Introduction
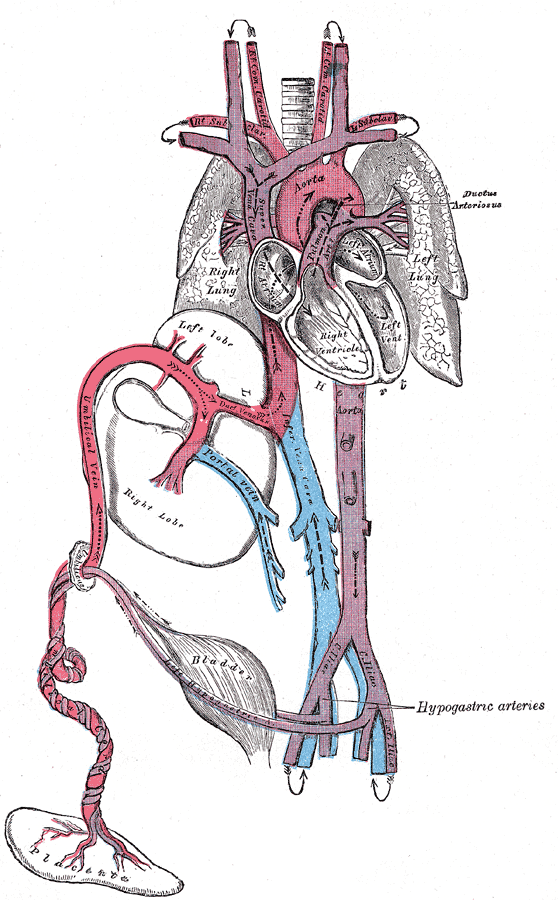
The ductus arteriosus is a fetal vessel that allows the oxygenated blood from the placenta to bypass the lungs in utero. At birth, the lungs fill with air with the first breaths, pulmonary vascular resistance drops, and blood flows from the right ventricle to the lungs for oxygenation. The increased arterial oxygen tension and the decreased flow through the ductus arteriosus allow the ductus to constrict. The ductus arteriosus is functionally closed by 12 to 24 hours of age in healthy, full-term newborns. Permanent (anatomic) closure is complete within 2 to 3 weeks.
In premature infants, the ductus arteriosus does not close rapidly and may require pharmacologic or surgical closure to treat side effects.[1][2][3]
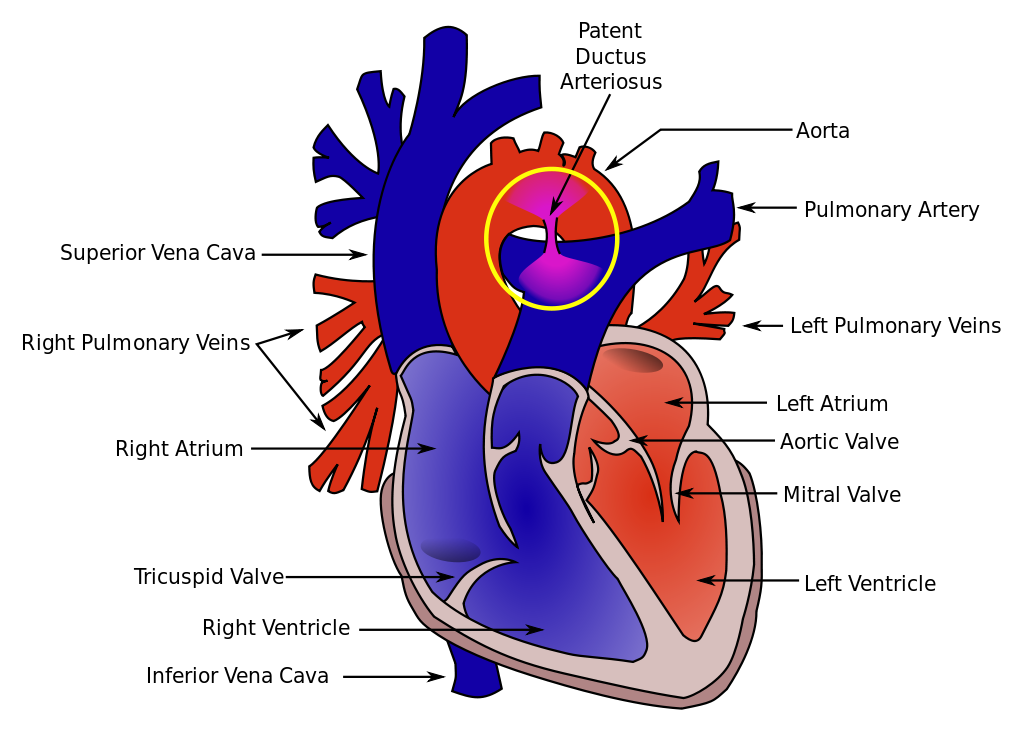
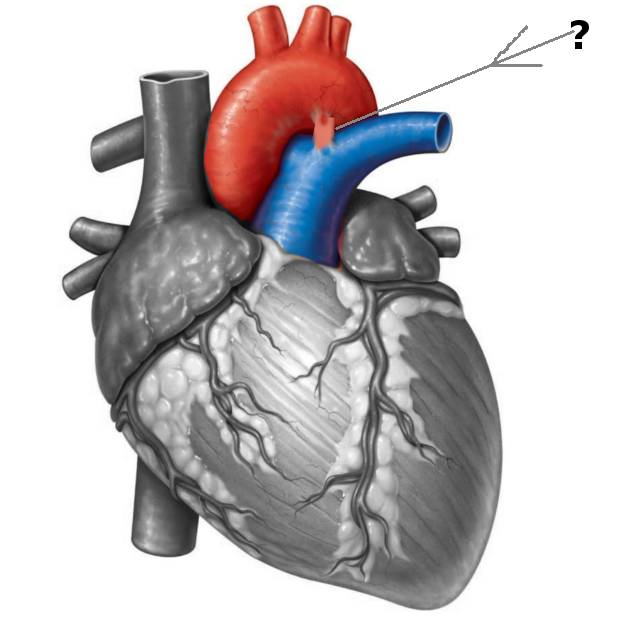
Anatomy
During fetal life, the ductus is a normal structure that permits blood leaving the right ventricle to bypass the pulmonary circulation and enter the descending aorta. Less than 10% of this blood enters the pulmonary circulation. After birth, the ductus closes within 24-48 hours. The ductus is a remnant of the distal sixth aortic arch and connects the proximal descending aorta to the main pulmonary artery. The ductus can be found just posterior to the arch of the aorta, where it enters the anterior pulmonary artery. The ductus has a conical shape, which is large at the aortic end and narrow at the pulmonary end. However, the shape, size, and length of the ductus are very variable.
