficial and deep vessels. The superficial lymph vessels of the lower limb can further split into two groups: a medial group, which follows the greater saphenous vein, and a lateral group, which follows the small saphenous vein.[4][5] There are also deep lymph vessels, including the anterior tibial, posterior tibial, and peroneal vessels, that follow the course of the corresponding blood vessels.[4][5] The lymph vessels of the lower limb drain into the popliteal, superficial inguinal, deep inguinal, external iliac, and lumbar or aortic lymph nodes.[4][5]
Nerves
The peroneus longus muscle receives innervation from the superficial peroneal nerve. The superficial peroneal nerve is one of the terminal branches of the common peroneal nerve, which originates from the sciatic nerve (L4-S3).[10] The sciatic nerve branches at the apex of the popliteal fossa into the tibial and common peroneal nerves. The tibial nerve continues its course down the leg, posterior to the tibia supplying the deep muscles of the posterior leg. It terminates by dividing into two sensory branches, medial and lateral plantar nerves.[5]
The common peroneal artery follows the medial border of the biceps femoris, running in a lateral and inferior direction and continuing over the head of the gastrocnemius.[5] The common peroneal nerve wraps around the neck of the fibula, passing between the attachments of the fibularis longus muscle to supply the lateral compartment of the leg.[5] It then divides and terminates into the superficial peroneal, which will supply the lateral compartment of the leg, and the deep peroneal, which will supply the anterior compartment of the leg, including the extensor hallucis longus.[5] The nerve roots of the superficial peroneal artery are L4-S1. Injury to the superficial peroneal nerve can result in loss of eversion and sensation loss over most of the dorsal foot and anterolateral aspect of the distal leg.[11]
Physiologic Variants
The peroneus longus muscle arises from the head and upper lateral side of the fibula and inserts on the base of the first metatarsal, medial cuneiform. Its tendon passes inferior to the cuboid bone in a bone tunnel termed the cuboid tunnel and inserts onto the plantar surface of the foot on the medial cuneiform. However, several variants exist that may possess one or more accessory tendinous slips that insert into other neighboring bones or tendons. These physiologic variants are clinically important because the peroneus longus muscle is involved in several pathologies, including traumatic injury, tendinitis, dislocation, acute rupture, and chronic tear. Some of these may be more common with certain physiologic variants. A recent study described common physiologic variants in cadaveric specimens.[12]
A table describing the incidence of various bony insertions of the peroneus longus tendon appears below. The description of the most common insertions of the peroneus longus tendon may help physicians better understand the symptoms associated with peroneus longus tendon pathologies and the role played by the tendon in maintaining the arch of the foot.[12]
- The base of 1st metatarsal: 30 specimens, 100%
- Medial cuneiform: 26 specimens, 86.6%
- The neck of the 1st metatarsal: 3 specimens, 10%
- The base of the 2nd metatarsal: 6, 20%
- The base of the 4th metatarsal: 5, 16.6%
- The base of the 5th metatarsal: 7, 23.3%
Surgical Considerations
In trauma and other mechanical injuries, the peroneus longus tendon can become dislocated, subluxated or ruptured. In 2016, a research team queried foot and ankle surgeons nationally to understand their management of acute peroneal tendon tears. There were marked differences in treatment protocols as well as operative techniques. 22% of the surgeons chose nonoperative treatment for greater than one year, while 33% immediately went to operative interventions. For surgeons who decided to operate, 88% tubularized tendons after the repair, 33% excised redundant tissue, and 22% removed the peroneal tubercle if it demonstrated hypertrophy.[13]
Surgical treatment correlates with improved full return to activity and improved patient-reported outcome scores in symptomatic patients.[14] A personalized, comprehensive rehabilitation program is necessary to optimize the recovery of surgically treated peroneal tendon tears and ruptures. Since most peroneal tendon tears occur in young active patients and athletes, early return to activity is of utmost importance.
