Introduction
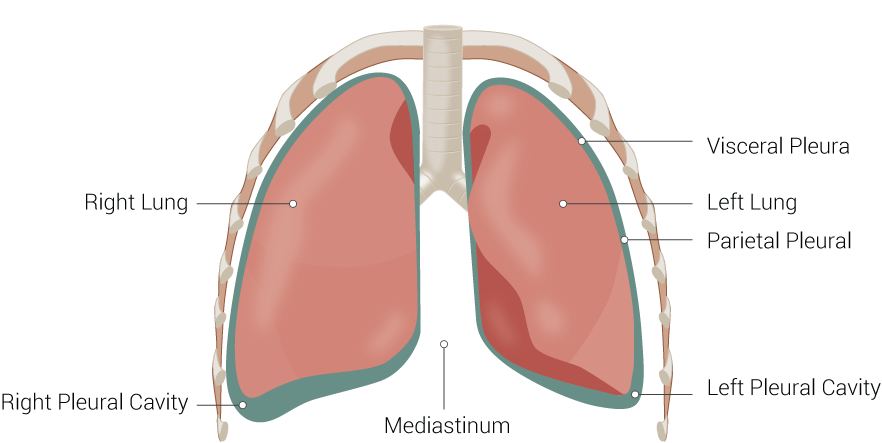
The thoracic mediastinum is the compartment that runs the length of the thoracic cavity between the pleural sacs of the lungs. This compartment extends longitudinally from the thoracic inlet to the superior surface of the diaphragm. Although there are no physical barriers between compartments other than the pericardium, the mediastinum is typically discussed based on subdivisions. The four-compartment model divides the mediastinum into the superior, anterior, middle, and posterior portions. The mediastinum houses many vital structures including the heart, great vessels, trachea, and essential nerves. It also functions as a protected pathway for structures traversing from the neck, superiorly, and into the abdomen, inferiorly. The mediastinum is also clinically significant due to the variety of physical anomalies and pathologies that can occur in this region.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
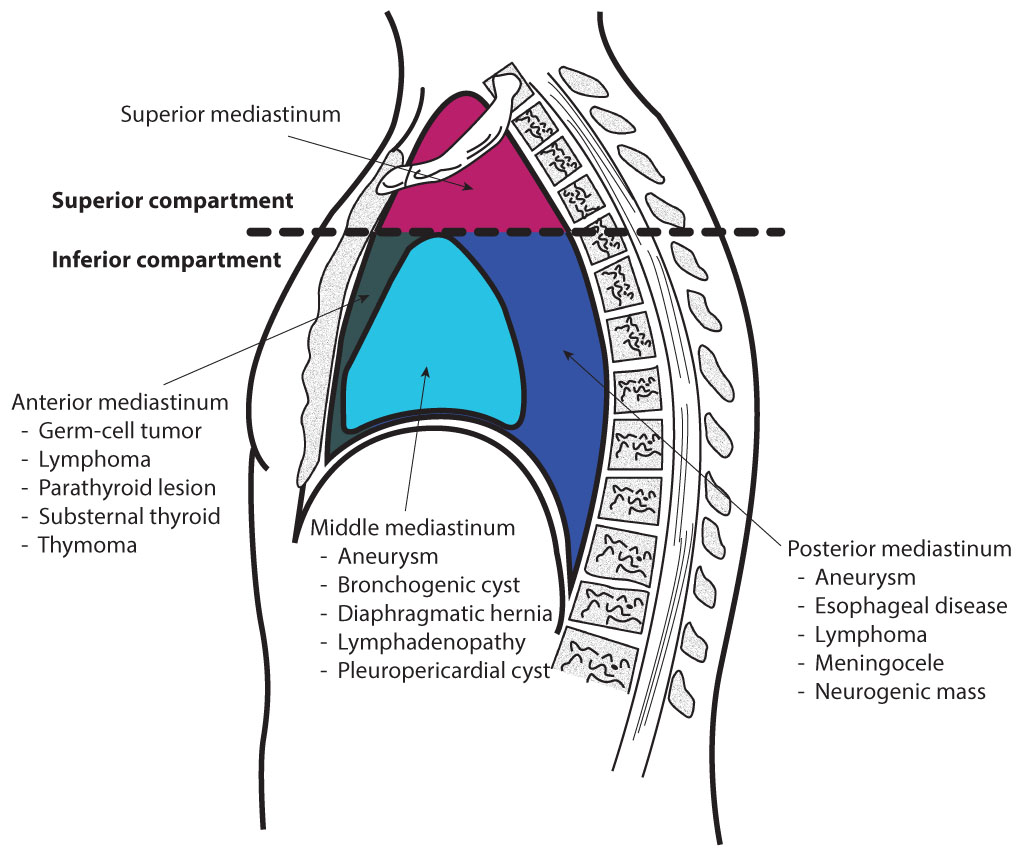
The mediastinum is divided compartmentally and consists of subdivisions that house and support vital structures within the thorax. Below are the borders of each region of the mediastinum.