For surgeons, an anatomical marker of the patent ductus is the recurrent laryngeal nerve, which loops posteriorly around the ductus and ascends behind the aorta en route to the larynx. The recurrent laryngeal nerve is often injured during surgical ligature of the ductus.
The Patent ductus is classified based on its angiographic features and includes the following:
- Type A: Conical
- Type B: Window
- Type C: Tubular
- Type D: Complex
- Type E: Elongated
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
During fetal life, the oxygen tension is low, and the pulmonary vascular system is not functioning. Coupled with circulating levels of prostaglandins from the placenta, this keeps the ductus patent. At birth, the placenta is removed and thus the source of prostaglandins is also diminished, this allows blood to flow into the lungs where the remaining prostaglandins are broken down. In addition, with birth, as the infant takes its first breaths, the oxygen tension increases, which also drops the pulmonary vascular resistance.
In most healthy newborns, the ductus will close within 12-24 hours of life. This occurs by contraction of the muscles of the ductus, which are sensitive to oxygen, acetylcholine, bradykinin, and endothelin. While the functional closure occurs within hours of birth, the anatomic closure may take several weeks. During the second stage, the ductus becomes fibrous and thus, there is no blood flow through it. Most infants have closure of the ductus within 2-3 weeks, and if the ductus remains patent after 8 weeks, it should be closed. Spontaneous closure of the ductus is very rare.