The lateral compartment of the leg is also susceptible to acute compartment syndrome. When the pressure inside the lateral compartment increases, tissue perfusion can be compromised, potentially leading to irreversible muscle and nerve damage, resulting in muscle and soft tissue necrosis.[5] The most common cause of compartment syndrome involving the lateral compartment is trauma, tight casts or dressing, post-ischemic swelling, and arterial injury.[5] However, it is also possible to develop compartment syndrome chronically and must merit consideration when a patient presents with lateral leg pain, tenderness, and firmness to palpation. Recognition of compartment syndrome is essential to treating and preventing ischemia and necrosis of the neurovascular structures and muscles.[5][15][16][3]
Patients with compartment syndrome will often present with pain out of proportion to the clinical situation. The physical exam findings of compartment syndrome often include pain on palpation of the muscles involved, pain with passive stretching of the muscle (most sensitive test finding before the onset of ischemia), and firmness of the compartment.[5][15][16]
Compartment syndrome primarily affects the venous system. Consequently, arterial pulses are usually intact.[5] The definitive diagnosis of compartment syndrome requires the measurement of compartmental pressures. A resting compartment pressure of greater than 30 mm Hg confirms the diagnosis of compartment syndrome.[5][15][16] In acute compartment syndrome, time is of the essence—if treated within 6 hours of ischemia, complete recovery is anticipated, whereas necrosis occurs after 6 hours of ischemia.[17] Definitive management of acute anterior compartment syndrome is subcutaneous fasciotomy.[5][15][16]
Clinical Significance
The peroneus longus is important in plantar flexion and eversion of the foot at the ankle. For this reason, it is tested during the physical exam to assess the range of motion and motor strength of the ankle. Weakened or absent motor strength can indicate muscle or nerve damage to the peroneus longus and/or peroneus brevis muscles—the two muscles of the lateral compartment of the lower limb.[4]
The peroneus longus muscle can also be involved in tendinitis, subluxation, dislocation, and acute or chronic tendon tears. Most peroneal tendon injuries occur in young, active patients, commonly occurring secondary to sports such as football, soccer, and running. Injury to the peroneus longus tendon is a cause of lateral ankle pain and may lead to ankle instability. Tears are most commonly longitudinal due to subluxation over the fibula but can also be transverse.[18]
An isolated tear is more commonly found in the peroneus brevis muscle but can also occur in the peroneus longus. Non-operative treatment includes NSAIDs, ice, rest, immobilization, and physical therapy. Steroid injections can also be used in patients refractory to previously mentioned treatments. Recent literature has shown a growing interest in PRP injections under ultrasound guidance; however, it is not commonly adopted in practice yet. If conservative treatment fails, operative treatment can include an open debridement, synovectomy, and arthroscopic peroneal tendoscopy for tendinitis. For peroneal tendon tears, operative treatment includes an end-to-end repair, side-to-side anastomosis, or Pulvertaft weave with chronic tears, as well as allograft reconstruction.[19][20]
Lastly, the lateral compartment of the leg can be involved in compartment syndrome. Although the anterior compartment is the most common site for compartment syndrome, lateral compartment syndrome can occur acutely following blunt force injury or trauma or as a chronic, exertional syndrome commonly seen in athletes.[5][15] The muscle groups of the lower limb divide into compartments formed by strong, inflexible fascial membranes. Compartment syndrome occurs when increased pressure within one of these compartments compromises the circulation and function of the tissues within that space.[5][15] The lateral compartment contains muscles that primarily plantar flexes the foot at the ankle and evert the foot. These muscles are innervated and supplied by the superficial peroneal nerve and anterior tibial artery, respectively. Increased pressure in the lateral compartment can cause paresthesias, weakness of muscle action, and pain with passive stretch of the muscles.[5][15] Compartment syndrome constitutes a medical emergency that requires a fasciotomy of the involved compartment.[5]