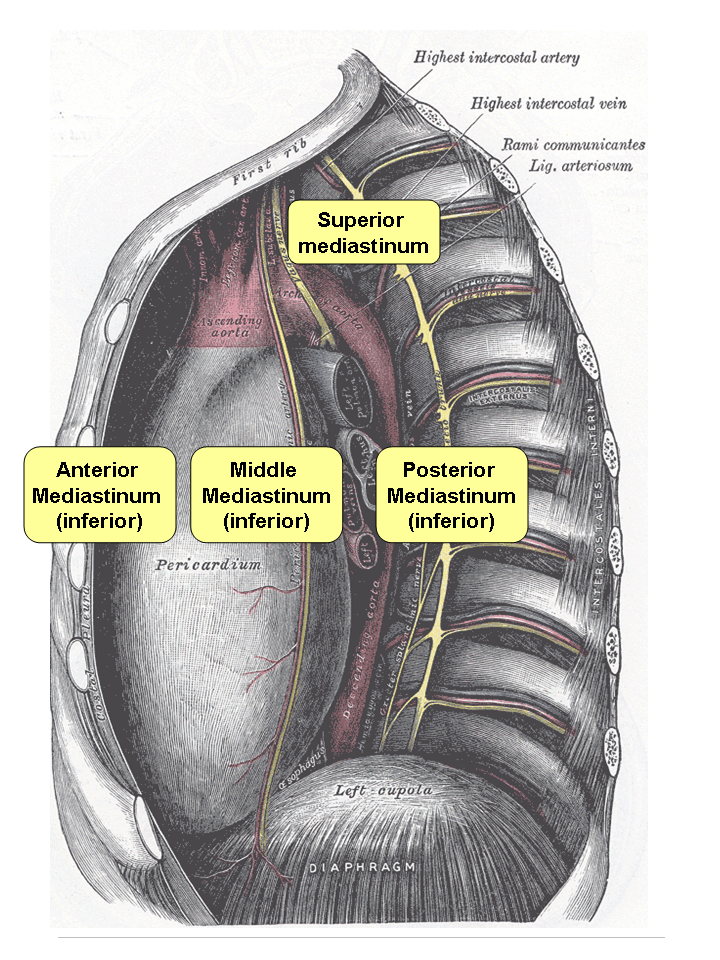
- Superior Mediastinum: bordered by the thoracic outlet superiorly, transverse thoracic plane (the plane of Ludwig) or sternal angle inferiorly, medial border of the pleural sacs laterally, dorsal surface of the sternum anteriorly, and ventral surface of the first four thoracic vertebral bodies posteriorly[1][2][3]
- Anterior Mediastinum: bordered by the pericardium posteriorly, medial border of the pleural sacs laterally, and the sternum, transversus thoracis muscles, and fifth, sixth, and seventh left costal cartilages anteriorly[1][2][4][5]
- Middle Mediastinum: formed by the borders of the pericardial sac anteriorly and posteriorly, reflected to the medial borders of the pleural sacs bilaterally, transverse thoracic plane superiorly, and thoracic surface of the diaphragm inferiorly[1][2][5][6][7]
- Posterior Mediastinum: bordered by the pericardium anteriorly, the thoracic surface of the diaphragm inferiorly, the transverse thoracic plane superiorly, the bodies of the fifth to the twelfth thoracic vertebrae posteriorly, and the pleural sacs laterally[1][2][5]
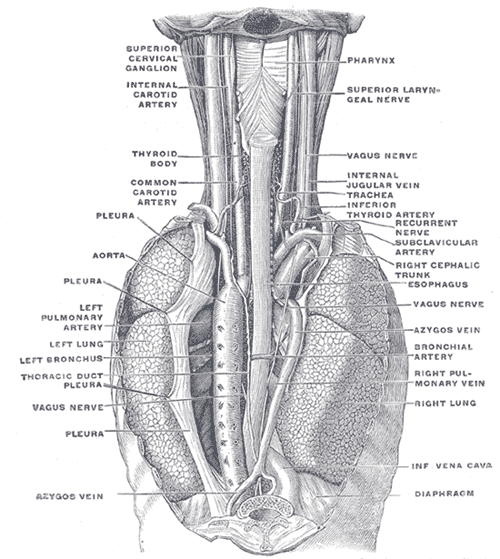
Each region of the thoracic mediastinum contains unique structures. Listed below are the different regions of the thoracic mediastinum and a high-level overview of their components.
- Superior Mediastinum:
- Organs: thymus, trachea, esophagus
- Arteries: aortic arch, brachiocephalic trunk, left common carotid artery, left subclavian artery
- Veins and lymphatics: superior vena cava, brachiocephalic veins, the arch of the azygos, thoracic duct
- Nerves: left and right vagus, recurrent laryngeal, cardiac, left and right phrenic nerves[1][2][8][3]
- Anterior Mediastinum:
- Organs: thymus
- Arteries: internal thoracic branches
- Veins and lymphatics: internal thoracic branches, parasternal lymph nodes
- Nerves: none[1][2][8][4][5]
- Middle Mediastinum:
- Organs: the heart and its great vessel roots, trachea and main bronchi
- Arteries: ascending aorta, pulmonary trunk, pericardiacophrenic arteries
- Veins and lymphatics: superior vena cava, pulmonary veins, pericardiacophrenic veins
- Nerves: phrenic, vagus, sympathetics[1][2][8][9][5][6][7]
- Posterior Mediastinum:
Each region of the mediastinum can be considered to serve a primary function.
The superior mediastinum is essentially a conduit space allowing structures to pass between the head, neck, and thorax.[1][2][3] The anterior mediastinum is protective in nature and filled with connective and fatty tissue that cushions and supports the thymus as well as the vital cardiac structures just posterior to it.[2][5] The middle mediastinum houses the heart and the roots of the great vessels.[2][5][6][7] The posterior mediastinum, which can be thought of as a continuation of the superior mediastinum, also serves as a conduit. It provides space for the passage of structures between the thoracic and abdominal cavities.[2][5]