A patent ductus arteriosus (PDA) is rare in healthy term newborns. As gestational age decreases, the incidence of PDA increases. In extremely premature infants, especially those with respiratory distress syndrome, up to 80% may have a PDA at 3 days of age. Some genetic conditions are associated with PDA: Trisomy 13, 18, 21; Holt-Oram, Noonan, CHARGE, TAAD/PDA, DiGeorge, and familial PDA, many forms of congenital heart disease. Maternal conditions and exposures associated with PDA include maternal diabetes, magnesium exposure, cocaine, and calcium channel blockers. Neonatal conditions and exposures associated with PDA include extreme prematurity, respiratory distress syndrome, neonatal sepsis, birth at high altitude, excess fluid administration, loop diuretics, aminoglycosides, cimetidine, and heparin. [4][5]
Epidemiology
The ductus arteriosus will close in virtually all healthy term newborns by 72 hours of age. The incidence of PDA in premature infants is inversely proportional to gestational age. In infants who are > 30 weeks gestation at birth, 90% will have a closed ductus at day 4, and 98% will be closed by the time of discharge. Infants born weighing less than 1000 grams are at the highest risk for PDA. In this population, 70% will have a PDA on day 7.[6]
In at least 10% of other congenital heart disorders, a patent ductus may be present.
Pathophysiology
The patency of the ductus is promoted by prostaglandin E2. If the ductus remains patent after birth, it is associated with pulmonary edema and pulmonary hemorrhage, necrotizing enterocolitis, intraventricular hemorrhage, congestive heart failure, renal failure, and bronchopulmonary dysplasia (BPD). A PDA can result in blood flowing from the descending aorta across the patent ductus arteriosus into the pulmonary circulation ("left-to-right"). This results in pulmonary edema. The "steal" from the aorta during diastole requires increased cardiac output to compensate. Extremely premature infants have limited ability to increase stroke volume and thus use increased heart rate to increase cardiac output. Decreased blood flow to the lower body results in an increased risk for necrotizing enterocolitis and renal failure. [7][8][9]
The magnitude of the left-to-right shunt depends on many factors, but the most important is the ratio of the pulmonary vascular resistance (PVR) to the systemic vascular resistance (SVR). If the PVR is low and the SVR is high, the flow through the shunt to the lungs will be high. This will also result in more blood returning to the left atrium and left ventricle, which later results in left atrial and left ventricular hypertrophy.
History and Physical
The classic PDA murmur is a continuous, “machinery” murmur below the clavicle, radiating to the back, although it can also manifest as a systolic or holosystolic murmur. The infant will have a prominent precordial impulse, tachycardia, and bounding peripheral pulses due to increased cardiac output. Hypotension is most prominent in infants < 1000g grams. A widened pulse pressure (> 30mmHg) occurs both because of a mild increase in systolic blood pressure to overcome the decrease in distal blood flow due to run-off through the PDA during diastole, in addition to lower diastolic blood pressure from the run-off. The increase in respiratory distress and hypoxia occurs with pulmonary edema. Hepatomegaly can be appreciated when there is congestive heart failure.
Evaluation
Chest radiography may show increased pulmonary vascular markings and pulmonary edema. Echocardiography shows a patent ductus arteriosus. Left-to-right flow is indicative of a typical PDA. Right-to-left flow across the PDA indicates pulmonary hypertension, for which the PDA may be a secondary finding. A hemodynamically significant PDA manifests on echo with increased left atrial and left ventricular enlargement. Reversal of diastolic flow in the abdominal aorta at the level of the diaphragm may be seen but is technically challenging, so the absence of a reversal of diastolic flow on echo does not mean it is clinically absent. Increased serum creatinine and decreased urine output indicate the level of renal impairment. [10][11][12]
Treatment / Management
In gestationally more mature infants, conservative management of a PDA may be sufficient to support the infant while awaiting spontaneous closure. Conservative management includes careful fluid restriction (110 to 130ml/kg/d while monitoring urine output) and increasing peak end-expiratory pressure (PEEP) to treat pulmonary edema. Diuretics are controversial due to the lack of evidence that they improve outcomes in very premature infants, may prevent PDA closure, and cause electrolyte derangements, which can be difficult to manage in extremely premature infants. [13][14][15](A1)
Pharmacologic treatment with indomethacin, ibuprofen, or acetaminophen/paracetamol should be considered for preterm infants with a symptomatic PDA. Infants who are born weighing greater than 1000 grams are unlikely to require pharmacologic therapy to close the ductus. Although the ductus in a preterm infant > 1000g at birth does not close as quickly as in a healthy term infant (median time for closure is 7 days in infants >1000 g), the vast majority close spontaneously prior to hospital discharge and do not require medication.
