Introduction
Mechanical ventilation is a critical intervention to sustain life in acute or emergent settings, particularly in patients with compromised airways, impaired ventilation, or hypoxemic respiratory failure. This procedure involves applying positive pressure breaths and relies on the airway system's compliance and resistance. Clinicians in critical care units must understand how mechanical ventilation affects patient physiology and response to various disease states, emphasizing the need for a deep understanding of safe application principles. A solid understanding of human physiology and airway mechanics principles is crucial for clinicians in treating intubated patients, forming the foundation for safe and effective ventilation strategies. This knowledge is essential for recognizing key indications for invasive mechanical ventilation to select the common and appropriate ventilation modes, initial settings, and supportive care for intubated patients, which are reviewed below. Noninvasive ventilation is addressed separately.[1]
The primary indications for invasive mechanical ventilation are categorized as follows:
- Airway compromise due to disease
- Patients who are obtunded or with dynamic airways need airway protection, such as those from trauma or oropharyngeal infection.
- Patients with airway obstruction can experience either proximal (such as angioedema) or distal issues (such as asthmatic bronchospasm or acute exacerbation of chronic obstructive pulmonary disease or COPD).
- Hypoventilation can result from impaired drive, pump failure, or gas exchange difficulties, leading to hypercapnic respiratory failure. The etiology of the condition can be divided into the following subcategories:
- Impaired central drive (such as drug overdose)
- Respiratory muscle weakness (such as muscular dystrophy and myositis)
- Peripheral nervous system defects (such as Guillain-Barré syndrome or myasthenic crisis)
- Restrictive ventilatory defects (such as chest wall trauma or disease or massive pneumothorax or effusion)
- Hypoxemic respiratory failure may arise from the inability to effectively exchange oxygen or deliver it to peripheral tissues due to the following reasons:
- Alveolar filling defects (such as pneumonia, acute respiratory distress syndrome (ARDS), or pulmonary edema)
- Pulmonary vascular defects leading to ventilation-perfusion mismatch (such as massive pulmonary embolism or air emboli)
- Diffusion defects (such as advanced pulmonary fibrosis)
- Increased ventilatory demand can result from conditions such as severe sepsis, shock, or severe metabolic acidosis.[2][3][4][5][6]
Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Function
Mechanical ventilation operates by applying a positive pressure breath, relying on the compliance and resistance of the airway system. During spontaneous inspiration, the lung expands as transpulmonary pressure primarily stems from a negative pleural pressure generated by the inspiratory muscles. In contrast, controlled mechanical ventilation utilizes positive airway pressure to drive gas into the lungs, creating a positive-pressure environment.[7] Tidal volume (VT) represents the air exchanged during each respiratory cycle.[8] Physiologically, VT is influenced by the individual's height and gender, typically between 8 and 10 mL/kg of ideal body weight.[2] Mechanical ventilation can be administered through various modes, including mandatory or assisted modes. In the assisted mode, the patient's inspiratory effort triggers the mechanical ventilation to deliver the breath. At the same time, the pressure is the product of negative pleural pressure and positive alveolar pressure.
The most common modes of mechanical ventilation include:
- Volume-limited assist control (VAC) ventilation
- Pressure-limited assist control (PAC) ventilation
- Synchronized intermittent mandatory ventilation (SIMV) with pressure support ventilation (PSV)
PSV is usually not used as a primary mode; instead, it is commonly used during the weaning process from mechanical ventilation. Other types of mechanical ventilation modes include controlled mechanical ventilation, which can be volume-limited or pressure-limited, as well as intermittent mandatory ventilation. Additionally, airway pressure release ventilation (APRV) or bilevel mechanical ventilation are less frequently used as initial settings.[9] Breath delivery in mechanical ventilation can generally be categorized as volume-limited or pressure-limited. Variations in tidal volume (VT) and airway pressure occur depending on respiratory compliance, airway resistance, and the specific mode of mechanical ventilation used. For instance, VT is set to a fixed amount in VAC mode, with the static airway pressure (or plateau pressure at end inspiration) influenced by lung compliance. Conversely, in PAC mode, the driving pressure is set and fixed, resulting in variable VT from breath to breath, which depends on lung compliance (ie, higher lung compliance leads to higher VT, and lower lung compliance leads to lower VT).
Mechanical ventilation comprises four stages: the trigger phase, the inspiratory phase, the cycling phase, and the expiratory phase. The trigger phase initiates inhalation, either prompted by the patient's effort or predefined parameters set by the mechanical ventilator. The inspiratory phase involves the intake of air into the patient's lungs. Following inspiration, the cycling phase denotes the cessation of inhalation but precedes the onset of exhalation. Lastly, the expiratory phase signifies the passive exhalation of air from the patient's lungs.
Setting Mechanical Ventilation
The mechanical ventilation modes mentioned above are used for initiation. The selection of mechanical ventilation mode should be personalized to ensure safety by optimizing ventilation-perfusion matching and the pressure-volume relationship of the lungs.[10] In addition, patient-ventilator synchrony and comfort are important factors for the mode selection.
VAC mode: When VAC mode is chosen, the following parameters have to be set on the ventilator:
- Tidal volume (VT): The tidal volume is usually determined based on ideal or predicted body weight (PBW) rather than actual weight. In conditions such as ARDS that require a protective lung strategy, the VT is set at a low range of 4 to 8 mL/kg PBW.
- Respiratory rate (RR): The respiratory rate is typically between 12 and 16 breaths per minute. A higher respiratory rate (up to 35 breaths per minute) may be selected to achieve sufficient minute ventilation, especially during a protective lung strategy in ARDS to prevent severe hypercapnia or counteract severe acidosis.
- Inspiratory flow rate (IFR): The inspiratory flow rate is usually set between 40 and 60 L/min to achieve an inspiratory and expiratory ratio of 1:2 or 1:3. A higher inspiratory flow rate (up to 90 L/min) is often recommended in cases of severe distal airway obstruction, such as acute COPD exacerbation or severe asthma exacerbation. This higher rate allows for longer expiratory time to empty the lungs, targeting an inspiratory-to-expiratory ratio (I:E) greater than 1:3.
