Introduction
Calcium is the most abundant cation in the human body and plays an integral role in neural transmission, enzyme activity, myocardial function, coagulation, and other cellular functions. Most of the calcium is found in the bones as calcium phosphate, whereas a small percentage is found in cells and extracellular fluids. In the serum, about 45% of calcium is bound to proteins, 45% exists as the active form of free or ionized calcium, and 10% is bound to anions. Normal calcium levels range from approximately 8.9 to 10.1 mg/dL, but this number can vary depending on the laboratory. Serum calcium levels fluctuate based on serum albumin levels, as a large percentage of calcium is bound to albumin. Therefore, calcium levels must be adjusted based on albumin levels. Hydrogen ions also bind to circulating albumin, so both acidosis and alkalosis can affect serum calcium levels. For example, increased hydrogen ions in acidosis take up additional binding sites on albumin, leading to increased free calcium levels. Thus, calcium levels should also be adjusted for serum pH.[1]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology of hypercalcemia can be divided into 2 major categories: parathyroid hormone–mediated and non-parathyroid hormone–mediated.
Parathyroid Hormone–Mediated
Primary hyperparathyroidism: This condition results in elevated levels of calcium with high or inappropriately normal parathyroid hormone levels and is typically caused by a parathyroid adenoma. Patients most commonly present with asymptomatic high-normal calcium or mild hypercalcemia. However, high levels of parathyroid hormone can also lead to severe hypercalcemia, osteoporosis, bone fractures, nephrolithiasis, and renal failure.[2]
Tertiary hyperparathyroidism: This condition also results in elevated levels of calcium and high levels of parathyroid hormone but is due to parathyroid hyperplasia from chronic overstimulation, most often in patients with renal failure or a history of renal transplant.[3]
Familial hypocalciuric hypercalcemia: This condition is caused by a loss-of-function mutation in the calcium-sensing receptor gene and is inherited in an autosomal dominant manner. This condition also results in elevated levels of calcium and parathyroid hormone but can be distinguished by the low levels of calcium in the urine.[4]
Medications can also cause hypercalcemia. Lithium use leads to hypercalcemia by altering the set point at which calcium suppresses parathyroid hormone, requiring higher levels of calcium for parathyroid hormone suppression.[5] Teriparatide is a recombinant human parathyroid hormone used to treat osteoporosis that can cause transient hypercalcemia.[6] Aboloparatide is a synthetic peptide analog of parathyroid hormone–related protein that binds to the parathyroid hormone receptor type 1, potentiating the actions of parathyroid hormone and parathyroid hormone–related protein. Consequently, it can similarly increase serum calcium levels.[7]
Non-Parathyroid Hormone-Mediated
Medication-induced: Thiazide diuretics increase calcium reabsorption in the distal convoluted tubule of the nephron, resulting in parathyroid hormone-independent hypercalcemia. These diuretics also block sodium and chloride transport, leading to increased passive absorption of sodium, water, and calcium in response to decreased arterial volume.[5] Excessive use of calcium carbonate for treating stomach reflex disease or indigestion may lead to milk-alkali syndrome, resulting in hypercalcemia, renal dysfunction, and metabolic alkalosis.[8] Prolonged use of retinoic acid causes an increase in bone resorption, which can also increase calcium levels.[9]
Hypercalcemia of malignancy: This condition is most commonly caused by excessive production of parathyroid hormone–related protein by tumors, which act on parathyroid hormone receptors due to their structural similarity. Malignancy can also cause metastatic disease to the bone and increase osteoclast activity, leading to increased bone resorption and hypercalcemia. Moreover, other malignancies, especially hematologic, such as Hodgkin or non-Hodgkin lymphoma, and granulomatous diseases, such as sarcoidosis and tuberculosis, can cause increased production of active 1,25-dihydroxy vitamin D, leading to hypercalcemia.[10] See StatPearls' companion reference, "Malignancy-Related Hypercalcemia," for more information.[11]
Vitamin D toxicity: In addition to 1,25-dihydroxy vitamin D, increased levels of 25-hydroxy vitamin D are also a major cause of hypercalcemia. Such elevation in vitamin D levels can result from excessive supplementation of vitamin D/calcitriol or excessive consumption of vitamin D-fortified dairy, which often contains calcium.