Blood Supply and Lymphatics
The thoracic mediastinum houses the heart and the great vessels. Due to this anatomical configuration, the thoracic mediastinum has many blood vessels traveling through it.[1][2][5][6][7] Since the lymphatic system closely integrates into the cardiovascular system, there is also a significant presence of lymphatics in this area.[1][2][5][10]
The superior mediastinum contains the arch of the aorta and its three associated major branches: the brachiocephalic trunk, the left common carotid, and the left subclavian arteries.[1][2][5] In addition to these large arteries, some smaller branches of the aorta are present within the superior mediastinum including the thymic branches of the internal thoracic arteries, the proximal portions of the pericardiophrenic arteries, and the third and fourth posterior intercostal arteries.[11][9][3] The majority of lymphatic drainage in this region coalesces at the thoracic duct, which empties into the bloodstream at the left subclavian vein.[1][4][5][10]
The internal thoracic arteries descend inferiorly and deep to the lateral borders of the sternum. These arteries exit the anterior thoracic mediastinum inferiorly and branch into the musculophrenic arteries and superior epigastric arteries.[11] Lymphatics in this region include the parasternal, pericardial and superior diaphragmatic lymph nodes.[12][5][6][10]
The middle thoracic mediastinum, bounded by the pericardium, contains the coronary arteries and its associated branches. The lymphatics within the pericardium are a complex network of vessels that penetrate all layers of the cardiac tissue. These vessels ultimately drain posteriorly towards the pre-tracheal lymph nodes that lie between the aorta and the trachea.[12][6][10]
The posterior thoracic mediastinum contains the descending aorta as it courses slightly left of midline down towards the diaphragm. The most notable arterial branches in this region are the proximal portions of the intercostal arteries. The lymphatics of this region include the thoracic duct, retrocardiac lymph nodes, diaphragmatic lymph nodes, posterior mediastinal lymph nodes, and prevertebral lymph nodes.[1][2][5][10]
Nerves
In the superior mediastinum, there are two broad categories of nerves passing within the region, nerves that originate superior to the thorax and nerves that originate within the thorax.
