Introduction
Lipofuscin is a pigmented, heterogenous byproduct of failed intracellular catabolism conventionally found within lysosomes or the cytosol of aging postmitotic cells. Although it is present in virtually any cell type, phenotypically proliferative cells often dilute its concentration to an insignificant level.[1] Hannover first discovered lipofuscin in 1842, but its progressive accumulation with age was unknown until the end of the nineteenth century.[2][3] While this historical description is still accurate, the literature of the past few decades has shifted focus towards its newly understood function as a photosensitizer of tissue and potentiator of intracellular dyshomeostasis. Because of lipofuscin’s extensively cross-linked tertiary structure and nondegradable nature, it is hypothesized to play a critical role in inhibiting proteasome function, mitophagy, autophagy, lysosomal stability, and the propagating reactive oxygen species.[1][4][5]
Lipofuscin is frequently used interchangeably with “ceroid” or “ceroid lipofuscin” as both ceroid and lipofuscin are autofluorescent intracellular accumulations of similar composition.[6] However, this may be misleading as the etymological differentiation between lipofuscin and ceroid was traditionally intended to label the former as a term associated with normal aging, and the latter for pathological conditions.[7][8][7] This distinction has become muddied as traditional lipofuscin has continued to gain attention for its risk modification effect on many diseases.[4]
Structure
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure
Its Latin namesake translates to “dark lipid,” which is only partially correct in characterizing its variable composition.[3] Lipofuscin is heterogenous amalgam mainly composed of oxidized proteins (30 to 70%) and lipids such as triglycerides, free fatty acids, cholesterol, and lipoproteins (20 to 50%). Carbohydrates make a small contribution that proportionally may increase with age (4 to 7%). This idiosyncratic composition varies amongst tissues types, but many lipofuscin researchers agree that the protein content has a significant contribution from mitochondria.[3][9][10] Jung et al. suggested that some lipofuscin aggregates’ protein source may even be up to 50% ATP synthase subunit residues in congenital ceroid lipofuscinoses.[6]
Metals such as iron, copper, zinc, aluminum, manganese, and calcium make up only 2% of lipofuscin.[11] Despite minimal contribution to lipofuscin’s total volume, iron is hypothesized to be the principal source free radicals via Fenton mechanics.[12][13]
Fluorophores are another important component of lipofuscin structure. Its 400nm to 700nm fluorescence emission spectrum is a testament to its tissue-to-tissue variability.[1][4] Cell-specific breakdown products result in a broad range of photosensitive substances, of which fluorophore A2E is of specific interest due to its supposed association with wet macular degeneration. Many phototoxic effects have been described.[1][14][15] Ultimately, these components aggregate secondary to a maladaptive intracellular environment favoring lipid peroxidation, proteasome and autophagy inhibition, and erratic polymerization of granule constituents.[4][13] The result is the formation of a nondegradable and insoluble accumulation of lipofuscin in lysosomes and cytosols. Repeat cycles of inept lysosomal autophagy and mitophagy, compounded by uncontrolled reactive oxygen species, leads to a positive feedback loop of lipofuscin buildup.[13]
The continuous net positive gain of intracellular lipofuscin can have a dramatic effect on the lysosomal structure. As seen in the work of Sitte and collaborators, progressive formation within fibroblast lysosomes and spillover into the cytoplasm can cause a toxic effect, hastening apoptosis.[16] Eventually, cellular macrostructure may become compromised due to shear lipofuscin volume. In motor neurons of humans over one hundred years of age, research shows that lipofuscin may constitute up to 75% of total cytoplasmic volume.[17] G0-phase cells such as myocytes and neurons will display the largest accumulations.[18]
Function
Outside of congenital lysosomal storage disease diagnostics, lipofuscin has no traditional histological purpose or clinical value other than indicating oxidative dyshomeostasis and aging cellular machinery. For over a century its main histological utility was the identification of cellular senescence, inversely correlating with longevity.[2][4]
