Introduction
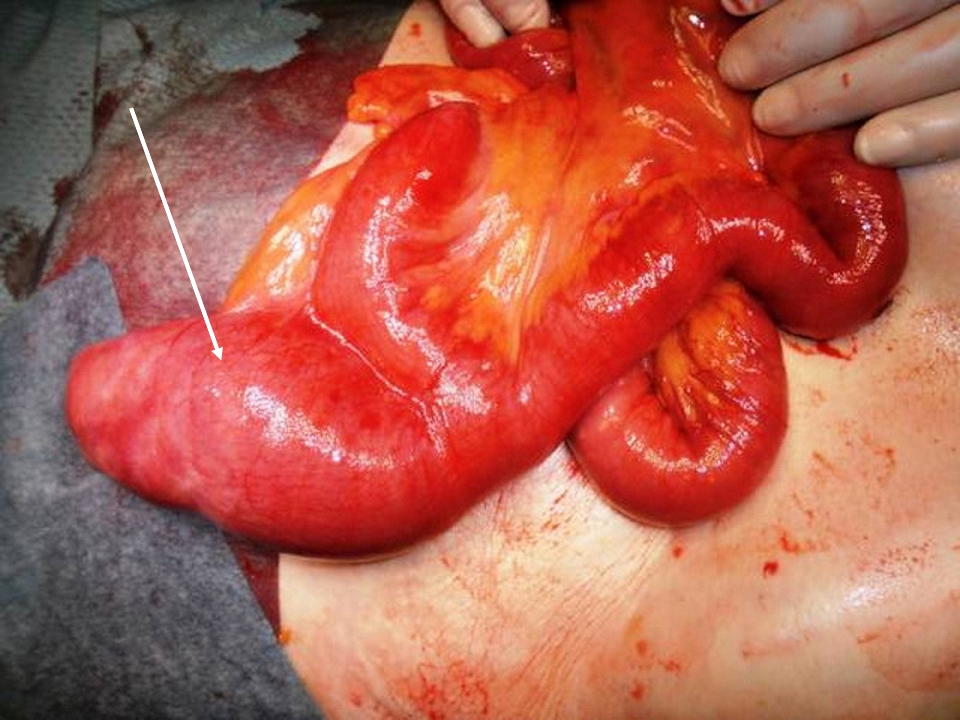
The incomplete obliteration of the omphalomesenteric duct in the developing embryo causes Meckel diverticulum. It is the most common congenital anomaly of the gastrointestinal tract.[1] The incomplete obliteration of the duct results in a diverticulum in the small intestine (see Image. Meckel Diverticulum). Often, these are completely asymptomatic.[2] Acid secretion from the ectopic gastric mucosa within the diverticulum can result in gastrointestinal bleeding and abdominal pain. It is useful to remember the rule of 2s. Meckel diverticulum occurs in 2% of the population; 2% are symptomatic, children are usually less than 2 years, affects males twice as often as females, is located 2 feet proximal to the ileocecal valve, is 2 inches long or less, and can have 2 types of the mucosal lining.[3][4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Meckel diverticulum is caused by the incomplete obliteration of the omphalomesenteric duct, which connects the yolk sac to the gut in the developing embryo (see Image. Meckel Diverticulum). It provides nutrition until the placenta forms. At about 7 weeks of gestation, the duct separates from the intestine. Suppose the duct fails to partially or entirely separate and involute. In that case, it can result in an omphalomesenteric cyst, an omphalomesenteric fistula that drains through the umbilicus, or a fibrous band from the diverticulum to the umbilicus, which can cause an obstruction.[5] If there is no additional attachment, it forms into a Meckel diverticulum. The “rule of 2s” has been used to describe a Meckel diverticulum conveniently. It is the most common congenital gastrointestinal anomaly in about 2% of infants.[1] It usually measures 2 inches long and is located in the ileum approximately 2 feet from the ileocecal valve. It is twice as common in males. It can contain 2 types of tissue (gastric or pancreatic). It is a true diverticulum because it contains all the layers of the small bowel wall. The diverticulum can sometimes have ectopic tissue within the walls. The embryonic origin of the ectopic tissue is unknown. Approximately 15% of patients have ectopic tissue within the diverticulum.[1]
Epidemiology
Meckel diverticulum is the most common congenital anomaly of the gastrointestinal tract. There is no clear familial predisposition. Patients with other malformations of the gastrointestinal tract, nervous system, or cardiovascular system have an increased risk of having a Meckel diverticulum. The prevalence of Meckel diverticulum in the general population is approximately 2%; however, it is difficult to determine the exact number because many patients are asymptomatic.[1] The patient often becomes symptomatic in the first decade of life with an average age of 2.5.[2]
Pathophysiology
Many patients with Meckel diverticulum are asymptomatic. Risk factors for increased risk of developing symptoms include age younger than 50, male gender, diverticulum greater than 2 cm long, ectopic tissue, broad-based diverticulum, and fibrous bands attached to the diverticulum.[2] The pancreatic bicarbonate in the duodenum typically neutralizes the acid secreted by the normal gastric mucosa. In a Meckel diverticulum, the ectopic gastric mucosa secretes an acid that is not neutralized, resulting in the adjacent mucosa's ulceration and painless rectal bleeding. The ectopic mucosa can also originate from the pancreas, jejunum, or a combination of the mucosa.[6] The bleeding site is usually distal to the diverticulum and not within the diverticulum. The presence of a fibrous band attached to the diverticulum can result in small bowel obstruction. The diverticulum can also act as a lead point for intussusception, leading to small bowel obstruction.[7] The incarceration of the Meckel diverticulum can also result in small bowel obstruction. Inflammation in the diverticulum can result in Meckel diverticulitis with perforation.[8][9][10]