The superior thoracic mediastinum contains the left and right phrenic nerves (C3 - C5), the left and right vagus nerves, and other associated vagal branches including the esophageal plexus, the inferior cervical cardiac branches, the thoracic cardiac branches, and the recurrent laryngeal nerves. As for the nerves originating from within the thorax, there is the superior portion of the sympathetic trunk (T1 through T4) and its associated sympathetic branches such as the thoracic cardiac and pulmonary branches.[8][13]
The anterior mediastinum does not contain any major named nerves.[2][8][5][8]
The middle mediastinum is densely innervated by the autonomic nervous system and somatically innervated by the phrenic nerves. The sympathetic innervation arises from branches of the sympathetic trunk around the T2 through T4 levels while parasympathetic innervation derives from branches of the left and right vagus nerves. Branches of the left and right phrenic nerves provide somatic innervation to the fibrous and parietal pericardial layers.[14][1][2][8][9][6][13] Because the boundaries of the middle mediastinum are the borders of the pericardium itself, only a small portion of the nerves mentioned truly reside within the middle mediastinum.
The posterior mediastinum contains many autonomic and somatic nerves. Sympathetic nerves arise from the sympathetic chain at the T5 to T12 levels and parasympathetic innervation is provided by the left and right vagus nerves which form of the esophageal plexus. The somatic nerves in the posterior mediastinum are the intercostal nerves.[1][2][8][5]
Muscles
Although often overlooked, there are many critical muscular structures within the thoracic mediastinum. For example, the superior thoracic mediastinum contains the skeletal and smooth muscle of the esophagus and the left and right inferior oblique portion of longus colli muscle which assists in mobilizing the cervical spine.[1][3][15] The anterior thoracic mediastinum contains the transversus thoracis muscles, an accessory muscle of expiration. The transversus thoracis muscles originate on the posterolateral area of the sternum and aid in depressing the ribs during active expiration.[16] The middle thoracic mediastinum houses one of the most important muscles of the body, the heart. The posterior thoracic mediastinum contains the distal smooth muscular portion of the esophagus. Many of the large blood vessels in the mediastinum comprise numerous layers of smooth muscle that allow for cardiovascular homeostasis.[1][2][8][6]
Physiologic Variants
Regularly, there is a minimal level of variation in the compartmentalization and organization of the thoracic mediastinum between individuals. The structures held within the thoracic mediastinal compartments are highly subject to variability, though. Below are some physiologic variants that can affect and/or be seen in structures within the thoracic mediastinal compartments.
Superior Mediastinum[17][1][5]:
- Absent brachiocephalic trunk (right common carotid and subclavian arteries branch directly from aortic arch)
- Patent ductus arteriosus
- Tracheoesophageal fistula
Anterior Mediastinum[1]:
- Pectus excavatum
- Thymic aplasia
- Thymic cyst
- Dextrocardia
- Heart side dominance (based on which coronary artery gives rise to the posterior interventricular branch)
- Patent foramen ovale
- Tetralogy of Fallot
- Ventricular septal defects
- Bronchogenic cysts
- Esophageal atresia
- Esophageal stenosis
Clinical Significance
The thoracic mediastinum is a significant region of the human body that includes vital cardiopulmonary structures. The mediastinum is involved in a variety of clinical abnormalities at all ages. Below is an abbreviated list of clinical correlations organized by subdivision.