As previously mentioned, recent discoveries have led to a greater understanding of lipofuscin’s function as a potentiator, rather than bystander, of apoptosis and intracellular dysregulation. While the exact details of lipofuscin’s effect on the cell are still hypothetical, there is agreement on several areas of research.[19] The most widely accepted theory of lipofuscin formation is the “mitochondrial-lysosomal axis theory of postmitotic cellular aging” proposed by Brunk and Terman: lipofuscin forms as a result of chronic lysosomal uptake of iron-rich mitochondrial breakdown products that propagate reactive oxygen species.[20][21] The subsequent lipid peroxidation breakdown products cause extensive cross-linking, preventing degradation and decreasing lysosomal stability. Sequelae include the release of toxic lipofuscin and excess iron into the cytosol, restarting the cycle as another lysosome attempts to degrade the nondegradable.[12]
There are reports of other mechanisms of collateral damage. Cross-linked lipofuscin proteins such as 4-hydroxynonenal are very weak proteasomal substrates and limit proteasome efficacy.[22] Furthermore, exposed hydrophobic residues on rich unfolded oxidized protein aggregates have been shown to attach to 20S and 26S proteasomes, inhibiting further attempts to degrade the material.[23][24] Autophagy and mitophagy gradually become impaired, allowing for a cytosolic accumulation of lipofuscin.[4][25] Because pro-apoptotic proteins like c-jun, bax, p27 do not degrade efficiently, lipofuscin correlates with increased rates of apoptosis.[4][26] Hohn et al. showed that artificial lipofuscin with increased iron stores led to increasing caspase 3 activity as well.[12] Evidence of lipofuscin's direct contribution to a negative effect on mitophagy has been highlighted by its ability to decrease PINK1 expression on senescent mitochondria, an essential protein for marking malfunctioning mitochondria. Lipofuscinogenesis also demonstrates inhibition of mitochondrial fission.[25][27]
Tissue Preparation
Lipofuscin can exist in almost any tissue; therefore tissue preparation varies significantly. Extraction for analysis is the preferred method in postmitotic cells where lipofuscin is most abundant. Traditionally, organic solvent extraction or density gradient ultracentrifugation were used to isolate lipofuscin due to its high lipid content.[4][28] However, modern analysis and quantification of lipofuscin rely on its intrinsic autofluorescence properties.[29]
Histochemistry and Cytochemistry
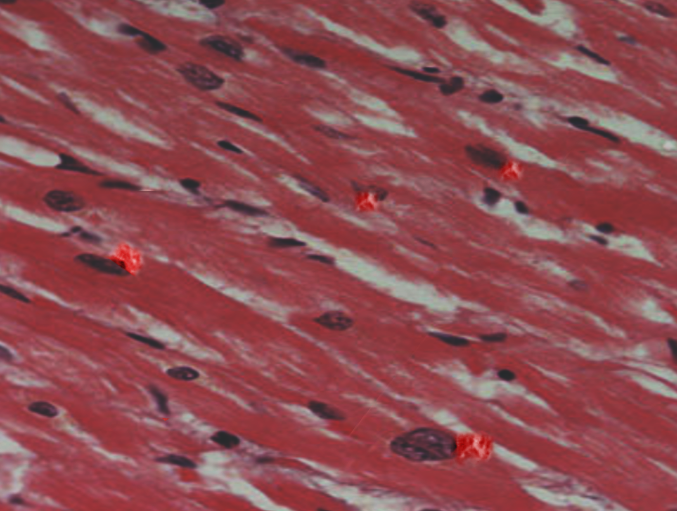
Due to its highly variable and polymeric nature, there are no antibodies specific for lipofuscin. Jung et al. pointed out that using non-overlapping antibodies and probes can be used to localize lipofuscin's fluorescence with other cellular structures of interest.[29] Many classical methods for identifying lipofuscin involved lipid and carbohydrate histochemical staining including but not limited to sudan black, Fontana-Masson, Schmorl, Ziehl-Nielson, copper sulfate, picric acid, Nile Blue, OsO4, eosin, hematoxylin, and ferric ferricyanide. Arguably, sudan black has been the most commonly used stain.[2][3][6][30]
Microscopy, Light
Both light and electron microscopy are viable methods to identify lipofuscin with or without histochemical or immunocytochemical staining; however, fluorescence microscopy is the gold standard for quantitative identification.[29] Lipofuscin can be detected within ultraviolet light (330nm to 380nm) as well as within the visible light spectrum ranging from 380nm to approximately 700nm.[1][8] Maximum fluorescence emission is around 578 nm for excitation at 364 nm.[31]
Lipofuscin granule spatial arrangement is variable, even though there may be more predictable locations per cell type. It is often free floating in the cytoplasm. With electron microscopic magnification, detailed lysosomal membranes can be easily seen surrounding the granular aggregations.[6]
Clinical Significance
The clinical significance of lipofuscin is yet to be fully elucidated despite its ubiquity in aging and a number of diseases. As discussed earlier, its hypothesized role in cellular degeneration via oxidative sequelae is likely widespread in many common pathologies; however, there are diseases in which lipofuscin accumulation is suspected to be a legitimate risk factor.