History and Physical
Many patients who have a Meckel diverticulum never find out they have it. It is often found incidentally in imaging studies. If patients develop symptoms, they usually present in the first 10 years of life with an average age of 2.5 years with painless rectal bleeding.[2] The rectal bleeding is typically described as currant jelly or the color of brick. Children typically present with the classic “currant jelly” colored stool, while adults present with melena.[11] The bleeding usually resolves without intervention. As the patient becomes hypovolemic, the splanchnic vessels constrict to prevent further bleeding. Patients can present with a variety of gastrointestinal symptoms other than painless rectal bleeding. It should be suspected in children with recurrent or atypical intussusception, a patient with symptoms of appendicitis after their appendix has been removed, and adults with an unclear source of gastrointestinal bleeding.[1] Although it is classically described as painless rectal bleeding, some patients may present with abdominal pain.[12]
Evaluation
Clinically, Meckel diverticulum should be suspected in any child younger than 2 years of age with painless rectal bleeding. It accounts for approximately 50% of all lower gastrointestinal bleeding in children younger than 2 years of age.[11] A plain abdominal X-ray is of very low yield. Even barium studies rarely fill the diverticulum. The most sensitive test is a Meckel radionuclide scan (commonly known as a Meckel scan).[13] It is a nuclear study done by injecting technetium-99m, which is absorbed by the ectopic gastric mucosa, allowing for visualization of the Meckel diverticulum. The dye uptake can be enhanced using cimetidine, ranitidine, or glucagon. A tagged red blood cell (RBC) scan can also detect a Meckel diverticulum in patients with active bleeding. A CT scan of the abdomen and pelvis may show evidence of inflammation or obstruction at the diverticulum. More invasive methods include mesenteric angiography as well as exploratory laparoscopy.[14]
The most sensitive test is a Meckel radionuclide scan (commonly known as a Meckel scan). It is a nuclear study done by injecting technetium-99m, which is absorbed by the ectopic gastric mucosa, allowing for visualization of the Meckel diverticulum. The uptake of the dye can be enhanced using cimetidine or glucagon. The feeding artery of the Meckel diverticulum (an anomalous superior mesenteric artery branch) has a long and non-branching course and ends toward the right lower quadrant (see Image. Meckel Diverticulum With its Supplying Artery). In the case of active and ongoing bleeding, contrast extravasation is evident in the angiogram. A superior mesenteric angiogram may be helpful if the bleeding is greater than 0.5 ml/min. Usually, the bleeding has stopped by the time angiography is completed. Angiography is not very useful for most types of lower gastrointestinal bleeding.