The superior thoracic mediastinum is clinically relevant due to its large vessels and nerves. Penetrating wounds to this area have a high likelihood of affecting important vessels or nerves resulting in critical damage on impact, as well as during extraction.[19] The arch of the aorta, the site of a potential aneurysm, runs through the center of the superior thoracic mediastinum. It carries the entirety of the cardiac output before its distribution throughout the body. An aneurysm in the arch of the aorta is dangerous and if untreated for long enough can dissect and result in near-instant death.[20] The superior thoracic mediastinum also houses parts of the esophagus and trachea, which are both conduits that commonly are obstructed and injured by ingestion and inhalation of foreign substances.[21][22]
The anterior mediastinum may appear clinically benign, but it is responsible for many clinical considerations. The thymus, located in the superior portion of the anterior mediastinum, is notorious for its role in diseases such as myasthenia gravis, pure red cell aplasia, and thymus cancer.[14][23] Additionally, the anterior mediastinum is located directly posterior to the sternum and is therefore vulnerable to trauma to the anterior thorax which can result in an intrathoracic or thymic hematoma.[24]
The middle mediastinum is arguably the most important subdivision of the region as it contains the pericardium, heart, and great vessel roots. Myocardial infarction, pericardial effusion, cardiac tamponade, Tetralogy of Fallot, and cardiomegaly are just a few examples of pathologies that manifest in the middle thoracic mediastinum.[18][25][26]
The posterior mediastinum piggybacks a large amount of its clinical importance from the structures descending from the superior thoracic mediastinum. The descending aorta, autonomic nervous networks, extensive lymphatics, and esophagus are all capable of causing vast systemic dysfunction in the presence of pathology. Descending thoracic aortic aneurysm, thoracic duct obstruction, and distal esophageal-related dysphagia are problems that can quickly evolve into life-threatening situations.[20][21][27]
These examples are just a few of the many pathologies involved in the thoracic mediastinum. These compartments and their structures are often involved in diseases from acute to chronic, infectious to traumatic, and congenital to neoplastic. Therefore, understanding the distinct regions of the thoracic mediastinum, the contained structures, landmarks, and physiologic variants, is essential to clinicians at all levels.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
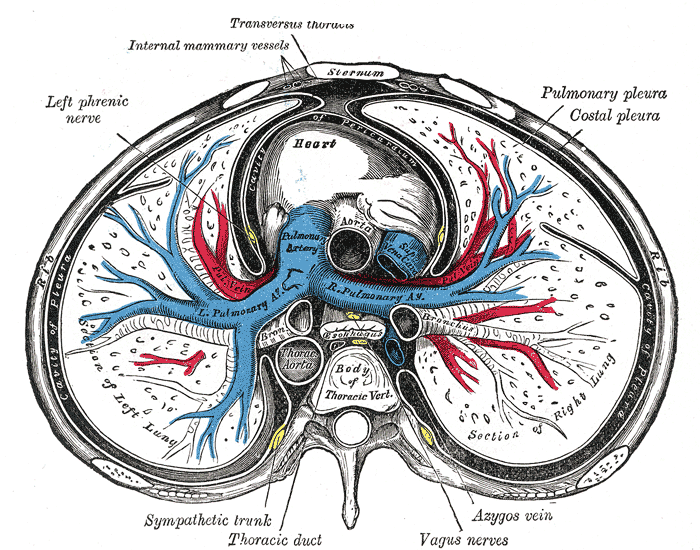
The Mediastinum, Transverse Section of the Thorax. The Mediastinum, a transverse section of the thorax, showing the contents of the middle and the posterior mediastinum, left phrenic nerve, heart, lungs, pulmonary pleura, and costal pleura.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Bardo DME, Biyyam DR, Patel MC, Wong K, van Tassel D, Robison RK. Magnetic resonance imaging of the pediatric mediastinum. Pediatric radiology. 2018 Aug:48(9):1209-1222. doi: 10.1007/s00247-018-4112-1. Epub 2018 Aug 4 [PubMed PMID: 30078043]