Endocrinopathies: Patients with hyperthyroidism often have increased osteoclast activity and bone resorption, leading to increased levels of both total and ionized calcium.[12] Pheochromocytoma can result in hypercalcemia either due to the presence of multiple endocrine neoplasia type 2, which is characterized by the presence of primary hyperparathyroidism, or due to a presentation similar to malignancy-related hypercalcemia in which there is an increased production of parathyroid hormone–related protein.[13] An uncommon endocrinopathy associated with hypercalcemia is adrenal insufficiency. This condition often leads to volume depletion, which results in a decreased glomerular filtration rate. In addition, it leads to increased tubular absorption, leading to hypercalcemia. Adrenal insufficiency may also contribute to increased 1,25 vitamin D, but the exact mechanisms are not known.[14]
Hypercalcemia of immobilization: Although uncommon, this is an important etiology, especially in patients with limited mobility. In these patients, an imbalance of increased osteoclast activity and decreased osteoblast activity leads to increased bone resorption and hypercalcemia.[15]
Other rare etiologies of hypercalcemia are showcased in case reports.[16]
Epidemiology
The prevalence of hypercalcemia in the general population is approximately 1% to 2%. About 90% of hypercalcemia cases are due to primary hyperparathyroidism and malignancy-associated hypercalcemia. The prevalence of primary hyperparathyroidism in the general population ranges from 0.2% to 0.8% and increases with age. Overall, 2% of all cancers are associated with hypercalcemia, but in the pediatric age group, the prevalence is less, about 0.4% to 1.3%.[17]
Pathophysiology
The 2 main regulators of calcium homeostasis in adults are parathyroid hormone and vitamin D. Parathyroid hormone functions to increase serum calcium levels by binding to osteoclasts, which increases bone resorption. In addition, it increases calcium absorption in the kidneys and facilitates the formation of active 1,25 dihydroxy-vitamin D by activating the enzyme 1-alpha-hydroxylase. This activated form of vitamin D increases intestinal absorption of calcium into the circulation.[18] Calcitonin is a hormone that lowers serum calcium levels by increasing calcium deposition in bones, inhibiting renal and intestinal absorption of calcium, and increasing urinary calcium excretion. Although calcitonin does not play a significant role in calcium homeostasis in adults, it is an important regulator in children.[19]
History and Physical
History
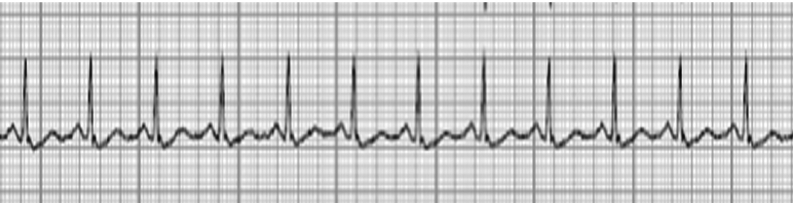
Hypercalcemia is often an incidental finding detected on labwork completed for other reasons. When calcium levels rise above 12 mg/dL, patients typically present with clinical signs and symptoms, including polyuria, polydipsia, constipation, weakness, neuropsychiatric effects, nausea, vomiting, fatigue, anorexia, and confusion. These symptoms occur mainly due to several factors, such as suppressed neural transmission, loss of the kidney's concentrating ability, other renal dysfunction, and effects on the central nervous system.[20] Cardiac tissue also relies on calcium homeostasis, and hypercalcemia can lead to shortened QT intervals, prolonged PR intervals, and widened QRS complex on electrocardiogram (ECG) (see Image. ECG Findings of Hypercalcemia). Cardiac manifestations include bradycardia, heart block, and other arrhythmias, which can be life-threatening. At severe levels, hypercalcemia can even lead to stupor or coma. Chronically high levels of hypercalcemia can also cause calcium renal stones, pancreatitis, and peptic ulcers. Patients with hypercalcemia due to hyperparathyroidism can present with fractures from osteopenia and osteoporosis. The collective symptoms of hypercalcemia are often summarized by the phrases groans, bones, stones, moans, thrones, and psychiatric overtones.