- Fraction of inspired oxygen (FiO2): FiO2 should be adjusted to the minimum level necessary to maintain a pulse oximetry (SpO2) reading of 90% to 96%. Avoiding hyperoxemia is crucial, as studies have demonstrated an increase in mortality among critically ill patients with excessive oxygen levels.
- Positive end-expiratory pressure (PEEP): PEEP increases the functional residual capacity and prevents the collapse of alveoli, thus reducing atelectrauma. Initially, the PEEP level is typically set at 5 cm H2O and adjusted based on the patient's underlying condition and oxygenation requirements. PEEP is titrated according to respiratory system mechanics or guidelines such as the ARDS network table in conditions such as ARDS.
- Trigger sensitivity: Triggers can be categorized into 2 types—flow trigger and pressure trigger. Pressure triggers are typically set at -2 cm H2O but should be avoided if auto-PEEP is suspected. In such cases, flow triggers should be used and set at a threshold of 2 L/min.[2][11][12][13][14][15]
PAC mode: The following parameters must be adjusted on the ventilator when using PAC mode:
- Inspiratory pressure (Pi): As discussed above, the inspiratory pressure level is usually set between 10 and 20 cm H2O, based on the patient's underlying condition to achieve adequate VT.
- Inspiratory time (Ti): Inspiratory time is typically set to 1 second and adjusted to achieve an I:E ratio of 1:2 to 1:3.
- PEEP and FiO2 settings are selected similarly to VAC mode. However, the inspiratory pressure adds additional pressure to the peak airway pressure and may further increase the risk of barotrauma.
SIMV/PSV mode: When SIMV/PSV mode is selected, the initial settings include the following:
- Pressure support (PS): The pressure support typically ranges from 5 to 15 cm H2O for spontaneous breaths initiated by the patient above the set rate. It can be adjusted as needed to maintain certain minute ventilation.
- Tidal volume (VT): The tidal volume is set similarly to VAC mode to achieve targeted minute ventilation without causing ventilator-associated lung injury (typically 4 to 8 mL/kg PBW) for the non-spontaneous breaths.
Airway Pressure Release Ventilation Mode
APRV is a form of continuous positive airway pressure (CPAP) characterized by timed pressure release while allowing for spontaneous breathing (see Graph. APRV Pressure Cycles With Superimposed Spontaneous Breathing).[16] APRV provides continuous pressure to keep the lungs open, with a timed release to lower the set pressure. This continuous pressure phase facilitates the recruitment of proximal and distal alveoli by transmitting pressure to the chest wall. The prolonged continuous pressure phase, along with the short release phase, helps prevent continuous cycles of recruitment-derecruitment seen in pressure or volume control ventilation settings. This mechanism aids in avoiding atelectrauma, barotrauma, and ventilator-induced lung injury.
The timed release in APRV facilitates passive exhalation and enhances CO2 clearance. Due to its reliance on spontaneous ventilation, APRV necessitates less sedation than conventional modes, reducing the risk of sedation-related complications (see Graph. Tidal Volume Comparison During APRV Versus Conventional Ventilation). Spontaneous breathing can increase end-expiratory lung volume, decrease atelectasis, and improve ventilation to dependent lung regions. Spontaneous breathing in APRV can raise end-expiratory lung volume, reduce atelectasis, and enhance ventilation in dependent lung regions. Moreover, spontaneous breathing improves the hemodynamic profile by lowering intrathoracic pressure and enhancing preload and cardiac output.
Setting up APRV involves adjusting 4 main variables: P-high, P-low, T-high, and T-low.[17] P-high represents the continuous pressure set, whereas P-low signifies the pressure release phase of the cycle. T-high determines the duration of the continuous pressure, whereas T-low indicates the release phase duration. Initially, the patient should be placed on assist control/volume control (AC/VC) immediately post-intubation until paralysis subsides. Subsequently, an inspiratory hold maneuver should be performed to determine the plateau pressure, which becomes the P-high and typically ranges from 27 to 29 cm H2O. However, obese patients may require higher pressures. P-low is usually set to 0, considering that in most cases, intrinsic PEEP (iPEEP) prevents full exhalation.
The T-high is typically set to 4 to 6 seconds, while the T-low is adjusted to 0.2 to 0.8 seconds in restrictive lung disease and 0.8 to 1.5 seconds in obstructive lung disease cases. Examining the flow-time waveform on the ventilator is crucial to set the T-low accurately. The T-low should ideally be around 75% of the peak expiratory flow rate (PEFR) for optimal ventilation (see Graph. Peak Expiratory Flow Rate Curve Illustration).[18] Continuous monitoring and readjustment of T-low to maintain this target are necessary as lung recruitment progresses. During APRV, FiO2 levels should be titrated downward gradually as the patient's comfort and oxygenation permit.
Spontaneous breathing is paramount in APRV, and a slight amount of pressure support or automatic tube compensation should be provided to counter the endotracheal tube's intrinsic resistance. Hypoxemia in APRV can be addressed by increasing both P-high and T-high settings.[19] Alternatively, shortening the T-low can also help correct hypoxemia. APRV allows for permissive hypercapnia; however, excessive hypercapnia can be managed by reducing sedation or increasing P-high and T-high settings. Increasing T-low can also alleviate hypercapnia, but this approach is limited as APRV relies on iPEEP during P-low to maintain lung recruitment. Augmenting T-low may reduce iPEEP, thereby risking alveolar derecruitment.