Congenital neuronal ceroid lipofuscinoses (NCLs) have the strongest evidence for the implication of lipofuscin's direct role in pathology. These early onset lysosomal storage disorders cause a massive buildup of lipofuscin visible on biopsy. With NCLs such as Batten disease and Niemann-Pick C disease, inevitable and progressive accumulation leads to cell dysfunction and death at a young age.[4][6]
Elderly patients often present with hyperpigmented macules and patches most frequently on their dorsal hands and other sun-exposed areas of the skin. These benign melanin and lipofuscin-rich areas are colloquially known as "age spots" or "liver spots," and have no clinical significance.[3] Another disease in which lipofuscin’s abundance is a clear indicator of its role in pathology is apocrine chromhidrosis, a rare disease in which the patient's sweat appears red. Identification of extensive lipofuscin granules in apocrine glands can be useful in differentiating the etiological process from toxin-induced psuedochromhidrosis and extrinsic pigment-induced eccrine chromhidrosis.[32]
The role of lipofuscin in most other pathologies are much less defined. Age-related macular degeneration’s correlation to lipofuscin accumulation has been hypothesized but remains highly controversial. Most agree that lipofuscin accumulation inhibits phagocytosis of retinal pigment epithelial cells and that its fluorophores sensitize lysosomes to the visible light spectrum, leading to cellular instability.[1][6][33] However, some studies argue that lipofuscin concentration does not correlate with the rate of macular degeneration.[34]
Lipofuscin accumulation has been observed, but not implicated, in many other common diseases found in the clinical setting. A prominent area of investigation is underway in analyzing its presence and possible role in advancing some of the most prolific age-related neurodegenerative diseases such as Alzheimer disease and Parkinson disease. Its accumulation has been noted in a number of other diseases including but not limited to atherosclerosis, Niemann-Pick disease, brown bowel syndrome, pigmented cysts, dermal hyperpigmentation, as well as numerous neoplastic processes such as pancreatic tumors, non-choroidal melanomas, and mammary gland carcinomas.[4][6]
While these pathologies may have a unique relationship with lipofuscin, it is important to keep in mind that the clinical significance of finding lipofuscin in a biopsy of the prototypical patient is limited outside of signifying cellular senescence or oxidative stress. Seeing that lipofuscin can potentially be in any cell type of any patient of older age, incidental finding on biopsy does not require further workup unless there is a specific indication.
Media
References
Brunk UT, Terman A. Lipofuscin: mechanisms of age-related accumulation and influence on cell function. Free radical biology & medicine. 2002 Sep 1:33(5):611-9 [PubMed PMID: 12208347]
Level 3 (low-level) evidenceSalmonowicz H, Passos JF. Detecting senescence: a new method for an old pigment. Aging cell. 2017 Jun:16(3):432-434. doi: 10.1111/acel.12580. Epub 2017 Feb 9 [PubMed PMID: 28185406]
Skoczyńska A, Budzisz E, Trznadel-Grodzka E, Rotsztejn H. Melanin and lipofuscin as hallmarks of skin aging. Postepy dermatologii i alergologii. 2017 Apr:34(2):97-103. doi: 10.5114/ada.2017.67070. Epub 2017 Apr 13 [PubMed PMID: 28507486]
Moreno-García A, Kun A, Calero O, Medina M, Calero M. An Overview of the Role of Lipofuscin in Age-Related Neurodegeneration. Frontiers in neuroscience. 2018:12():464. doi: 10.3389/fnins.2018.00464. Epub 2018 Jul 5 [PubMed PMID: 30026686]