Ugalde PA, Pereira ST, Araujo C, Irion KL. Correlative anatomy for the mediastinum. Thoracic surgery clinics. 2011 May:21(2):251-72, ix. doi: 10.1016/j.thorsurg.2010.12.008. Epub [PubMed PMID: 21477775]
Huang YX, Jin LZ, Lowe JA, Wang XY, Xu HZ, Teng YJ, Zhang HZ, Chi YL. Three-dimensional reconstruction of the superior mediastinum from Chinese Visible Human Female. Surgical and radiologic anatomy : SRA. 2010 Aug:32(7):693-8. doi: 10.1007/s00276-010-0627-3. Epub 2010 Feb 4 [PubMed PMID: 20131053]
Biondi A, Rausei S, Cananzi FC, Zoccali M, D'Ugo S, Persiani R. [Surgical anatomy of the anterior mediastinum]. Annali italiani di chirurgia. 2007 Sep-Oct:78(5):351-3 [PubMed PMID: 18338536]
Whitten CR, Khan S, Munneke GJ, Grubnic S. A diagnostic approach to mediastinal abnormalities. Radiographics : a review publication of the Radiological Society of North America, Inc. 2007 May-Jun:27(3):657-71 [PubMed PMID: 17495284]
Volpe JK, Makaryus AN. Anatomy, Thorax, Heart and Pericardial Cavity. StatPearls. 2023 Jan:(): [PubMed PMID: 29494059]
Rehman I, Nassereddin A, Rehman A. Anatomy, Thorax, Pericardium. StatPearls. 2023 Jan:(): [PubMed PMID: 29489245]
Wang J, Li J, Liu G, Deslauriers J. Nerves of the mediastinum. Thoracic surgery clinics. 2011 May:21(2):239-49, ix. doi: 10.1016/j.thorsurg.2011.01.006. Epub [PubMed PMID: 21477774]
Nason LK, Walker CM, McNeeley MF, Burivong W, Fligner CL, Godwin JD. Imaging of the diaphragm: anatomy and function. Radiographics : a review publication of the Radiological Society of North America, Inc. 2012 Mar-Apr:32(2):E51-70. doi: 10.1148/rg.322115127. Epub [PubMed PMID: 22411950]
Burlew JT, Weber C, Banks KP. Anatomy, Thorax, Mediastinal Lymph Nodes. StatPearls. 2023 Jan:(): [PubMed PMID: 30422458]
Shahoud JS, Kerndt CC, Burns B. Anatomy, Thorax, Internal Mammary (Internal Thoracic) Arteries. StatPearls. 2025 Jan:(): [PubMed PMID: 30726022]
Brakenhielm E, Alitalo K. Cardiac lymphatics in health and disease. Nature reviews. Cardiology. 2019 Jan:16(1):56-68. doi: 10.1038/s41569-018-0087-8. Epub [PubMed PMID: 30333526]
Oliver KA, Ashurst JV. Anatomy, Thorax, Phrenic Nerves. StatPearls. 2023 Jan:(): [PubMed PMID: 30020697]
Yasuda M, Osaki T, Fukuich Y, Kobayashi K, Iwata T, So T. Anterior mediastinal tumor as a solitary lymph node metastasis of occult thyroid carcinoma. Journal of surgical case reports. 2019 Feb:2019(2):rjz029. doi: 10.1093/jscr/rjz029. Epub 2019 Feb 14 [PubMed PMID: 30792843]
Level 3 (low-level) evidencePark MS, Moon SH, Kim TH, Oh JK, Kim HJ, Park KT, Riew KD. Surgical Anatomy of the Longus Colli Muscle and Uncinate Process in the Cervical Spine. Yonsei medical journal. 2016 Jul:57(4):968-72. doi: 10.3349/ymj.2016.57.4.968. Epub [PubMed PMID: 27189293]
Ueshima H. Transversus Thoracic Muscle Plane Block. Asian journal of anesthesiology. 2018 Dec:56(4):153. doi: 10.6859/aja.201812_56(4).0005. Epub [PubMed PMID: 30922020]