Physical Examination
Patients with hypercalcemia may have a completely normal physical examination; however, some physical examination findings are associated, including alterations in their heart rate or rhythm detectable on palpation of the pulse or cardiac auscultation. Patients can also have diminished deep tendon reflexes. A musculoskeletal examination may reveal reduced muscle tone and generalized pain. Other physical examination findings can be associated with the causative etiology.
Evaluation
Laboratory
Most cases of hypercalcemia are detected on routine testing.
Hypercalcemia can be classified into the following categories:
- Mild hypercalcemia: 10.5 to 11.9 mg/dL
- Moderate hypercalcemia: 12.0 to 13.9 mg/dL
- Hypercalcemic crisis: 14.0 to 16.0 mg/dL
Obtaining a detailed history and performing a thorough physical examination, including reviewing all medications, are crucial to determining the etiology of hypercalcemia. A key diagnostic step is checking a parathyroid hormone level to clarify if hypercalcemia is parathyroid hormone-mediated or not. The etiology of hypercalcemia can likely be obtained by history, physical examination, and laboratory investigations, but additional workup is sometimes needed.
If parathyroid hormone levels are within normal limits (but inappropriately not suppressed by hypercalcemia) or elevated, this is considered parathyroid hormone-mediated hypercalcemia. At that point, the main differentials include primary hyperparathyroidism, tertiary hyperparathyroidism, and familial hypocalciuric hypercalcemia. The next step is to conduct a 24-hour urinary calcium test to differentiate between hyperparathyroidism (associated with high levels of urinary calcium) and familial hypocalciuric hypercalcemia (associated with low levels of urinary calcium).
If parathyroid hormone levels are suppressed, then parathyroid hormone-independent etiologies of hypercalcemia should be considered, including medication-induced hypercalcemia, hypercalcemia of immobilization, underlying malignancy, granulomatous disorder, and endocrinopathies. Additional laboratory investigations to aid in the diagnosis of non-parathyroid hormone–mediated hypercalcemia may include ionized calcium, phosphorus, magnesium, alkaline phosphatase, 25-dihydroxy vitamin D, glomerular filtration rate, parathyroid hormone–related protein, serum and urine electrophoresis, thyroid panel, serum metanephrines, and insulin-like growth factor 1. Testing should be tailored to the most probable causes.
Hypercalcemia is easily diagnosed through laboratory tests, but further diagnostics often guide etiology and treatment options.
ECG: Short QT interval, low amplitude T-wave, ST-segment elevation, PR prolongation, tall and wide QRS, and arrhythmias, including bradycardia and premature ventricular contractions.
Renal ultrasound: Chronic hypercalcemia can lead to the formation of renal stones, which can be visualized on ultrasound.
Bone density scan or dual-energy X-ray absorptiometry (DEXA): This scan may reveal osteoporosis related to primary hyperparathyroidism.
Age-appropriate cancer screening: Imaging and procedural techniques such as mammogram, colonoscopy, low-dose lung computed tomography (CT) scan, and abdominal CT scan/magnetic resonance imaging (MRI) can help locate the cause of malignancy-related hypercalcemia.
Thyroid/parathyroid ultrasound: This imaging modality can detect a parathyroid adenoma if present. However, if the ultrasound is negative, additional imaging, such as a parathyroid nuclear scan or four-dimensional parathyroid CT scan, may be needed.
Treatment / Management
The goals of treating hypercalcemia include increased elimination from the extracellular fluid, reduced gastrointestinal absorption, and decreased bone resorption. Treatment options differ based on the etiology and severity of hypercalcemia.
Hydration: Patients with hypercalcemia can become volume-depleted and require intravenous (IV) hydration. Hydration is typically accomplished with a 0.9% saline infusion until the patient has an adequate urine output and becomes euvolemic.[21]
Electrolyte replacement: Hypercalcemia can often present with other electrolytic abnormalities such as hypokalemia, hypomagnesemia, and hypophosphatemia. These abnormalities should all be appropriately repleted to maintain normal levels.