For those infants who are symptomatic despite conservative management (increasing PEEP and restricting fluid), there are three choices for pharmacologic treatment: indomethacin, ibuprofen, and acetaminophen/paracetamol. Indomethacin typically is given in 3 doses, 12 hours apart. A fourth dose can be given 24 hours after the third to ensure closure. Ibuprofen typically is given in 3 doses, 24 hours apart. Indomethacin and ibuprofen have a fairly equivalent efficacy (around 66% to 70%). In resistant cases, a second course of medication may be considered, but cumulative effects on renal function should be evaluated before embarking on a second course. The side effects of indomethacin and ibuprofen are similar, but indomethacin has been associated with more concerns for gut perfusion and necrotizing enterocolitis. However, in a large multicenter randomized controlled trial, there was no increase in necrotizing enterocolitis in infants fed small (15 ml/kg/d) amounts of milk during treatment with indomethacin when compared with infants who were fasted.
Acetaminophen/paracetamol shows promise for treating a patent ductus arteriosus. Multiple small studies show close equivalence between indomethacin and ibuprofen, although it may be less effective in infants previously treated with indomethacin or ibuprofen or in the smallest infants. It is administered intravenously at 15 mg/kg/dose every 6 hours for 3 to 8 days. Most studies were 3 days, continuing to 6 days if closure was not achieved. Liver enzymes should be monitored for toxicity.
If the PDA is hemodynamically significant despite pharmacologic therapy and results in increased respiratory support or renal impairment, or if there are contraindications to the use of pharmacologic therapy, surgical ligation can be performed.
Differential Diagnosis
- Coronary artery fistula
- Sinus of Valsalva aneurysm
- Aortopulmonary defect
- Persistent truncus arteriosus
- Pulmonary arteriovenous fistula
- Total anomalous pulmonary venous return
Prognosis
For infants with just an isolated PDA, the prognosis is good. In premature infants, the prognosis is dependent on other comorbidities. After the closure of the PDA, most children have a normal life expectancy. Spontaneous closure of the PDA is rare. With the use of indomethacin, close to 80-90% of infants will have successful closure of the PDA. In adults, surgical closure is always required, provided the patient has not developed fixed pulmonary hypertension.
The morbidity and mortality are linked to the volume of blood flow via the PDA. If left untreated, pulmonary hypertension can develop, which will lead to premature death. Premature infants with PDA may develop respiratory distress syndrome. Surgical complications of the PDA include injury to the recurrent laryngeal nerve, occlusion of the descending aorta, injury to the pulmonary artery and phrenic nerve, and death.
Complications
- Eisenmenger phenomenon
- Closure of the aorta during surgery
- Recurrent laryngeal nerve injury
- Necrotizing enterocolitis
- Pulmonary hypertension
- Right heart failure
Postoperative and Rehabilitation Care
Endocarditis prophylaxis is required for the first 6 months after closure.
Consultations
- Cardiac surgeon
- Interventional radiology
- Cardiologist
- Pediatrician
Enhancing Healthcare Team Outcomes
PDA is not an uncommon finding in neonates. The majority of patients with a PDA are young children, and the care of this congenital anomaly has changed over the years. Since most infants are managed in the NICU, a healthcare team is usually involved in the care. A pediatrician, intensivist, cardiac surgeon, and interventional radiologist are usually consulted on the best treatment approach. Initially, premature infants are managed with ibuprofen, and if that fails, surgery is an option. Today, endovascular procedures are also available to close the ductus. However, the care of an infant with a PDA is always done by a nurse. These patients need close monitoring because they often have other comorbidities. The pharmacist should be fully aware of the dose of ibuprofen and other drug options available to close the ductus. Only through a systemic approach to congenital heart disorders can the morbidity and mortality be lowered. [16][17][18] (Level 5)