Ferrand A, Roy SK, Faure C, Moussa A, Aspirot A. Postoperative noninvasive ventilation and complications in esophageal atresia-tracheoesophageal fistula. Journal of pediatric surgery. 2019 May:54(5):945-948. doi: 10.1016/j.jpedsurg.2019.01.023. Epub 2019 Jan 31 [PubMed PMID: 30814037]
Wise-Faberowski L, Asija R, McElhinney DB. Tetralogy of Fallot: Everything you wanted to know but were afraid to ask. Paediatric anaesthesia. 2019 May:29(5):475-482. doi: 10.1111/pan.13569. Epub 2019 Apr 15 [PubMed PMID: 30592107]
Salhiyyah K, Ashoub A, Diprose P, Barlow C. Knife in the superior mediastinum: Amazing escape. Annals of cardiac anaesthesia. 2017 Apr-Jun:20(2):247. doi: 10.4103/aca.ACA_251_16. Epub [PubMed PMID: 28393789]
Saeyeldin AA, Velasquez CA, Mahmood SUB, Brownstein AJ, Zafar MA, Ziganshin BA, Elefteriades JA. Thoracic aortic aneurysm: unlocking the "silent killer" secrets. General thoracic and cardiovascular surgery. 2019 Jan:67(1):1-11. doi: 10.1007/s11748-017-0874-x. Epub 2017 Dec 4 [PubMed PMID: 29204794]
Chirica M, Kelly MD, Siboni S, Aiolfi A, Riva CG, Asti E, Ferrari D, Leppäniemi A, Ten Broek RPG, Brichon PY, Kluger Y, Fraga GP, Frey G, Andreollo NA, Coccolini F, Frattini C, Moore EE, Chiara O, Di Saverio S, Sartelli M, Weber D, Ansaloni L, Biffl W, Corte H, Wani I, Baiocchi G, Cattan P, Catena F, Bonavina L. Esophageal emergencies: WSES guidelines. World journal of emergency surgery : WJES. 2019:14():26. doi: 10.1186/s13017-019-0245-2. Epub 2019 May 31 [PubMed PMID: 31164915]
Jones SW, Williams FN, Cairns BA, Cartotto R. Inhalation Injury: Pathophysiology, Diagnosis, and Treatment. Clinics in plastic surgery. 2017 Jul:44(3):505-511. doi: 10.1016/j.cps.2017.02.009. Epub 2017 Apr 18 [PubMed PMID: 28576239]
Peters R, Peters O, Braak S, Verschakelen J. Pathology of the thymus on CT-imaging. JBR-BTR : organe de la Societe royale belge de radiologie (SRBR) = orgaan van de Koninklijke Belgische Vereniging voor Radiologie (KBVR). 2012 Sep-Oct:95(5):281-8 [PubMed PMID: 23198365]
Arabi RI, Aljudaibi A, Althumali AA, Rajb BS, Arja RD. Traumatic retrosternal hematoma leading to extra-pericardial cardiac tamponade-Case report. International journal of surgery case reports. 2019:61():30-32. doi: 10.1016/j.ijscr.2019.06.055. Epub 2019 Jun 27 [PubMed PMID: 31310858]
Level 3 (low-level) evidenceAncion A, Robinet S, Lancellotti P. [Cardiac tamponade]. Revue medicale de Liege. 2018 May:73(5-6):277-282 [PubMed PMID: 29926566]
Saleh M, Ambrose JA. Understanding myocardial infarction. F1000Research. 2018:7():. pii: F1000 Faculty Rev-1378. doi: 10.12688/f1000research.15096.1. Epub 2018 Sep 3 [PubMed PMID: 30228871]
Level 3 (low-level) evidenceJohnson OW, Chick JF, Chauhan NR, Fairchild AH, Fan CM, Stecker MS, Killoran TP, Suzuki-Han A. The thoracic duct: clinical importance, anatomic variation, imaging, and embolization. European radiology. 2016 Aug:26(8):2482-93. doi: 10.1007/s00330-015-4112-6. Epub 2015 Dec 1 [PubMed PMID: 26628065]