Calcitonin: Calcitonin can be administered as an intramuscular or subcutaneous injection at a dose of 4 units/kg every 12 hours to acutely lower calcium levels. This hormone is effective as quickly as 2 hours after administration, but its effect only lasts approximately 4 to 7 days, limiting its use in chronic therapy. Calcitonin is often combined with other calcium-lowering modalities to maintain low levels of calcium.[22]
Bisphosphonates: Both pamidronate and zoledronic acid are approved for treating hypercalcemia of malignancy; however, zoledronic acid is shown to be more effective. These medications typically take approximately 3 days to lower calcium levels back to the normal range. They are often administered simultaneously with hydration and calcitonin so that these agents can lower calcium levels acutely while waiting for the bisphosphonates to be effective.[23]
Denosumab: This monoclonal antibody binds to the RANK ligand and inhibits osteoclasts. Denosumab is considered the first-line treatment for hypercalcemia of malignancy, along with bisphosphonates and hydration. This medication is a great treatment option for patients who have renal impairment and is shown to be very effective in lowering calcium levels.[23][24](A1)
Parathyroidectomy: When the etiology of hypercalcemia is primary hyperparathyroidism, the patient should be evaluated to determine whether they meet the surgical criteria for a parathyroidectomy. These criteria include serum calcium greater than 1.0 mg/dL above the upper limit of normal, evidence of osteoporosis on DEXA scan, fragility or vertebral fracture, 24-hour urine calcium greater than 400 mg/d, presence of renal stones, or age less than 50.[25] If these criteria are met, the patients should pursue a parathyroidectomy to reduce calcium levels for a more long-term approach.[26](A1)
Cinacelcet: Cinacelcet is a calcimimetic medication that is currently approved by the Food and Drug Administration for treating secondary hyperparathyroidism due to renal failure. This medication is also used in patients with primary hyperparathyroidism who are not candidates for surgery and has recently been reported in case studies as a treatment for hypercalcemia of malignancy.[27] Cinacelcet works by increasing the sensitivity of the calcium-sensing receptors on the surface of the parathyroid cells, resulting in decreased parathyroid hormone release.[27]
Renal replacement therapy: This treatment, completed with a low- or no-calcium bath, is typically reserved for patients with severe hypercalcemia and renal failure or those who are unable to tolerate IV hydration.
Glucocorticoids: In cases where hypercalcemia is due to lymphoma or granulomatous diseases, oral prednisone (20-40 mg daily) inhibits calcitriol production and lowers calcium levels.[23]
Gallium nitrate: Similar to bisphosphonates, gallium nitrate inhibits osteoclasts but can lead to nephrotoxicity and further electrolyte abnormalities; therefore, it has been withdrawn from the market.
Mithramycin: This medication rapidly inhibits osteoclast RNA synthesis but is both hepatotoxic and nephrotoxic, so it is also often avoided.
Ketoconazole: As an antifungal agent, ketoconazole inhibits 1-alpha-hydroxylase in macrophages and lowers levels of active vitamin D.[28][29]
Treatment of underlying disease: As the etiology of hypercalcemia is very broad, in addition to the acute treatment of hypercalcemia, and to achieve more long-term results, it is also imperative to identify and treat the underlying condition causing the hypercalcemia.
Differential Diagnosis
Although hypercalcemia can present with various symptoms, the most common complaints include dehydration and polyuria.
Dehydration
Dehydrated patients can show higher levels of serum calcium due to hemoconcentration. The history often reveals a decreased fluid intake, but additional signs, such as dry mouth, dry skin, reduced skin turgor, tachycardia, hypotension, and reduced urine output, should be evaluated. Dehydration must be corrected with oral or IV hydration to help improve and normalize the calcium levels.
Polyuria
If a patient presents with polyuria, several differentials need to be considered. Patients with uncontrolled diabetes mellitus often have polyuria due to the osmotic effects of hyperglycemia. In addition, patients with diabetes insipidus (central or nephrogenic) can have polyuria due to water diuresis and hypernatremia. Patients presenting with acute polyuria may also have a urinary tract infection or hypokalemia.