Issues of Concern
Ventilator-Associated Lung Injury
Ventilator-associated lung injury often occurs when ventilator settings are not adjusted based on PBW, especially in conditions like ARDS characterized by stiff lungs. Utilizing a lung-protective strategy involving low tidal volumes and targeted airway pressures is crucial to prevent lung injuries in these cases.[20]
Ventilator-Associated Events
Ventilator-associated events refer to a deterioration in respiratory status after a period of stability or improvement on the ventilator, accompanied by evidence of infection or inflammation and laboratory confirmation of respiratory infection.[21] Risk factors for ventilator-associated events include sedation (such as with benzodiazepines or propofol), fluid overload, high tidal-volume ventilation, and high inspiratory driving pressures.[22] Strategies to mitigate ventilator-associated events include implementing ventilator bundles to reduce sedation, conducting daily spontaneous awakening and breathing trials, promoting early mobilization, adopting conservative fluid and transfusion strategies, and employing lung-protective ventilation strategies. Recent studies have explored the impact of these interventions on patient outcomes, including the effectiveness of ventilator bundles.[23][24]
Hemodynamic Changes
Transitioning a patient to mechanical ventilation shifts from natural negative pressure ventilation to positive pressure ventilation, impacting heart-lung physiology and altering hemodynamic status. Positive pressure ventilation elevates intrathoracic pressure, leading to decreased right ventricular preload and left ventricular preload and afterload. Additionally, the increased pressure augments the right ventricular afterload.[25] Although these effects may have minimal impact on the hemodynamics of a healthy individual, they can cause significant alterations in critically ill patients. For instance, a patient with acute pulmonary edema may benefit from reduced preload, whereas this change may not be beneficial for someone in septic shock.
Clinical Significance
Clinical strategies for ventilator management may include lung-protective, obstructive, and intermediate strategies.
Lung-Protective Strategy
The lung-protective strategy is recommended for patients at risk of developing acute lung injury or progressing to ARDS. This approach involves using low tidal volume ventilation, as demonstrated in landmark trials such as the ARMA study, which showed improved mortality in ARDS patients with low tidal volume ventilation. This method is used to prevent barotrauma, volume trauma, and atelectatic trauma. Patients with conditions such as pneumonia, severe aspiration, pancreatitis, and sepsis are examples of those at risk and should be treated using the lung-protective strategy. A tidal volume (VT) of 6 mL/kg based on ideal body weight is recommended.[26][27][28] In patients with acute lung injury progressing to ARDS, lung recruitment diminishes, and shunts develop, reducing functional lung volume. A low tidal volume strategy offsets the decreased functional lung volume. Tidal volume should not be adjusted based on minute ventilation goals; the respiratory rate should be adjusted based on minute ventilation goals and the patient's acid-base status. A starting respiratory rate of 16 breaths per minute is generally suitable for most patients to maintain normocapnia.[29]
A blood gas analysis should be obtained approximately 30 minutes after initiating mechanical ventilation, guiding adjustments to the respiratory rate based on the patient's acid-base status and PaCO2 levels. If PaCO2 significantly exceeds 40 mm Hg, the respiratory rate should be increased; conversely, if PaCO2 is notably below 40 mm Hg, the respiratory rate should be decreased. End-tidal carbon dioxide (EtCO2) is not a reliable indicator of PaCO2 due to physiological shunt, dead space, and reduced cardiac output influencing EtCO2 levels. The inspiratory flow rate is typically set at 60 L/min but can be adjusted higher if the patient demonstrates increased inspiratory effort at the onset of inspiration.[30] Following intubation, it is advisable to reduce the FiO2 to 40% immediately to prevent hyperoxemia.[13] The lung-protective strategy involves controlling both the FiO2 and PEEP adjustments simultaneously. Poor oxygenation in acute lung injury results from derecruited alveoli and a physiological shunt. Consequently, FiO2 and PEEP should be incrementally increased together to address this issue. The oxygenation target should align with the ARDSnet protocol, aiming for 88% to 95% range.
ARDSnet PEEP/FiO2 protocol: After initiating mechanical ventilation, it is essential to regularly reassess its effects on the patient, particularly on the alveoli.[31] This assessment involves monitoring the plateau pressure and driving pressure. The plateau pressure reflects the pressure exerted on small airways and alveoli and should ideally be maintained below 30 to avoid volume trauma and lung injury resulting from alveolar overdistension. An inspiratory pause must be initiated to measure the plateau pressure.
The driving pressure represents the tidal volume relative to lung compliance, indicating the "functional" lung volume that remains recruitable and unshunted. Calculating the driving pressure involves subtracting the PEEP level from the plateau pressure.[32] If the driving pressure exceeds 14, reducing tidal volume (VT) to 4 mL/kg is crucial when plateau and driving pressures surpass these thresholds. Increasing the respiratory rate can help offset the decrease in minute ventilation, although permissive hypercapnia may be unavoidable. Permissive hypercapnia is a strategy that tolerates elevated PCO2 levels to facilitate lung-protective ventilation with low tidal volumes.[33] However, recruitment maneuvers have been associated with increased mortality in moderate-to-severe ARDS and should not be used routinely.[34]
Obstructive Strategy
Patients with obstructive lung diseases like asthma and COPD are typically treated initially with noninvasive ventilation. However, in some cases, they may require intubation and mechanical ventilation. Obstructive lung diseases are characterized by narrowed airways and small airway collapse during expiration, leading to increased airflow resistance and decreased expiratory flow rates. This condition prolongs exhalation time, making it difficult to exhale the tidal volume before the next inhalation fully. As a result, residual air may remain in the chest at the start of inhalation. As the air becomes trapped in the alveoli, intrathoracic pressure increases, leading to a phenomenon known as auto-PEEP. This elevated pressure must be overcome during inhalation. As more air becomes trapped in the chest, flattening the diaphragm and expanding the lungs decrease compliance, leading to dynamic hyperinflation. With the progression of auto-PEEP and dynamic hyperinflation, there is increased work of breathing, reduced inhalation efficiency, and a risk of hemodynamic instability due to elevated intrathoracic pressure. Given these challenges, the ventilator strategy must counteract these pathologically increased pressures. Additionally, to address the obstructive process effectively, ventilatory management should be integrated with maximal medical therapy, including in-line nebulizers.