Outcomes
The outcome for the majority of patients in whom the PDA is ligated or medically treated is good. However, in most of these infants, it is the presence of other disorders that dictate the prognosis. Spontaneous closure of the ductus is very rare after the first three months of birth. Further, even in infants treated medically with ibuprofen, sometimes the ductus may reopen and require surgical closure. In all adults, the presence of a ductus requires surgical closure. In fact, before the ductus is closed in the adult population, the status of the pulmonary vasculature must be determined. Thus, patients with mild pulmonary hypertension have a normal life expectancy. The surgical mortality for ductus varies from 2-20% depending on the infant's age and other co-existing comorbidities. If left untreated, the mortality rate increases with age. [19][20][21](Level 5)
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Fink D, Nitzan I, Bin-Nun A, Mimouni F, Hammerman C. Ductus arteriosus outcome with focus on the initially patent but hemodynamically insignificant ductus in preterm neonates. Journal of perinatology : official journal of the California Perinatal Association. 2018 Nov:38(11):1526-1531. doi: 10.1038/s41372-018-0204-x. Epub 2018 Aug 17 [PubMed PMID: 30120422]
Clyman RI. Patent ductus arteriosus, its treatments, and the risks of pulmonary morbidity. Seminars in perinatology. 2018 Jun:42(4):235-242. doi: 10.1053/j.semperi.2018.05.006. Epub 2018 May 10 [PubMed PMID: 29958703]
Jasani B, Weisz DE, McNamara PJ. Evidence-based use of acetaminophen for hemodynamically significant ductus arteriosus in preterm infants. Seminars in perinatology. 2018 Jun:42(4):243-252. doi: 10.1053/j.semperi.2018.05.007. Epub 2018 May 24 [PubMed PMID: 29958702]
Hung YC, Yeh JL, Hsu JH. Molecular Mechanisms for Regulating Postnatal Ductus Arteriosus Closure. International journal of molecular sciences. 2018 Jun 25:19(7):. doi: 10.3390/ijms19071861. Epub 2018 Jun 25 [PubMed PMID: 29941785]
Reese J, Scott TA, Patrick SW. Changing patterns of patent ductus arteriosus surgical ligation in the United States. Seminars in perinatology. 2018 Jun:42(4):253-261. doi: 10.1053/j.semperi.2018.05.008. Epub 2018 May 22 [PubMed PMID: 29954594]
Iwashima S, Satake E, Uchiyama H, Seki K, Ishikawa T. Closure time of ductus arteriosus after birth based on survival analysis. Early human development. 2018 Jun:121():37-43. doi: 10.1016/j.earlhumdev.2018.05.003. Epub 2018 May 10 [PubMed PMID: 29754023]
P S, Jose J, George OK. Contemporary outcomes of percutaneous closure of patent ductus arteriosus in adolescents and adults. Indian heart journal. 2018 Mar-Apr:70(2):308-315. doi: 10.1016/j.ihj.2017.08.001. Epub 2017 Aug 9 [PubMed PMID: 29716712]
Weisz DE, Giesinger RE. Surgical management of a patent ductus arteriosus: Is this still an option? Seminars in fetal & neonatal medicine. 2018 Aug:23(4):255-266. doi: 10.1016/j.siny.2018.03.003. Epub 2018 Mar 7 [PubMed PMID: 29636280]
de Boode WP, Kluckow M, McNamara PJ, Gupta S. Role of neonatologist-performed echocardiography in the assessment and management of patent ductus arteriosus physiology in the newborn. Seminars in fetal & neonatal medicine. 2018 Aug:23(4):292-297. doi: 10.1016/j.siny.2018.03.007. Epub 2018 Mar 7 [PubMed PMID: 29551482]