Media
(Click Image to Enlarge)
References
Khan IA, Mahabadi N, D’Abarno A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Leg Lateral Compartment. StatPearls. 2023 Jan:(): [PubMed PMID: 30137811]
Chandwani D, Varacallo M. Exertional Compartment Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 31335004]
Varacallo M, Shirey L, Kavuri V, Harding S. Acute compartment syndrome of the hand secondary to propofol extravasation. Journal of clinical anesthesia. 2018 Jun:47():1-2. doi: 10.1016/j.jclinane.2018.01.020. Epub 2018 Feb 21 [PubMed PMID: 29476968]
Hallinan JTPD, Wang W, Pathria MN, Smitaman E, Huang BK. The peroneus longus muscle and tendon: a review of its anatomy and pathology. Skeletal radiology. 2019 Sep:48(9):1329-1344. doi: 10.1007/s00256-019-3168-9. Epub 2019 Feb 15 [PubMed PMID: 30770941]
Lezak B, Summers S. Anatomy, Bony Pelvis and Lower Limb: Leg Anterior Compartment. StatPearls. 2023 Jan:(): [PubMed PMID: 30969547]
Mróz I, Kielczewski S, Pawlicki D, Kurzydło W, Bachul P, Konarska M, Bereza T, Walocha K, Kaythampillai LN, Depukat P, Pasternak A, Bonczar T, Chmielewski P, Mizia E, Skrzat J, Mazur M, Warchoł Ł, Tomaszewski K. Blood vessels of the shin - anterior tibial artery - anatomy and embryology - own studies and review of the literature. Folia medica Cracoviensia. 2016:56(1):33-47 [PubMed PMID: 27513837]
Gros J, Tabin CJ. Vertebrate limb bud formation is initiated by localized epithelial-to-mesenchymal transition. Science (New York, N.Y.). 2014 Mar 14:343(6176):1253-6. doi: 10.1126/science.1248228. Epub [PubMed PMID: 24626928]
Level 3 (low-level) evidenceBarham G, Clarke NM. Genetic regulation of embryological limb development with relation to congenital limb deformity in humans. Journal of children's orthopaedics. 2008 Feb:2(1):1-9. doi: 10.1007/s11832-008-0076-2. Epub 2008 Feb 7 [PubMed PMID: 19308596]
Hyland S, Sinkler MA, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Popliteal Region. StatPearls. 2023 Jan:(): [PubMed PMID: 30422486]
Miniato MA, Varacallo M. Anatomy, Back, Lumbosacral Trunk. StatPearls. 2023 Jan:(): [PubMed PMID: 30969700]
Garrett A, Geiger Z. Anatomy, Bony Pelvis and Lower Limb: Superficial Peroneal Nerve (Superficial Fibular Nerve). StatPearls. 2023 Jan:(): [PubMed PMID: 30521214]
Patil V, Frisch NC, Ebraheim NA. Anatomical variations in the insertion of the peroneus (fibularis) longus tendon. Foot & ankle international. 2007 Nov:28(11):1179-82 [PubMed PMID: 18021587]
Brodsky JW, Zide JR, Kane JM. Acute Peroneal Injury. Foot and ankle clinics. 2017 Dec:22(4):833-841. doi: 10.1016/j.fcl.2017.07.013. Epub [PubMed PMID: 29078831]
van Dijk PA, Lubberts B, Verheul C, DiGiovanni CW, Kerkhoffs GM. Rehabilitation after surgical treatment of peroneal tendon tears and ruptures. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2016 Apr:24(4):1165-74. doi: 10.1007/s00167-015-3944-6. Epub 2016 Jan 23 [PubMed PMID: 26803783]
Mabvuure NT, Malahias M, Hindocha S, Khan W, Juma A. Acute compartment syndrome of the limbs: current concepts and management. The open orthopaedics journal. 2012:6():535-43. doi: 10.2174/1874325001206010535. Epub 2012 Nov 30 [PubMed PMID: 23248724]
Taylor RM, Sullivan MP, Mehta S. Acute compartment syndrome: obtaining diagnosis, providing treatment, and minimizing medicolegal risk. Current reviews in musculoskeletal medicine. 2012 Sep:5(3):206-13. doi: 10.1007/s12178-012-9126-y. Epub [PubMed PMID: 22644598]
Kiel J, Kaiser K. Tibial Anterior Compartment Syndrome. StatPearls. 2023 Jan:(): [PubMed PMID: 30085512]
Walt J, Massey P. Peroneal Tendon Syndromes. StatPearls. 2023 Jan:(): [PubMed PMID: 31335074]
Davda K, Malhotra K, O'Donnell P, Singh D, Cullen N. Peroneal tendon disorders. EFORT open reviews. 2017 Jun:2(6):281-292. doi: 10.1302/2058-5241.2.160047. Epub 2017 Jun 22 [PubMed PMID: 28736620]
Philbin TM, Landis GS, Smith B. Peroneal tendon injuries. The Journal of the American Academy of Orthopaedic Surgeons. 2009 May:17(5):306-17 [PubMed PMID: 19411642]