Extending the expiratory phase to allow for a complete exhalation can reduce auto-PEEP and dynamic hyperinflation when managing the ventilator for an obstructive patient.[2] Most patients require deep sedation to avoid over-breathing the ventilator and excessive inspiratory efforts. Tidal volume (VT) should be set to 8 mL/kg, while the initial respiratory rate (RR) should be set at 10 breaths per minute.[30] These settings provide sufficient time for full expiration, thus reducing auto-PEEP. This approach often aligns with the permissive hypercapnia strategy, focusing on lower tidal volumes and adequate oxygenation rather than PaCO2 levels. The inspiratory flow rate should be 60 L/min, while FiO2 should be maintained at 40% after initiating ventilation. In obstructive lung diseases, the primary issue is ventilation rather than oxygenation, so increasing FiO2 is generally unnecessary. Minimal PEEP is recommended, with some studies suggesting a PEEP of 0 and others suggesting a small amount to counteract auto-PEEP.
The ventilator waveform should be carefully assessed. If the waveform does not return to baseline (0) by the start of the next breath, the respiratory rate must be reduced to prevent increased hyperinflation and auto-PEEP. If a patient experiences a sudden desaturation or drop in blood pressure, they should be disconnected from the ventilator to allow for a complete exhalation. A clinician may assist exhalation by applying pressure to the patient's chest. A comprehensive evaluation, including ruling out pneumothorax due to volume trauma, is necessary.[29] If plateau pressures remain chronically high, it is also essential to rule out the possibility of pneumothorax.
Intermediate Strategy
The PReVENT trial found no significant difference between an intermediate tidal volume strategy (10 mL/kg) and a low tidal volume strategy (6 mL/kg) in patients without ARDS.[35] For patients without obstructive physiology or acute lung injury risk, an intermediate tidal volume strategy (8-10 mL/kg) may be appropriate. Typically, these patients do not experience significant oxygenation or ventilation challenges, so minimal ventilator settings are often adequate. Starting with a tidal volume (VT) of 8 mL/kg, respiratory rate (RR) of 16, inspiratory flow rate (IFR) of 60 L/min, FiO2 of 40%, and PEEP of 5 cm H2O, with titration as needed, is a reasonable starting point.
Other Issues
Ventilator bundles are crucial in preventing ventilator-associated events. These measures include minimizing sedation, conducting daily spontaneous breathing trials, promoting early mobilization, adopting conservative fluid and transfusion strategies, and implementing lung-protective strategies.
Sedation
Sedation is critical in treating patients on mechanical ventilation, especially in providing pain control and ensuring comfort post-intubation. An "analgesia first" sedation strategy is preferred, with fentanyl being a commonly used agent due to its minimally hypotension-inducing hemodynamic properties.[36][37] If a patient remains agitated despite starting analgesic sedation, additional agents like propofol may be considered based on the patient's hemodynamic status and clinical requirements. In addition, obtaining a chest x-ray and blood gas analysis is crucial to confirm proper endotracheal tube placement and evaluate minute ventilation. Although some centers use ultrasound for endotracheal tube confirmation, it is not yet standard practice everywhere. Regular monitoring of plateau pressures is essential to evaluate alveolar integrity.
Mobility
All patients undergoing mechanical ventilation should have the head of the bed elevated to at least 30°. Based on a 2016 Cochrane review on ventilator-associated pneumonia, a semi-recumbent position (30°-60°) reduced clinically suspected ventilator-associated pneumonia by 25.7% compared to a 0° to 10° supine position. Nonetheless, it is noteworthy that the available data on this topic is limited.[38]
Airway Maintenance
If a patient suddenly desaturates, clinicians should follow the DOPES mnemonic to identify potential causes. DOPES stands for displacement, obstruction of the endotracheal tube or airways, pneumothorax/pulmonary embolism/pulmonary edema, equipment failure, and stacked breaths. The patient should be disconnected from the ventilator and switched to a bag valve mask. The individual performing bagging should ventilate calmly and allow for a full exhalation. Following this, clinicians should adopt a systematic approach, as mentioned below.
- Is the patient's EtCO2 still showing a good waveform? If not, the endotracheal tube may have been dislodged.
- Does the patient bag easily or with difficulty? If bagging is difficult, it may indicate obstructive problems such as an obstructed endotracheal tube, pneumothorax, or bronchospasm.
- Equipment failure is suggested if the patient bags easily and SpO2 rises rapidly. During the failure evaluation, another clinician should assess the patient using an ultrasound of the lungs and heart and obtain a chest X-ray. If no other cause of desaturation is found, pulmonary embolism should be considered.
Venous Thromboembolism Prophylaxis
Invasive mechanical ventilation independently increases the risk of venous thromboembolism in the intensive care unit.[39] Therefore, implementing prophylactic measures is crucial to prevent additional morbidities.
Gastrointestinal Prophylaxis
Gastrointestinal bleeding affects approximately 5% of critically ill patients who are not receiving prophylaxis.[40] In a multicenter study, invasive mechanical ventilation was identified as 1 of the 2 independent risk factors for gastrointestinal bleeding (odds ratio for bleeding, 15.6; 95% CI, 3.0 to 80.1).[41] Therefore, implementing an acid suppression strategy for mechanically ventilated patients has been recommended.[42] Proton pump inhibitors are the most effective agents for preventing clinically important gastrointestinal bleeding, although their use may increase the risk of pneumonia. Continuing acid suppression beyond discharge from the intensive care unit is unnecessary.[43]
Enhancing Healthcare Team Outcomes
Emphasizing the importance of effective communication among interprofessional healthcare team members is crucial when caring for mechanically ventilated patients. Respiratory therapists are critical in ventilator management, and their expertise should be effectively utilized.[44] Notably, assigning a single dedicated healthcare professional for ventilator management is crucial to ensure consistency and accuracy in care. To ensure proper treatment alignment, all adjustments to the ventilator must be communicated and coordinated with other healthcare team members responsible for the patient's overall care.