Prognosis
The prognosis of hypercalcemia is largely dependent on its etiology. Many processes causing hypercalcemia are benign and have simple treatment options that lead to a good prognosis, such as medication-induced hypercalcemia and primary hyperparathyroidism. When hypercalcemia is due to malignancy or granulomatous disorders, the prognosis may be very poor. Therefore, this is another reason why not only diagnosing hypercalcemia but also determining its etiology is crucial for its proper management.
Complications
The complications of hypercalcemia include the following:
- Depression
- Kidney stones
- Bone pain
- Constipation
- Pancreatitis
- Renal failure
- Gastric ulcers
- Paresthesias
- Syncope and arrhythmias
- Altered mental status
Deterrence and Patient Education
The management of hypercalcemia involves both evidence-based medical interventions and a focused diagnostic approach to ensure cost-effective, patient-centered care. Lifestyle modifications and dietary adjustments are often necessary to prevent worsening of hypercalcemia, necessitating patient education, potentially involving physicians or dietitians. Effective communication between interdisciplinary teams and the patient is crucial for including the patient in all treatment options and allowing for autonomy.
Pearls and Other Issues
In addition to treatment, follow-up becomes equally important and care must be coordinated to ensure effective long-term management of the patient's condition. Educating the patient on the importance of follow-up and the consequences of uncontrolled disease is necessary to ensure patient safety and improve patient outcomes. Patients should be advised to stay well hydrated to prevent worsening of calcium levels.
Key information to keep in mind when dealing with hypercalcemia is to determine the etiology. Treatment options can differ tremendously based on the underlying condition, so choosing the correct therapy involves a comprehensive history, physical, and additional investigations. One of the pitfalls in assessing hypercalcemia is that cases of mild hypercalcemia can be overlooked, especially if patients remain asymptomatic. It is imperative that cases of persistent hypercalcemia, even if mild, be investigated further.
Enhancing Healthcare Team Outcomes
Patients often discover they have hypercalcemia either through routine lab tests or due to symptoms. Early identification and subsequent management can result in decreased morbidity and mortality associated with hypercalcemia. The etiologies of hypercalcemia are abundant, often requiring a collaborative effort among various healthcare professionals to diagnose and treat accurately. Primary care or family physicians are typically the first-line health professionals involved, as hypercalcemia is often found during routine blood work and checkups. Other specialists, such as endocrinologists and nephrologists, may also identify the problem during their routine checkups of patients. Pharmacists are essential in identifying medication-induced hypercalcemia. When patients are inpatient, nurses and ancillary staff play a crucial role in obtaining laboratory results, administering prompt treatment, and monitoring for adverse effects of medications at the bedside. In outpatient settings, other staff members may be involved in administering infusions or securing insurance approvals.
In addition, patients and their families need to be involved in outpatient management to monitor for potential symptoms and ensure medication compliance. In cases of hypercalcemia due to immobilization, physical and occupational therapy teams are crucial to ensure adequate movement and hydration. When hypercalcemia is associated with malignancy, the prognosis is guarded, and patients may transition to palliative or hospice care.