de Freitas Martins F, Ibarra Rios D, F Resende MH, Javed H, Weisz D, Jain A, de Andrade Lopes JM, McNamara PJ. Relationship of Patent Ductus Arteriosus Size to Echocardiographic Markers of Shunt Volume. The Journal of pediatrics. 2018 Nov:202():50-55.e3. doi: 10.1016/j.jpeds.2018.06.045. Epub 2018 Aug 13 [PubMed PMID: 30115452]
van Laere D, van Overmeire B, Gupta S, El-Khuffash A, Savoia M, McNamara PJ, Schwarz CE, de Boode WP, European Special Interest Group ‘Neonatologist Performed Echocardiography’ (NPE). Application of NPE in the assessment of a patent ductus arteriosus. Pediatric research. 2018 Jul:84(Suppl 1):46-56. doi: 10.1038/s41390-018-0077-x. Epub [PubMed PMID: 30072803]
Singh Y, Katheria A, Tissot C. Functional Echocardiography in the Neonatal Intensive Care Unit. Indian pediatrics. 2018 May 15:55(5):417-424 [PubMed PMID: 29845957]
Henry BM, Hsieh WC, Sanna B, Vikse J, Taterra D, Tomaszewski KA. Incidence, Risk Factors, and Comorbidities of Vocal Cord Paralysis After Surgical Closure of a Patent Ductus Arteriosus: A Meta-analysis. Pediatric cardiology. 2019 Jan:40(1):116-125. doi: 10.1007/s00246-018-1967-8. Epub 2018 Aug 24 [PubMed PMID: 30167748]
Level 1 (high-level) evidenceHalil H, Buyuktiryaki M, Atay FY, Oncel MY, Uras N. Reopening of the ductus arteriosus in preterm infants; Clinical aspects and subsequent consequences. Journal of neonatal-perinatal medicine. 2018:11(3):273-279. doi: 10.3233/NPM-17136. Epub [PubMed PMID: 30149471]
Hundscheid T, Onland W, van Overmeire B, Dijk P, van Kaam AHLC, Dijkman KP, Kooi EMW, Villamor E, Kroon AA, Visser R, Vijlbrief DC, de Tollenaer SM, Cools F, van Laere D, Johansson AB, Hocq C, Zecic A, Adang E, Donders R, de Vries W, van Heijst AFJ, de Boode WP. Early treatment versus expectative management of patent ductus arteriosus in preterm infants: a multicentre, randomised, non-inferiority trial in Europe (BeNeDuctus trial). BMC pediatrics. 2018 Aug 4:18(1):262. doi: 10.1186/s12887-018-1215-7. Epub 2018 Aug 4 [PubMed PMID: 30077184]
Level 1 (high-level) evidenceCorcoran S, Briggs K, O' Connor H, Mullers S, Monteith C, Donnelly J, Dicker P, Franklin O, Malone FD, Breathnach FM. Prenatal detection of major congenital heart disease - optimising resources to improve outcomes. European journal of obstetrics, gynecology, and reproductive biology. 2016 Aug:203():260-3. doi: 10.1016/j.ejogrb.2016.06.008. Epub 2016 Jun 18 [PubMed PMID: 27359082]
Luca AC, Holoc AS, Iordache C. CONGENITAL HEART MALFORMATIONS IN NEWBORN BABIES WITH LOW BIRTH WEIGHT. Revista medico-chirurgicala a Societatii de Medici si Naturalisti din Iasi. 2015 Apr-Jun:119(2):353-60 [PubMed PMID: 26204636]
Whitfield K, Barkeij C, North A. MEDICATION MANAGEMENT OF THE EXTREMELY PREMATURE NEONATE - THE IMPACT OF A SPECIALIST PHARMACIST. Archives of disease in childhood. 2016 Sep:101(9):e2. doi: 10.1136/archdischild-2016-311535.55. Epub [PubMed PMID: 27540237]
Aygün A, Poryo M, Wagenpfeil G, Wissing A, Ebrahimi-Fakhari D, Zemlin M, Gortner L, Meyer S. Birth weight, Apgar scores and gentamicin were associated with acute kidney injuries in VLBW neonates requiring treatment for patent ductus arteriosus. Acta paediatrica (Oslo, Norway : 1992). 2019 Apr:108(4):645-653. doi: 10.1111/apa.14563. Epub 2018 Oct 1 [PubMed PMID: 30178614]
Liu J, Gao L, Tan HL, Zheng QH, Liu L, Wang Z. Transcatheter closure through single venous approach for young children with patent ductus arteriosus: A retrospective study of 686 cases. Medicine. 2018 Aug:97(35):e11958. doi: 10.1097/MD.0000000000011958. Epub [PubMed PMID: 30170394]
Level 2 (mid-level) evidenceMashally S, Nield LE, McNamara PJ, Martins FF, El-Khuffash A, Jain A, Weisz DE. Late oral acetaminophen versus immediate surgical ligation in preterm infants with persistent large patent ductus arteriosus. The Journal of thoracic and cardiovascular surgery. 2018 Nov:156(5):1937-1944. doi: 10.1016/j.jtcvs.2018.05.098. Epub 2018 Jul 11 [PubMed PMID: 30007780]