Media
(Click Image to Enlarge)
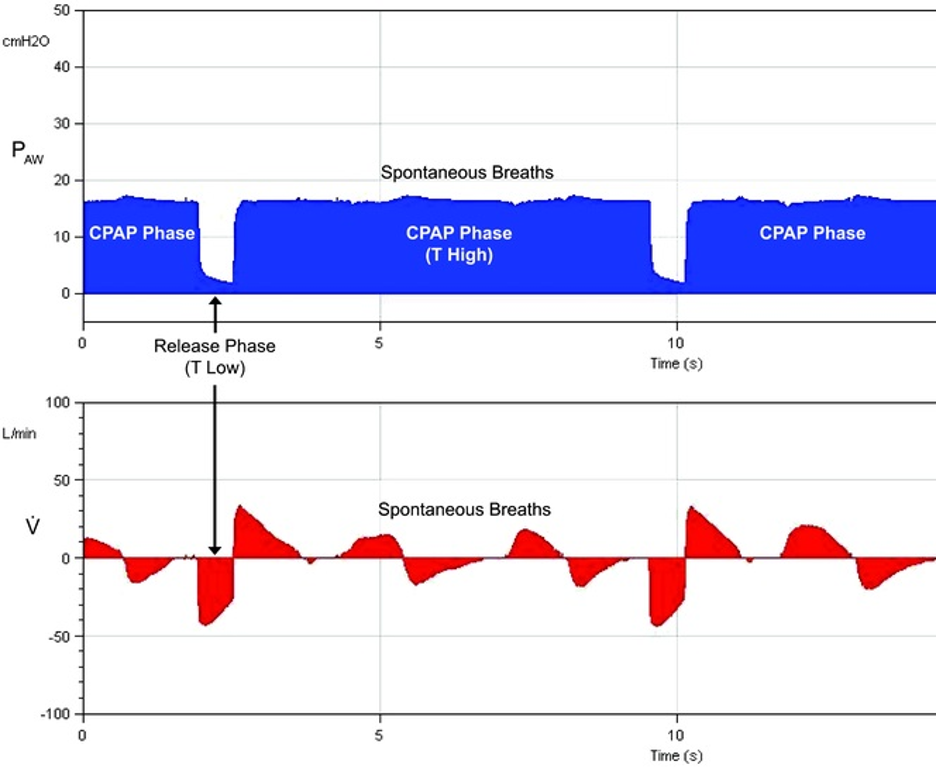
APRV Pressure Cycles With Superimposed Spontaneous Breathing. APRV involves pressure cycles with superimposed spontaneous breathing, and this mode functions as a form of CPAP. Here, P-high represents the CPAP level, and T-high indicates the duration of P-high. During APRV, the CPAP phase (P-high) is periodically released to a P-low for a brief period (T-low), and then the CPAP level is re-established on the subsequent breath. Spontaneous breathing can occur at both pressure levels and is not dependent on time cycling.
Habashi NM. Other approaches to open-lung ventilation: airway pressure release ventilation. Crit Care Med. 2005;33(3 suppl):228-240. doi: 10.1097/01.ccm.0000155920.11893.37.
(Click Image to Enlarge)
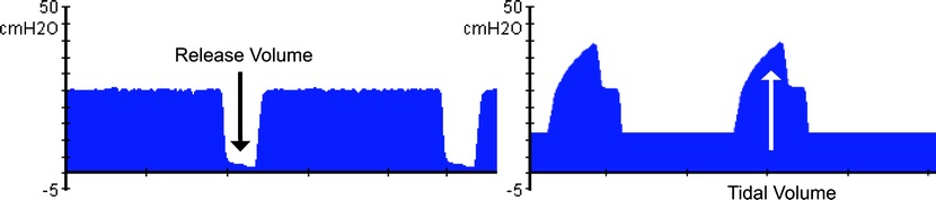
Tidal Volume Comparison During APRV Versus Conventional Ventilation. In APRV, release volumes augment ventilation, which is associated with decreasing airway pressure and lung distension. Conversely, during conventional ventilation, tidal volumes are generated by increasing airway pressure and lung distension.
Habashi NM. Other approaches to open-lung ventilation: airway pressure release ventilation. Crit Care Med. 2005;33(3 suppl):228-240. doi: 10.1097/01.ccm.0000155920.11893.37.
(Click Image to Enlarge)
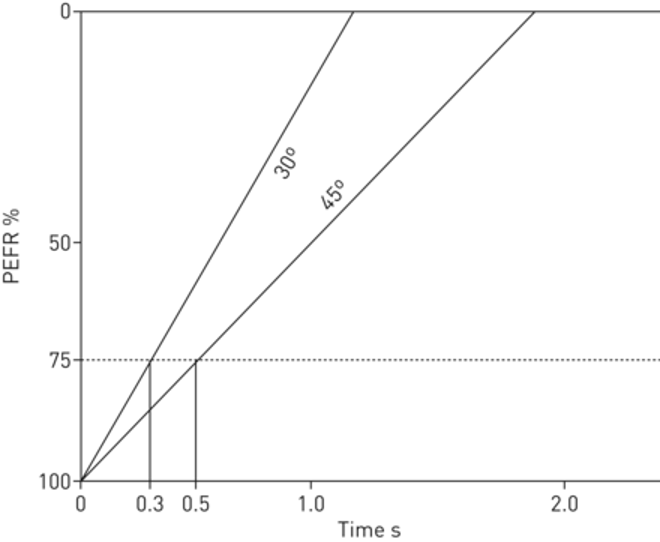
Peak Expiratory Flow Rate Curve Illustration. A patient with initially low lung compliance exhibits a steeper expiratory flow curve (30° angle) and requires a short release phase (T-low) of 0.3 seconds (in this example) to terminate expiratory flow at 75% of PEFR. As the lung recruitment improves compliance, the slope decreases to a 45° angle, necessitating an extended T-low time of 0.5 seconds (in this example). The lung's ability to accommodate larger tidal volumes improves with alveolar recruitment and increasing compliance. Thus, APRV enables time-controlled and adaptive mechanical ventilation tailored to the patient's respiratory system mechanics (time-controlled adaptive ventilation).
Habashi NM. Other approaches to open-lung ventilation: airway pressure release ventilation. Crit Care Med. 2005;33(3suppl):228-240. doi: 10.1097/01.ccm.0000155920.11893.37.
