Introduction
The globus pallidus (GP) is one of the components of the basal ganglia. It divides into globus pallidus internus (GPi) and globus pallidus externus (GPe). The globus pallidus and putamen collectively form the lentiform (lenticular) nucleus, which lies beneath the insula. The caudate nucleus and putamen form the corpus striatum. The corpus striatum is also an important part of the basal ganglia. The thalamus, subthalamus, and substantia nigra (SN) are not a part of the basal ganglia but serve essential functions for the network.
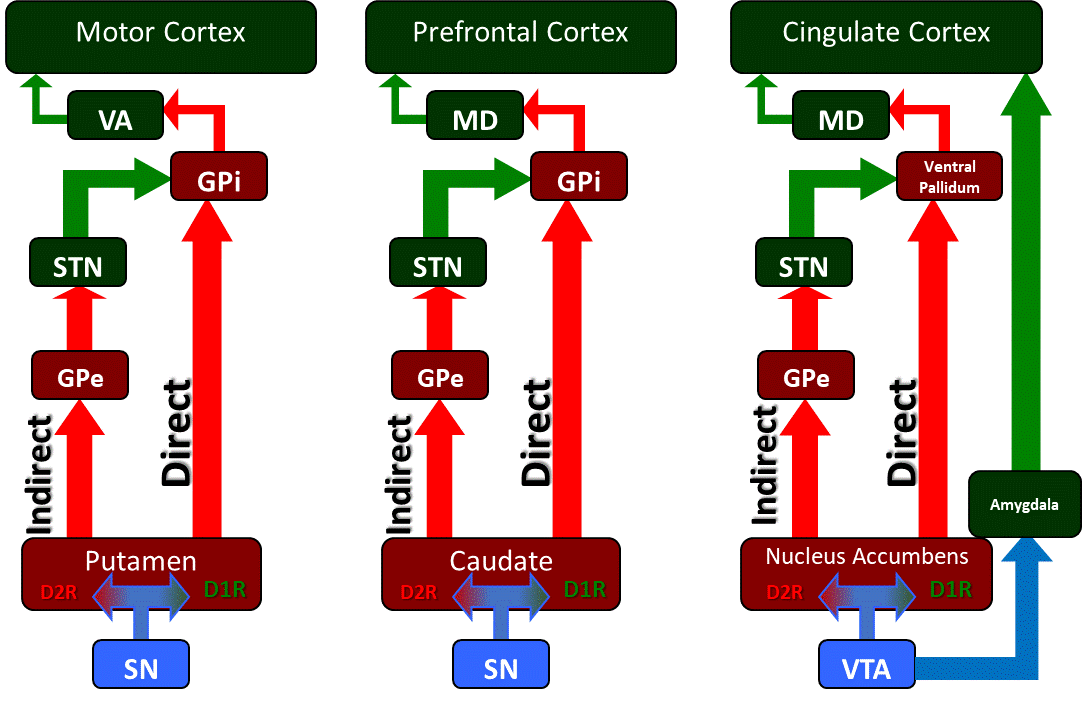
The motor system controlled by basal ganglia is made of corticobulbar and subcortical structures, the gray matter of the spinal cord, cerebellum, and efferent nerves. The basal ganglia coordinate with other structures in the brain to plan and implement goal-oriented behaviors. This coordination requires multiple striatal (motor), cognitive, and limbic (reward) circuits and pathways. The globus pallidus can modulate these pathways because of its connections. The major output of the striatum is through the GPe. The GPi acts as the final output for both direct and indirect pathways of the basal ganglia network. The thalamus, however, is slightly different. It acts as a relay because of its reciprocal interconnections with cortical and subcortical structures. Therefore, the thalamus can perform multiple motor and sensory functions. These unique characteristics enable each component to work effectively.