Media
(Click Image to Enlarge)
References
Blaine J, Chonchol M, Levi M. Renal control of calcium, phosphate, and magnesium homeostasis. Clinical journal of the American Society of Nephrology : CJASN. 2015 Jul 7:10(7):1257-72. doi: 10.2215/CJN.09750913. Epub 2014 Oct 6 [PubMed PMID: 25287933]
Level 3 (low-level) evidenceWalker MD, Silverberg SJ. Primary hyperparathyroidism. Nature reviews. Endocrinology. 2018 Feb:14(2):115-125. doi: 10.1038/nrendo.2017.104. Epub 2017 Sep 8 [PubMed PMID: 28885621]
Zhang LX, Zhang B, Liu XY, Wang ZM, Qi P, Zhang TY, Zhang Q. Advances in the treatment of secondary and tertiary hyperparathyroidism. Frontiers in endocrinology. 2022:13():1059828. doi: 10.3389/fendo.2022.1059828. Epub 2022 Dec 6 [PubMed PMID: 36561571]
Level 2 (mid-level) evidenceVarghese J, Rich T, Jimenez C. Benign familial hypocalciuric hypercalcemia. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2011 Mar-Apr:17 Suppl 1():13-7. doi: 10.4158/EP10308.RA. Epub [PubMed PMID: 21478088]
McHenry CR, Lee K. Lithium therapy and disorders of the parathyroid glands. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 1996 Mar-Apr:2(2):103-9 [PubMed PMID: 15251551]
Milosavljevic J, Thomas AM. Teriparatide Associated Late Hypercalcemia: A Report of Two Cases and Literature Review. Journal of community hospital internal medicine perspectives. 2022:12(1):54-58. doi: 10.55729/2000-9666.1010. Epub 2022 Jan 31 [PubMed PMID: 35711860]
Level 3 (low-level) evidenceArdura JA, Portal-Núñez S, Alonso V, Bravo B, Gortazar AR. Handling Parathormone Receptor Type 1 in Skeletal Diseases: Realities and Expectations of Abaloparatide. Trends in endocrinology and metabolism: TEM. 2019 Oct:30(10):756-766. doi: 10.1016/j.tem.2019.07.014. Epub 2019 Aug 11 [PubMed PMID: 31409530]
Medarov BI. Milk-alkali syndrome. Mayo Clinic proceedings. 2009 Mar:84(3):261-7. doi: 10.4065/84.3.261. Epub [PubMed PMID: 19252114]
Hammoud D, El Haddad B, Abdallah J. Hypercalcaemia secondary to hypervitaminosis a in a patient with chronic renal failure. The West Indian medical journal. 2014 Jan:63(1):105-8. doi: 10.7727/wimj.2011.171. Epub 2014 Jan 3 [PubMed PMID: 25303202]
Guise TA, Wysolmerski JJ. Cancer-Associated Hypercalcemia. The New England journal of medicine. 2022 Apr 14:386(15):1443-1451. doi: 10.1056/NEJMcp2113128. Epub [PubMed PMID: 35417639]
Vakiti A, Anastasopoulou C, Mewawalla P. Malignancy-Related Hypercalcemia. StatPearls. 2024 Jan:(): [PubMed PMID: 29494030]
Burman KD, Monchik JM, Earll JM, Wartofsky L. Ionized and total serum calcium and parathyroid hormone in hyperthyroidism. Annals of internal medicine. 1976 Jun:84(6):668-71 [PubMed PMID: 937877]
Mune T, Katakami H, Kato Y, Yasuda K, Matsukura S, Miura K. Production and secretion of parathyroid hormone-related protein in pheochromocytoma: participation of an alpha-adrenergic mechanism. The Journal of clinical endocrinology and metabolism. 1993 Mar:76(3):757-62 [PubMed PMID: 8383146]
De Silva SDN, Aravinthan M, Katulanda P. Glucocorticoid-induced adrenal insufficiency: an uncommon cause of hypercalcaemia. Endocrinology, diabetes & metabolism case reports. 2022 May 1:2022():. pii: 21-0177. doi: 10.1530/EDM-21-0177. Epub 2022 May 1 [PubMed PMID: 35510507]
Level 3 (low-level) evidenceCano-Torres EA, González-Cantú A, Hinojosa-Garza G, Castilleja-Leal F. Immobilization induced hypercalcemia. Clinical cases in mineral and bone metabolism : the official journal of the Italian Society of Osteoporosis, Mineral Metabolism, and Skeletal Diseases. 2016 Jan-Apr:13(1):46-7. doi: 10.11138/ccmbm/2016.13.1.046. Epub 2016 May 11 [PubMed PMID: 27252745]