An angiogram is only indicated when results of a barium or nuclear scan are negative. With conventional contrast arteriography, a Meckel diverticulum is characterized by the finding of an anomalous superior mesenteric artery branch feeding the diverticulum. A bleeding Meckel diverticulum diagnosis can be established by Meckel scan or mesenteric arteriography, double-balloon enteroscopy, and capsule endoscopy. However, if diagnostic testing is inconclusive, or the patient is hemodynamically unstable, either laparotomy or laparoscopy is indicated to determine whether a Meckel's diverticulum is the source of bleeding.[15][16][17]
Treatment / Management
If the patient has had significant blood loss, the patient should undergo volume resuscitation. Patients may require a blood transfusion if significant blood is lost. The treatment of symptomatic Meckel diverticulum is surgical excision. The diverticulum can be removed via laparoscopic or open technique.[18] The diverticulum should be excised along with the adjacent ileum. There is a growing trend to perform the excision laparoscopically rather than using the open technique.[18] The treatment of asymptomatic Meckel diverticulum is controversial (surgery versus observation). When a Meckel diverticulum is incidentally discovered during abdominal surgery for another condition, most surgeons recommend removal.[18]
Differential Diagnosis
The differential diagnosis is broad, including any cause of gastrointestinal bleeding. Massive gastrointestinal bleeding is uncommon in childhood. Stool may be mistaken for hematochezia if children ingest bismuth, iron, or spinach. A hemoccult test shows that the stool is negative. In infants, swallowed maternal blood from bleeding nipples, milk protein allergy, intussusception, and anal fissures can commonly cause rectal bleeding. Necrotizing enterocolitis should be on the differential in neonates and premature infants. Other common causes of rectal bleeding in older children include colitis, gastroenteritis, HSP, HUS, intussusception, inflammatory bowel disease, and vascular malformation.
Complications
The most common complication of Meckel diverticulum in children is rectal bleeding, which results in anemia.[7] The most common complication in adults is a small bowel obstruction.[19] The etiology of the obstruction may be secondary to the omphalomesenteric band, internal hernia, volvulus around the vitelline duct remnants, and intussusception, in which the diverticulum acts as the lead point.[7] The diverticulum can become inflamed, resulting in Meckel diverticulitis with perforation and peritonitis.
Enhancing Healthcare Team Outcomes
A team approach should be used to provide the best care for a patient with Meckel diverticulum. Multiple specialists may be involved, including emergency medicine, gastroenterology, radiology, surgery, and nuclear medicine. There are several potential complications, and the physicians should educate the nurses to watch for them and be encouraged to report any abnormal findings. In particular, these patients are at risk of developing perforation and acute peritonitis.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Sagar J, Kumar V, Shah DK. Meckel's diverticulum: a systematic review. Journal of the Royal Society of Medicine. 2006 Oct:99(10):501-5 [PubMed PMID: 17021300]
Level 1 (high-level) evidencePark JJ, Wolff BG, Tollefson MK, Walsh EE, Larson DR. Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950-2002). Annals of surgery. 2005 Mar:241(3):529-33 [PubMed PMID: 15729078]
Hansen CC, Søreide K. Systematic review of epidemiology, presentation, and management of Meckel's diverticulum in the 21st century. Medicine. 2018 Aug:97(35):e12154. doi: 10.1097/MD.0000000000012154. Epub [PubMed PMID: 30170459]
Level 1 (high-level) evidenceFrancis A,Kantarovich D,Khoshnam N,Alazraki AL,Patel B,Shehata BM, Pediatric Meckel's Diverticulum: Report of 208 Cases and Review of the Literature. Fetal and pediatric pathology. 2016; [PubMed PMID: 27064958]