References
Gong Y, Sankari A. Noninvasive Ventilation. StatPearls. 2024 Jan:(): [PubMed PMID: 35201716]
Pham T, Brochard LJ, Slutsky AS. Mechanical Ventilation: State of the Art. Mayo Clinic proceedings. 2017 Sep:92(9):1382-1400. doi: 10.1016/j.mayocp.2017.05.004. Epub [PubMed PMID: 28870355]
Farkas A, Lynch MJ, Westover R, Giles J, Siripong N, Nalatwad A, Pizon AF, Martin-Gill C. Pulmonary Complications of Opioid Overdose Treated With Naloxone. Annals of emergency medicine. 2020 Jan:75(1):39-48. doi: 10.1016/j.annemergmed.2019.04.006. Epub 2019 Jun 8 [PubMed PMID: 31182316]
Jablonski R, Bhorade S, Strek ME, Dematte J. Recognition and Management of Myositis-Associated Rapidly Progressive Interstitial Lung Disease. Chest. 2020 Jul:158(1):252-263. doi: 10.1016/j.chest.2020.01.033. Epub 2020 Feb 12 [PubMed PMID: 32059958]
Neumann B, Angstwurm K, Mergenthaler P, Kohler S, Schönenberger S, Bösel J, Neumann U, Vidal A, Huttner HB, Gerner ST, Thieme A, Steinbrecher A, Dunkel J, Roth C, Schneider H, Schimmel E, Fuhrer H, Fahrendorf C, Alberty A, Zinke J, Meisel A, Dohmen C, Stetefeld HR, German Myasthenic Crisis Study Group. Myasthenic crisis demanding mechanical ventilation: A multicenter analysis of 250 cases. Neurology. 2020 Jan 21:94(3):e299-e313. doi: 10.1212/WNL.0000000000008688. Epub 2019 Dec 4 [PubMed PMID: 31801833]
Level 3 (low-level) evidenceJung B, Martinez M, Claessens YE, Darmon M, Klouche K, Lautrette A, Levraut J, Maury E, Oberlin M, Terzi N, Viglino D, Yordanov Y, Claret PG, Bigé N, Société de Réanimation de Langue Française (SRLF), Société Française de Médecine d’Urgence (SFMU). Diagnosis and management of metabolic acidosis: guidelines from a French expert panel. Annals of intensive care. 2019 Aug 15:9(1):92. doi: 10.1186/s13613-019-0563-2. Epub 2019 Aug 15 [PubMed PMID: 31418093]
Cronin JN, Camporota L, Formenti F. Mechanical ventilation in COVID-19: A physiological perspective. Experimental physiology. 2022 Jul:107(7):683-693. doi: 10.1113/EP089400. Epub 2021 Sep 27 [PubMed PMID: 34541721]
Level 3 (low-level) evidenceHallett S, Toro F, Ashurst JV. Physiology, Tidal Volume. StatPearls. 2024 Jan:(): [PubMed PMID: 29494108]
Spiegel R, Hockstein M. Airway Pressure Release Ventilation: A Field Guide for the Emergency Physician. Emergency medicine clinics of North America. 2022 Aug:40(3):489-501. doi: 10.1016/j.emc.2022.05.004. Epub 2022 Jul 8 [PubMed PMID: 35953213]
Mireles-Cabodevila E, Hatipoğlu U, Chatburn RL. A rational framework for selecting modes of ventilation. Respiratory care. 2013 Feb:58(2):348-66. doi: 10.4187/respcare.01839. Epub [PubMed PMID: 22710796]
Chang HC, Ho CH, Kung SC, Chen WL, Wang CM, Cheng KC, Liu WL, Hsu HS. Maintenance of low driving pressure in patients with early acute respiratory distress syndrome significantly affects outcomes. Respiratory research. 2021 Dec 15:22(1):313. doi: 10.1186/s12931-021-01912-8. Epub 2021 Dec 15 [PubMed PMID: 34911557]
Laffey JG, O'Croinin D, McLoughlin P, Kavanagh BP. Permissive hypercapnia--role in protective lung ventilatory strategies. Intensive care medicine. 2004 Mar:30(3):347-56 [PubMed PMID: 14722644]
Girardis M, Busani S, Damiani E, Donati A, Rinaldi L, Marudi A, Morelli A, Antonelli M, Singer M. Effect of Conservative vs Conventional Oxygen Therapy on Mortality Among Patients in an Intensive Care Unit: The Oxygen-ICU Randomized Clinical Trial. JAMA. 2016 Oct 18:316(15):1583-1589. doi: 10.1001/jama.2016.11993. Epub [PubMed PMID: 27706466]
Level 1 (high-level) evidencePalmer E, Post B, Klapaukh R, Marra G, MacCallum NS, Brealey D, Ercole A, Jones A, Ashworth S, Watkinson P, Beale R, Brett SJ, Young JD, Black C, Rashan A, Martin D, Singer M, Harris S. The Association between Supraphysiologic Arterial Oxygen Levels and Mortality in Critically Ill Patients. A Multicenter Observational Cohort Study. American journal of respiratory and critical care medicine. 2019 Dec 1:200(11):1373-1380. doi: 10.1164/rccm.201904-0849OC. Epub [PubMed PMID: 31513754]
Krebs J, Pelosi P, Rocco PRM, Hagmann M, Luecke T. Positive end-expiratory pressure titrated according to respiratory system mechanics or to ARDSNetwork table did not guarantee positive end-expiratory transpulmonary pressure in acute respiratory distress syndrome. Journal of critical care. 2018 Dec:48():433-442. doi: 10.1016/j.jcrc.2018.10.005. Epub 2018 Oct 10 [PubMed PMID: 30336419]
Fredericks AS, Bunker MP, Gliga LA, Ebeling CG, Ringqvist JR, Heravi H, Manley J, Valladares J, Romito BT. Airway Pressure Release Ventilation: A Review of the Evidence, Theoretical Benefits, and Alternative Titration Strategies. Clinical medicine insights. Circulatory, respiratory and pulmonary medicine. 2020:14():1179548420903297. doi: 10.1177/1179548420903297. Epub 2020 Feb 5 [PubMed PMID: 32076372]