Level 3 (low-level) evidenceTerman A, Brunk UT. Aging as a catabolic malfunction. The international journal of biochemistry & cell biology. 2004 Dec:36(12):2365-75 [PubMed PMID: 15325578]
Level 3 (low-level) evidenceJung T, Bader N, Grune T. Lipofuscin: formation, distribution, and metabolic consequences. Annals of the New York Academy of Sciences. 2007 Nov:1119():97-111 [PubMed PMID: 18056959]
Level 3 (low-level) evidenceSeehafer SS, Pearce DA. You say lipofuscin, we say ceroid: defining autofluorescent storage material. Neurobiology of aging. 2006 Apr:27(4):576-88 [PubMed PMID: 16455164]
Level 3 (low-level) evidenceTohma H, Hepworth AR, Shavlakadze T, Grounds MD, Arthur PG. Quantification of ceroid and lipofuscin in skeletal muscle. The journal of histochemistry and cytochemistry : official journal of the Histochemistry Society. 2011 Aug:59(8):769-79. doi: 10.1369/0022155411412185. Epub [PubMed PMID: 21804079]
Level 3 (low-level) evidenceDouble KL, Dedov VN, Fedorow H, Kettle E, Halliday GM, Garner B, Brunk UT. The comparative biology of neuromelanin and lipofuscin in the human brain. Cellular and molecular life sciences : CMLS. 2008 Jun:65(11):1669-82. doi: 10.1007/s00018-008-7581-9. Epub [PubMed PMID: 18278576]
Level 2 (mid-level) evidenceHöhn A, Grune T. Lipofuscin: formation, effects and role of macroautophagy. Redox biology. 2013 Jan 19:1(1):140-4. doi: 10.1016/j.redox.2013.01.006. Epub 2013 Jan 19 [PubMed PMID: 24024146]
Level 3 (low-level) evidenceJolly RD, Douglas BV, Davey PM, Roiri JE. Lipofuscin in bovine muscle and brain: a model for studying age pigment. Gerontology. 1995:41 Suppl 2():283-95 [PubMed PMID: 8821339]
Level 3 (low-level) evidenceHöhn A, Jung T, Grimm S, Grune T. Lipofuscin-bound iron is a major intracellular source of oxidants: role in senescent cells. Free radical biology & medicine. 2010 Apr 15:48(8):1100-8. doi: 10.1016/j.freeradbiomed.2010.01.030. Epub 2010 Jan 29 [PubMed PMID: 20116426]
Brunk UT, Terman A. The mitochondrial-lysosomal axis theory of aging: accumulation of damaged mitochondria as a result of imperfect autophagocytosis. European journal of biochemistry. 2002 Apr:269(8):1996-2002 [PubMed PMID: 11985575]
Level 3 (low-level) evidenceWinkler BS, Boulton ME, Gottsch JD, Sternberg P. Oxidative damage and age-related macular degeneration. Molecular vision. 1999 Nov 3:5():32 [PubMed PMID: 10562656]
Tonolli PN, Chiarelli-Neto O, Santacruz-Perez C, Junqueira HC, Watanabe IS, Ravagnani FG, Martins WK, Baptista MS. Lipofuscin Generated by UVA Turns Keratinocytes Photosensitive to Visible Light. The Journal of investigative dermatology. 2017 Nov:137(11):2447-2450. doi: 10.1016/j.jid.2017.06.018. Epub 2017 Jul 12 [PubMed PMID: 28711386]
Sitte N, Merker K, Grune T, von Zglinicki T. Lipofuscin accumulation in proliferating fibroblasts in vitro: an indicator of oxidative stress. Experimental gerontology. 2001 Mar:36(3):475-86 [PubMed PMID: 11250119]
Yin D, Biochemical basis of lipofuscin, ceroid, and age pigment-like fluorophores. Free radical biology [PubMed PMID: 8902532]
Level 3 (low-level) evidenceNowotny K, Jung T, Grune T, Höhn A. Accumulation of modified proteins and aggregate formation in aging. Experimental gerontology. 2014 Sep:57():122-31. doi: 10.1016/j.exger.2014.05.016. Epub 2014 May 28 [PubMed PMID: 24877899]
Level 3 (low-level) evidenceKorovila I, Hugo M, Castro JP, Weber D, Höhn A, Grune T, Jung T. Proteostasis, oxidative stress and aging. Redox biology. 2017 Oct:13():550-567. doi: 10.1016/j.redox.2017.07.008. Epub 2017 Jul 12 [PubMed PMID: 28763764]