The dysfunction of the GP has been noted in ischemia, alcohol, and opiate abuse. This dysfunction gives rise to various cognitive and motor problems.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The globus pallidus (GP) is a subcortical structure of the brain. It is a triangular mass of cells located medial to the putamen. Its name originates from the Latin 'pale globe,' owing to its pale appearance due to the myelinated axons that make up the structure; this contrasts with the neighboring unmyelinated structures (putamen and striatum), which appear darker. The medial medullary lamina of the white matter divides the GP into globus pallidus internus (GPi) and globus pallidus externus (GPe).[1] The GPi is the medial subdivision, whereas GPe is the lateral subdivision. The GPe is relatively larger than the GPi. It is also located caudomedially to the corpus striatum.[2]
The globus pallidus, putamen, and caudate nucleus are intimately related to the lateral ventricles. The caudate nucleus lies directly laterally adjacent and nestled within the concave contour of the lateral ventricle, whereas the putamen lies inferior and within the concavity of the head and body of the caudate nucleus. The globus pallidus lies at the medial aspect of the putamen, bordered further medially by the curve of the internal capsule (best appreciated in an axial section).
The primary function of the globus pallidus is to control conscious and proprioceptive movements. The GPe is the intrinsic nucleus, whereas the GPi is the output nucleus. The intrinsic nucleus acts as a relay for information. The output nucleus primarily sends information to the thalamus.[3] To perform its function effectively, the GP receives input from multiple structures. The GP receives most of the inhibitory input (GABAergic) from the striatum. It is important to note that substantia nigra pars compacta (SNPc) has projections to the striatum. These projections secrete dopamine to target either D1 or D2 receptors present on the striatum. D1 receptors are excitatory (glutamatergic) in nature, whereas D2 receptors are inhibitory in nature.[4] Some inhibitory input (GABAergic) also comes from the caudate and putamen. The output is computed through the direct and indirect pathways.
Direct pathway
The 'direct pathway' promotes movement. The SNPc excites the striatum by secreting dopamine (nigrostriatal projections) to activate the D1 striatal receptors. The excited D1 receptors activate the striatum, sending more inhibitory signals to the GPi. A few inhibitory signals transmit simultaneously to the substantia nigra pars reticularis (SNPr). As a result, the GPi and SNPr experience inhibition. The GPi and SNPr lose their inhibitory influence on the thalamic nuclei (ventral anterior thalamic nucleus and ventral lateral thalamic nucleus). This loss of influence means that the thalamic nuclei are no longer inhibited and can send excitatory signals to the motor cortex via corticospinal projections. Ultimately, the excitation of the motor cortex allows the required movement to occur. It is important to note that GPi secretes an opiate known as substance-P, which may regulate the nigrostriatal pathway.[5]
Indirect pathway
The 'indirect pathway' limits motor function so that excessive and erratic movements do not occur. The SNPc inhibits the striatum by secreting dopamine (nigrostriatal projections) to activate D2 striatal receptors, which means that the inhibited D2 receptors send fewer inhibitory signals to GPe. The GPe is in a relatively excited state. Therefore, it sends more inhibitory signals to the subthalamic nucleus. The inhibited subthalamic nucleus can no longer inhibit the GPi and the SNPr. The GPi and the SNPr are, therefore, able to inhibit the thalamic nuclei. Ultimately, the thalamic nuclei inhibit movement. In recent experiments, it has been elucidated that the GPe secretes an opiate called enkephalin.[6] This opiate can modulate the nigrostriatal pathway.[7]
These pathways, therefore, explain how the GPe and the GPi differ in their functions.
Embryology
Human brain development begins during the third week of gestation from the ectoderm. The notochord induces neurulation, a process by which the ectoderm above the notochord forms neuroectoderm to give rise to other structures. As a result, the neural tube begins to form. The brain continues to develop from the neural tube. Following the closure of this neural tube by week 6, the primary brain vesicles form. These primary brain vesicles include the prosencephalon (forebrain), mesencephalon (midbrain), and rhombencephalon (hindbrain).[8] These primitive brain vesicles continue to differentiate into different structures. In the fifth week of gestation, the prosencephalon develops into the telencephalon and the diencephalon. The telencephalon gives rise to most of the components of the basal ganglia, which includes the caudate and the putamen.[9] The globus pallidus originates from neuroblasts in the wall of the 3rd ventricle of the diencephalon.