Level 3 (low-level) evidenceMotlaghzadeh Y, Bilezikian JP, Sellmeyer DE. Rare Causes of Hypercalcemia: 2021 Update. The Journal of clinical endocrinology and metabolism. 2021 Oct 21:106(11):3113-3128. doi: 10.1210/clinem/dgab504. Epub [PubMed PMID: 34240162]
Catalano A, Chilà D, Bellone F, Nicocia G, Martino G, Loddo I, Morabito N, Benvenga S, Loddo S. Incidence of hypocalcemia and hypercalcemia in hospitalized patients: Is it changing? Journal of clinical & translational endocrinology. 2018 Sep:13():9-13. doi: 10.1016/j.jcte.2018.05.004. Epub 2018 May 29 [PubMed PMID: 30023309]
Nussbaum SR. Pathophysiology and management of severe hypercalcemia. Endocrinology and metabolism clinics of North America. 1993 Jun:22(2):343-62 [PubMed PMID: 8325291]
Yu E, Sharma S. Physiology, Calcium. StatPearls. 2024 Jan:(): [PubMed PMID: 29489276]
Ralston SH, Coleman R, Fraser WD, Gallagher SJ, Hosking DJ, Iqbal JS, McCloskey E, Sampson D. Medical management of hypercalcemia. Calcified tissue international. 2004 Jan:74(1):1-11 [PubMed PMID: 14523593]
Tonon CR, Silva TAAL, Pereira FWL, Queiroz DAR, Junior ELF, Martins D, Azevedo PS, Okoshi MP, Zornoff LAM, de Paiva SAR, Minicucci MF, Polegato BF. A Review of Current Clinical Concepts in the Pathophysiology, Etiology, Diagnosis, and Management of Hypercalcemia. Medical science monitor : international medical journal of experimental and clinical research. 2022 Feb 26:28():e935821. doi: 10.12659/MSM.935821. Epub 2022 Feb 26 [PubMed PMID: 35217631]
Wisneski LA. Salmon calcitonin in the acute management of hypercalcemia. Calcified tissue international. 1990:46 Suppl():S26-30 [PubMed PMID: 2137363]
Minisola S, Pepe J, Piemonte S, Cipriani C. The diagnosis and management of hypercalcaemia. BMJ (Clinical research ed.). 2015 Jun 2:350():h2723. doi: 10.1136/bmj.h2723. Epub 2015 Jun 2 [PubMed PMID: 26037642]
El-Hajj Fuleihan G, Clines GA, Hu MI, Marcocci C, Murad MH, Piggott T, Van Poznak C, Wu JY, Drake MT. Treatment of Hypercalcemia of Malignancy in Adults: An Endocrine Society Clinical Practice Guideline. The Journal of clinical endocrinology and metabolism. 2023 Feb 15:108(3):507-528. doi: 10.1210/clinem/dgac621. Epub [PubMed PMID: 36545746]
Level 1 (high-level) evidenceBilezikian JP, Khan AA, Silverberg SJ, Fuleihan GE, Marcocci C, Minisola S, Perrier N, Sitges-Serra A, Thakker RV, Guyatt G, Mannstadt M, Potts JT, Clarke BL, Brandi ML, International Workshop on Primary Hyperparathyroidism. Evaluation and Management of Primary Hyperparathyroidism: Summary Statement and Guidelines from the Fifth International Workshop. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research. 2022 Nov:37(11):2293-2314. doi: 10.1002/jbmr.4677. Epub 2022 Oct 17 [PubMed PMID: 36245251]
Level 1 (high-level) evidenceWilhelm SM, Wang TS, Ruan DT, Lee JA, Asa SL, Duh QY, Doherty GM, Herrera MF, Pasieka JL, Perrier ND, Silverberg SJ, Solórzano CC, Sturgeon C, Tublin ME, Udelsman R, Carty SE. The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA surgery. 2016 Oct 1:151(10):959-968. doi: 10.1001/jamasurg.2016.2310. Epub [PubMed PMID: 27532368]
O'Callaghan S, Yau H. Treatment of malignancy-associated hypercalcemia with cinacalcet: a paradigm shift. Endocrine connections. 2021 Jan:10(1):R13-R24. doi: 10.1530/EC-20-0487. Epub [PubMed PMID: 33289687]
Conron M, Beynon HL. Ketoconazole for the treatment of refractory hypercalcemic sarcoidosis. Sarcoidosis, vasculitis, and diffuse lung diseases : official journal of WASOG. 2000 Oct:17(3):277-80 [PubMed PMID: 11033844]
Walker MD, Shane E. Hypercalcemia: A Review. JAMA. 2022 Oct 25:328(16):1624-1636. doi: 10.1001/jama.2022.18331. Epub [PubMed PMID: 36282253]