Terman A, Gustafsson B, Brunk UT. The lysosomal-mitochondrial axis theory of postmitotic aging and cell death. Chemico-biological interactions. 2006 Oct 27:163(1-2):29-37 [PubMed PMID: 16737690]
Level 3 (low-level) evidenceTerman A, Kurz T, Navratil M, Arriaga EA, Brunk UT. Mitochondrial turnover and aging of long-lived postmitotic cells: the mitochondrial-lysosomal axis theory of aging. Antioxidants & redox signaling. 2010 Apr:12(4):503-35. doi: 10.1089/ars.2009.2598. Epub [PubMed PMID: 19650712]
Level 3 (low-level) evidenceShringarpure R, Grune T, Sitte N, Davies KJ. 4-Hydroxynonenal-modified amyloid-beta peptide inhibits the proteasome: possible importance in Alzheimer's disease. Cellular and molecular life sciences : CMLS. 2000 Nov:57(12):1802-9 [PubMed PMID: 11130184]
Reinheckel T, Ullrich O, Sitte N, Grune T. Differential impairment of 20S and 26S proteasome activities in human hematopoietic K562 cells during oxidative stress. Archives of biochemistry and biophysics. 2000 May 1:377(1):65-8 [PubMed PMID: 10775442]
Höhn A, Jung T, Grimm S, Catalgol B, Weber D, Grune T. Lipofuscin inhibits the proteasome by binding to surface motifs. Free radical biology & medicine. 2011 Mar 1:50(5):585-91. doi: 10.1016/j.freeradbiomed.2010.12.011. Epub 2010 Dec 16 [PubMed PMID: 21167934]
König J, Ott C, Hugo M, Jung T, Bulteau AL, Grune T, Höhn A. Mitochondrial contribution to lipofuscin formation. Redox biology. 2017 Apr:11():673-681. doi: 10.1016/j.redox.2017.01.017. Epub 2017 Jan 25 [PubMed PMID: 28160744]
Powell SR, Wang P, Divald A, Teichberg S, Haridas V, McCloskey TW, Davies KJ, Katzeff H. Aggregates of oxidized proteins (lipofuscin) induce apoptosis through proteasome inhibition and dysregulation of proapoptotic proteins. Free radical biology & medicine. 2005 Apr 15:38(8):1093-101 [PubMed PMID: 15780767]
Level 3 (low-level) evidenceNgo JK, Davies KJ. Importance of the lon protease in mitochondrial maintenance and the significance of declining lon in aging. Annals of the New York Academy of Sciences. 2007 Nov:1119():78-87 [PubMed PMID: 18056957]
Level 3 (low-level) evidenceSiakotos AN. Procedures for the isolation of brain lipopigments: ceroid and lipofuscin. Methods in enzymology. 1974:31():478-85 [PubMed PMID: 4419292]
Level 3 (low-level) evidenceJung T, Höhn A, Grune T. Lipofuscin: detection and quantification by microscopic techniques. Methods in molecular biology (Clifton, N.J.). 2010:594():173-93. doi: 10.1007/978-1-60761-411-1_13. Epub [PubMed PMID: 20072918]
Level 3 (low-level) evidenceTerman A, Brunk UT. Lipofuscin. The international journal of biochemistry & cell biology. 2004 Aug:36(8):1400-4 [PubMed PMID: 15147719]
Warburton S, Davis WE, Southwick K, Xin H, Woolley AT, Burton GF, Thulin CD. Proteomic and phototoxic characterization of melanolipofuscin: correlation to disease and model for its origin. Molecular vision. 2007 Mar 1:13():318-29 [PubMed PMID: 17392682]
Blalock TW, Crowson AN, Danford B. A case of generalized red sweating. Dermatology online journal. 2014 Dec 14:21(3):. pii: 13030/qt73k8k695. Epub 2014 Dec 14 [PubMed PMID: 25780968]
Level 3 (low-level) evidenceSatoh M, Yamasaki Y, Nagake Y, Kasahara J, Hashimoto M, Nakanishi N, Makino H. Oxidative stress is reduced by the long-term use of vitamin E-coated dialysis filters. Kidney international. 2001 May:59(5):1943-50 [PubMed PMID: 11318967]
Smith RT. New Understanding of Age-Related Macular Degeneration Through Quantitative Autofluorescence. JAMA ophthalmology. 2016 Jul 1:134(7):824-6. doi: 10.1001/jamaophthalmol.2016.1466. Epub [PubMed PMID: 27254789]
Level 3 (low-level) evidence