Blood Supply and Lymphatics
The GP receives its blood supply from the anterior choroidal artery (AChA), middle cerebral artery (MCA), and anterior cerebral artery (ACA). The MCA provides the majority of the blood supply. The perforating branches of the ACA supply the anterior and inferior portions of the GP. The perforating arteries from the MCA perfuse the majority of the superior and posterior portions of the lateral section of the GP. Heubner’s artery (which arises from the A1 or A2 segment of the ACA or at the junction of the ACA with the anterior communicating artery) and the ACA also supply a small portion of the lateral segment of the GP.[10] The AChA perfuses the medial portion of the GP.[11]
The venous drainage of the GP derives from veins that drain the adjacent basal ganglia, particularly caudate and putamen. The system forms from a deep and ventricular group of veins. The deep group subdivides into a group of inferior striate veins that drain the putamen and caudate nuclei. The deep group of veins joins the deep middle cerebral and basal veins. The ventricular group of veins drains the caudate nucleus. The ventricular group joins the internal cerebral and basal veins.[12] The basal and internal cerebral veins join to form the great vein of Galen, which then drains into the straight sinus.
The GP, as a part of the basal ganglia, has a similar lymphatic drainage system as the cerebral cortex. The lymphatic system of the cerebral cortex forms from perivascular, cerebrospinal fluid (CSF), and olfactory drainage pathways, as well as meningeal lymphatic vessels.[13][14] However, a study mentions that the perivascular spaces in the basal ganglia and cerebral cortex are structurally different. This difference is partly responsible for the difference in fluid composition between the two.[15]
Nerves
The globus pallidus, being a part of the basal ganglia, plays an additional role in higher cognitive functions such as reinforcement and memory building. The nuclei (including GP) and cortical areas interconnect via independent parallel loop circuits. The association and limbic cortices project to specific striatal domains, which, in turn, project back to the corresponding cortical areas via the globus pallidus and the thalamus. There have also been suggestions that the location of both the GP and substantia nigra helps transmit information from the limbic to the associative system.[16]
Physiologic Variants
Studies have elucidated gender and differences in the volume of the basal ganglia structures, in keeping with similar studies of cortical structures showing such differences.[17] Specifically, with respect to the globus pallidus, imaging studies have demonstrated that it is larger in males compared to females after adjustment for measurements of overall cortical size, whereas the opposite is true for the caudate nucleus.[18] Indeed the general trend from imaging studies is that females have larger subcortical volumes than men.[19] Furthermore, there appears to be interindividual variability between hemispheres concerning the volume of the globus pallidus. Neuroimaging studies found that the left GP is significantly larger in volume than the right GP.[19][20]
Surgical Considerations
The GPi has implications in the surgical procedures involving deep brain stimulation (DBS) for treating dystonia in disorders like Wilson disease to improve quality of life.[21][22] A study noted that the DBS of bilateral GPi could be an effective treatment for dystonia due to the GNAL mutation, especially in patients unresponsive to medication or botulinum toxin.[23] With depression being among the most common non-motor symptoms of Parkinson disease, some investigators have reviewed the evidence to determine if there is a difference in mood effects (depression) after the DBS of either GPi or the subthalamic nucleus. However, their review found no clear benefit of targeting either the STN or the GPi.[24]
Since GPi is the principal striatal output circuit, it has seen significant use in ablative surgery for various neuropsychiatric disorders. GPi surgery has long been the target for treating hyperkinetic and hypokinetic movement disorders, including behavioral disorders such as Tourette syndrome. Pallidotomy was a surgical intervention for Huntington disease and Parkinson disease (PD). However, pallidotomy was abandoned in the mid-20th century as a treatment for PD.