Level 3 (low-level) evidenceYahchouchy EK, Marano AF, Etienne JC, Fingerhut AL. Meckel's diverticulum. Journal of the American College of Surgeons. 2001 May:192(5):658-62 [PubMed PMID: 11333103]
Uppal K, Tubbs RS, Matusz P, Shaffer K, Loukas M. Meckel's diverticulum: a review. Clinical anatomy (New York, N.Y.). 2011 May:24(4):416-22. doi: 10.1002/ca.21094. Epub 2011 Feb 14 [PubMed PMID: 21322060]
St-Vil D, Brandt ML, Panic S, Bensoussan AL, Blanchard H. Meckel's diverticulum in children: a 20-year review. Journal of pediatric surgery. 1991 Nov:26(11):1289-92 [PubMed PMID: 1812259]
Level 2 (mid-level) evidenceEvola G, Piazzese E, Bonanno S, Di Stefano C, Di Fede GF, Piazza L. Complicated Littre's umbilical hernia with normal Meckel's diverticulum: A case report and review of the literature. International journal of surgery case reports. 2021 Jul:84():106126. doi: 10.1016/j.ijscr.2021.106126. Epub 2021 Jun 18 [PubMed PMID: 34186459]
Level 3 (low-level) evidenceLópez-Lizárraga CR, Sánchez-Muñoz MP, Juárez-López GE, Pelayo-Orozco L, De la Cerda-Trujillo LF, Ploneda-Valencia CF. A rare case of a strangulated Littre's hernia with Meckel's diverticulum duplication. Case report and literature review. International journal of surgery case reports. 2017:33():58-61. doi: 10.1016/j.ijscr.2017.02.032. Epub 2017 Feb 21 [PubMed PMID: 28273609]
Level 3 (low-level) evidenceHorkoff MJ, Smyth NG, Hunter JM. A large incarcerated Meckel's diverticulum in an inguinal hernia. International journal of surgery case reports. 2014:5(12):899-901. doi: 10.1016/j.ijscr.2014.09.036. Epub 2014 Oct 17 [PubMed PMID: 25460431]
Level 3 (low-level) evidenceRattan KN, Singh J, Dalal P, Rattan A. Meckel's diverticulum in children: Our 12-year experience. African journal of paediatric surgery : AJPS. 2016 Oct-Dec:13(4):170-174. doi: 10.4103/0189-6725.194671. Epub [PubMed PMID: 28051045]
Kuru S, Kismet K. Meckel's diverticulum: clinical features, diagnosis and management. Revista espanola de enfermedades digestivas. 2018 Nov:110(11):726-732. doi: 10.17235/reed.2018.5628/2018. Epub [PubMed PMID: 30032625]
Elsayes KM, Menias CO, Harvin HJ, Francis IR. Imaging manifestations of Meckel's diverticulum. AJR. American journal of roentgenology. 2007 Jul:189(1):81-8 [PubMed PMID: 17579156]
Routh WD, Lawdahl RB, Lund E, Garcia JH, Keller FS. Meckel's diverticula: angiographic diagnosis in patients with non-acute hemorrhage and negative scintigraphy. Pediatric radiology. 1990:20(3):152-6 [PubMed PMID: 2352792]
Level 3 (low-level) evidenceTitley-Diaz WH, Aziz M. Meckel Scan. StatPearls. 2024 Jan:(): [PubMed PMID: 32809335]
Kovacs M, Botstein J, Braverman S. Angiographic diagnosis of Meckel's diverticulum in an adult patient with negative scintigraphy. Journal of radiology case reports. 2017 Mar:11(3):22-29. doi: 10.3941/jrcr.v11i3.2032. Epub 2017 Mar 31 [PubMed PMID: 28584569]
Level 3 (low-level) evidenceLee JM, Jeen CD, Kim SH, Lee JS, Nam SJ, Choi HS, Kim ES, Keum B. Meckel's diverticulum detected by computed tomographic enterography: report of 3 cases and review of the literature. The Turkish journal of gastroenterology : the official journal of Turkish Society of Gastroenterology. 2014 Apr:25(2):212-5. doi: 10.5152/tjg.2014.6044. Epub [PubMed PMID: 25003685]
Level 3 (low-level) evidenceRuscher KA, Fisher JN, Hughes CD, Neff S, Lerer TJ, Hight DW, Bourque MD, Campbell BT. National trends in the surgical management of Meckel's diverticulum. Journal of pediatric surgery. 2011 May:46(5):893-6. doi: 10.1016/j.jpedsurg.2011.02.024. Epub [PubMed PMID: 21616248]
Dumper J, Mackenzie S, Mitchell P, Sutherland F, Quan ML, Mew D. Complications of Meckel's diverticula in adults. Canadian journal of surgery. Journal canadien de chirurgie. 2006 Oct:49(5):353-7 [PubMed PMID: 17152574]
Level 3 (low-level) evidence