Zhou Y, Jin X, Lv Y, Wang P, Yang Y, Liang G, Wang B, Kang Y. Early application of airway pressure release ventilation may reduce the duration of mechanical ventilation in acute respiratory distress syndrome. Intensive care medicine. 2017 Nov:43(11):1648-1659. doi: 10.1007/s00134-017-4912-z. Epub 2017 Sep 22 [PubMed PMID: 28936695]
Kollisch-Singule M, Andrews P, Satalin J, Gatto LA, Nieman GF, Habashi NM. The time-controlled adaptive ventilation protocol: mechanistic approach to reducing ventilator-induced lung injury. European respiratory review : an official journal of the European Respiratory Society. 2019 Jun 30:28(152):. doi: 10.1183/16000617.0126-2018. Epub 2019 Apr 17 [PubMed PMID: 30996041]
Habashi NM. Other approaches to open-lung ventilation: airway pressure release ventilation. Critical care medicine. 2005 Mar:33(3 Suppl):S228-40 [PubMed PMID: 15753733]
Level 3 (low-level) evidenceFuller BM, Mohr NM, Ablordeppey E, Roman O, Mittauer D, Yan Y, Kollef MH, Carpenter CR, Roberts BW. The Practice Change and Clinical Impact of Lung-Protective Ventilation Initiated in the Emergency Department: A Secondary Analysis of Individual Patient-Level Data From Prior Clinical Trials and Cohort Studies. Critical care medicine. 2023 Feb 1:51(2):279-290. doi: 10.1097/CCM.0000000000005717. Epub 2022 Nov 14 [PubMed PMID: 36374044]
Weinberger J, Cocoros N, Klompas M. Ventilator-Associated Events: Epidemiology, Risk Factors, and Prevention. Infectious disease clinics of North America. 2021 Dec:35(4):871-899. doi: 10.1016/j.idc.2021.07.005. Epub [PubMed PMID: 34752224]
Klompas M. Ventilator-Associated Events: What They Are and What They Are Not. Respiratory care. 2019 Aug:64(8):953-961. doi: 10.4187/respcare.07059. Epub [PubMed PMID: 31346070]
Qi W, Murphy TE, Doyle MM, Ferrante LE. Association Between Daily Average of Mobility Achieved During Physical Therapy Sessions and Hospital-Acquired or Ventilator-Associated Pneumonia among Critically Ill Patients. Journal of intensive care medicine. 2023 May:38(5):418-424. doi: 10.1177/08850666221133318. Epub 2022 Oct 22 [PubMed PMID: 36278257]
Level 2 (mid-level) evidenceHassan EA, Elsaman SEA. Relationship between ventilator bundle compliance and the occurrence of ventilator-associated events: a prospective cohort study. BMC nursing. 2022 Aug 1:21(1):207. doi: 10.1186/s12912-022-00997-w. Epub 2022 Aug 1 [PubMed PMID: 35915444]
Grübler MR, Wigger O, Berger D, Blöchlinger S. Basic concepts of heart-lung interactions during mechanical ventilation. Swiss medical weekly. 2017:147():w14491. doi: 10.4414/smw.2017.14491. Epub 2017 Sep 12 [PubMed PMID: 28944931]
Sutherasan Y, Vargas M, Pelosi P. Protective mechanical ventilation in the non-injured lung: review and meta-analysis. Critical care (London, England). 2014 Mar 18:18(2):211. doi: 10.1186/cc13778. Epub 2014 Mar 18 [PubMed PMID: 24762100]
Level 3 (low-level) evidenceAcute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The New England journal of medicine. 2000 May 4:342(18):1301-8 [PubMed PMID: 10793162]
Level 1 (high-level) evidenceNeedham DM, Colantuoni E, Mendez-Tellez PA, Dinglas VD, Sevransky JE, Dennison Himmelfarb CR, Desai SV, Shanholtz C, Brower RG, Pronovost PJ. Lung protective mechanical ventilation and two year survival in patients with acute lung injury: prospective cohort study. BMJ (Clinical research ed.). 2012 Apr 5:344():e2124. doi: 10.1136/bmj.e2124. Epub 2012 Apr 5 [PubMed PMID: 22491953]
Mosier JM, Hypes C, Joshi R, Whitmore S, Parthasarathy S, Cairns CB. Ventilator Strategies and Rescue Therapies for Management of Acute Respiratory Failure in the Emergency Department. Annals of emergency medicine. 2015 Nov:66(5):529-41. doi: 10.1016/j.annemergmed.2015.04.030. Epub 2015 May 23 [PubMed PMID: 26014437]
Weingart SD. Managing Initial Mechanical Ventilation in the Emergency Department. Annals of emergency medicine. 2016 Nov:68(5):614-617. doi: 10.1016/j.annemergmed.2016.04.059. Epub 2016 Jun 9 [PubMed PMID: 27289336]
Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, Schoenfeld D, Thompson BT, National Heart, Lung, and Blood Institute ARDS Clinical Trials Network. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. The New England journal of medicine. 2004 Jul 22:351(4):327-36 [PubMed PMID: 15269312]
Level 1 (high-level) evidenceAmato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, Stewart TE, Briel M, Talmor D, Mercat A, Richard JC, Carvalho CR, Brower RG. Driving pressure and survival in the acute respiratory distress syndrome. The New England journal of medicine. 2015 Feb 19:372(8):747-55. doi: 10.1056/NEJMsa1410639. Epub [PubMed PMID: 25693014]
Level 2 (mid-level) evidenceFuchs H, Rossmann N, Schmid MB, Hoenig M, Thome U, Mayer B, Klotz D, Hummler HD. Permissive hypercapnia for severe acute respiratory distress syndrome in immunocompromised children: A single center experience. PloS one. 2017:12(6):e0179974. doi: 10.1371/journal.pone.0179974. Epub 2017 Jun 20 [PubMed PMID: 28632754]
Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators, Cavalcanti AB, Suzumura ÉA, Laranjeira LN, Paisani DM, Damiani LP, Guimarães HP, Romano ER, Regenga MM, Taniguchi LNT, Teixeira C, Pinheiro de Oliveira R, Machado FR, Diaz-Quijano FA, Filho MSA, Maia IS, Caser EB, Filho WO, Borges MC, Martins PA, Matsui M, Ospina-Tascón GA, Giancursi TS, Giraldo-Ramirez ND, Vieira SRR, Assef MDGPL, Hasan MS, Szczeklik W, Rios F, Amato MBP, Berwanger O, Ribeiro de Carvalho CR. Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on Mortality in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. JAMA. 2017 Oct 10:318(14):1335-1345. doi: 10.1001/jama.2017.14171. Epub [PubMed PMID: 28973363]
Level 3 (low-level) evidenceWriting Group for the PReVENT Investigators, Simonis FD, Serpa Neto A, Binnekade JM, Braber A, Bruin KCM, Determann RM, Goekoop GJ, Heidt J, Horn J, Innemee G, de Jonge E, Juffermans NP, Spronk PE, Steuten LM, Tuinman PR, de Wilde RBP, Vriends M, Gama de Abreu M, Pelosi P, Schultz MJ. Effect of a Low vs Intermediate Tidal Volume Strategy on Ventilator-Free Days in Intensive Care Unit Patients Without ARDS: A Randomized Clinical Trial. JAMA. 2018 Nov 13:320(18):1872-1880. doi: 10.1001/jama.2018.14280. Epub [PubMed PMID: 30357256]
Level 1 (high-level) evidenceBarr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, Davidson JE, Devlin JW, Kress JP, Joffe AM, Coursin DB, Herr DL, Tung A, Robinson BR, Fontaine DK, Ramsay MA, Riker RR, Sessler CN, Pun B, Skrobik Y, Jaeschke R, American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Critical care medicine. 2013 Jan:41(1):263-306. doi: 10.1097/CCM.0b013e3182783b72. Epub [PubMed PMID: 23269131]
Level 1 (high-level) evidenceDevlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJC, Pandharipande PP, Watson PL, Weinhouse GL, Nunnally ME, Rochwerg B, Balas MC, van den Boogaard M, Bosma KJ, Brummel NE, Chanques G, Denehy L, Drouot X, Fraser GL, Harris JE, Joffe AM, Kho ME, Kress JP, Lanphere JA, McKinley S, Neufeld KJ, Pisani MA, Payen JF, Pun BT, Puntillo KA, Riker RR, Robinson BRH, Shehabi Y, Szumita PM, Winkelman C, Centofanti JE, Price C, Nikayin S, Misak CJ, Flood PD, Kiedrowski K, Alhazzani W. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Critical care medicine. 2018 Sep:46(9):e825-e873. doi: 10.1097/CCM.0000000000003299. Epub [PubMed PMID: 30113379]
Level 1 (high-level) evidenceWang L, Li X, Yang Z, Tang X, Yuan Q, Deng L, Sun X. Semi-recumbent position versus supine position for the prevention of ventilator-associated pneumonia in adults requiring mechanical ventilation. The Cochrane database of systematic reviews. 2016 Jan 8:2016(1):CD009946. doi: 10.1002/14651858.CD009946.pub2. Epub 2016 Jan 8 [PubMed PMID: 26743945]
Level 1 (high-level) evidenceTran A, Fernando SM, Rochwerg B, Cook DJ, Crowther MA, Fowler RA, Alhazzani W, Siegal DM, Castellucci LA, Zarychanski R, English SW, Kyeremanteng K, Carrier M. Prognostic Factors Associated With Development of Venous Thromboembolism in Critically Ill Patients-A Systematic Review and Meta-Analysis. Critical care medicine. 2022 Apr 1:50(4):e370-e381. doi: 10.1097/CCM.0000000000005382. Epub [PubMed PMID: 34636806]
Level 1 (high-level) evidenceKrag M, Perner A, Wetterslev J, Wise MP, Borthwick M, Bendel S, McArthur C, Cook D, Nielsen N, Pelosi P, Keus F, Guttormsen AB, Moller AD, Møller MH, SUP-ICU co-authors. Prevalence and outcome of gastrointestinal bleeding and use of acid suppressants in acutely ill adult intensive care patients. Intensive care medicine. 2015 May:41(5):833-45. doi: 10.1007/s00134-015-3725-1. Epub 2015 Apr 10 [PubMed PMID: 25860444]
Cook DJ, Fuller HD, Guyatt GH, Marshall JC, Leasa D, Hall R, Winton TL, Rutledge F, Todd TJ, Roy P. Risk factors for gastrointestinal bleeding in critically ill patients. Canadian Critical Care Trials Group. The New England journal of medicine. 1994 Feb 10:330(6):377-81 [PubMed PMID: 8284001]
Alhazzani W, Alshamsi F, Belley-Cote E, Heels-Ansdell D, Brignardello-Petersen R, Alquraini M, Perner A, Møller MH, Krag M, Almenawer S, Rochwerg B, Dionne J, Jaeschke R, Alshahrani M, Deane A, Perri D, Thebane L, Al-Omari A, Finfer S, Cook D, Guyatt G. Efficacy and safety of stress ulcer prophylaxis in critically ill patients: a network meta-analysis of randomized trials. Intensive care medicine. 2018 Jan:44(1):1-11. doi: 10.1007/s00134-017-5005-8. Epub 2017 Dec 4 [PubMed PMID: 29199388]
Level 1 (high-level) evidenceCook D, Guyatt G. Prophylaxis against Upper Gastrointestinal Bleeding in Hospitalized Patients. The New England journal of medicine. 2018 Jun 28:378(26):2506-2516. doi: 10.1056/NEJMra1605507. Epub [PubMed PMID: 29949497]
Kollef MH. Evaluating the Value of the Respiratory Therapist: Where Is the Evidence? Focus on the Barnes-Jewish Hospital Experience. Respiratory care. 2017 Dec:62(12):1602-1610. doi: 10.4187/respcare.05807. Epub [PubMed PMID: 29162728]