Clinical Significance
Studies have demonstrated the involvement of GPi in different disorders, such as obsessive-compulsive disorders (OCD), Tourette’s syndrome, acquired dystonia, and attention deficit hyperactivity disorder (ADHD). Alterations in the resting-state functional connectivity of the cortico-striatal circuits have been implicated in OCD. Indeed, recent studies have noted increased resting-state functional connectivity between the left GPe and the left STN. This increased connectivity was also present between the left GPe and the left GPi. The involvement of these structures in the pathophysiology provides evidence for success in DBS targeted at GPi.[25]
The GP also has implications for parkinsonian motor symptoms. Studies have elucidated that dopamine depletion leads to excessive stimulation (increase in the firing rate) of the GPi neurons causing parkinsonian motor symptoms, as evidenced by increased activity of GPi in PD.[26] Other studies of the PD model have also shown that the loss of striatal dopaminergic activity leads to the disinhibition of the D2-striatal projection neurons, which causes increased inhibition of the GPe.[26] The inhibition of GPe, in turn, causes the disinhibition of the subthalamic nucleus, which results in the downregulation of autonomous firing in the STN neurons. Additionally, neuroimaging studies of patients with Huntington’s disease have reported a severe decrease in the size of the GP.[27]
Unlike the putamen and caudate, the GP is spared from ischemic injury after a hypoxic-ischemic insult. There are also case reports of bilateral GP lesions following alcohol and opiate abuse.[28] Since the GP is a critical structure in the basal ganglia circuits, its understanding is essential to gain a better understanding of motor and non-motor dysfunctions of the circuits.
Media
(Click Image to Enlarge)
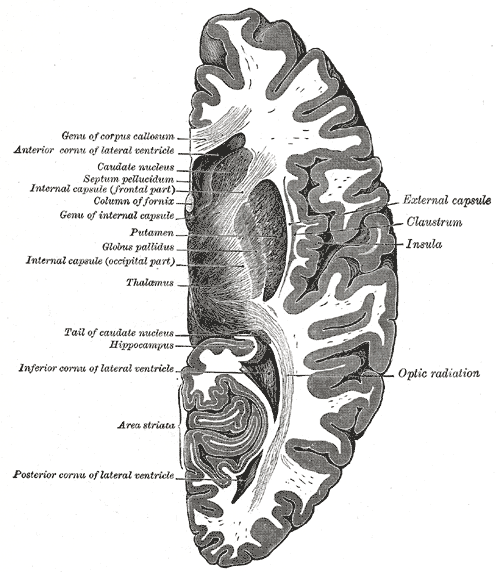
Horizontal Section of the Right Cerebral Hemisphere. Genu of corpus callosum, anterior cornua of lateral ventricle, caudate nucleus, septum pellucidum, internal capsule (frontal part), column of fornix, genu of internal capsule, putamen, globus pallidus, internal capsule (occipital part), thalamus, tail of caudate nucleus, hippocampus, inferior cornua of lateral ventricle, area striata, posterior cornua of lateral ventricle, optic radiation, insula, claustrum, and the external capsule.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
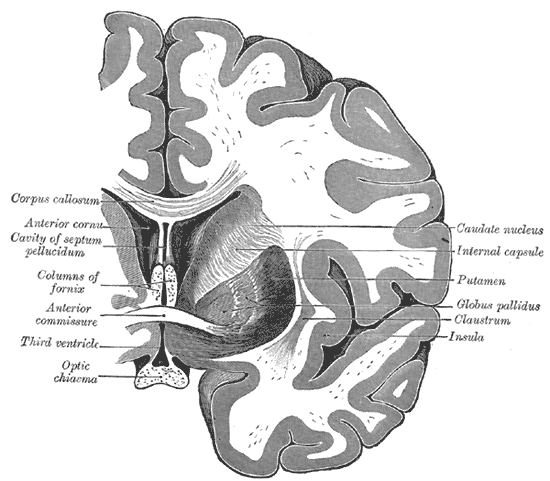
Coronal section of the Brain Through the Anterior Commissure. The caudate nucleus, internal capsule, putamen, globus pallidus, claustrum, insula, optic chiasma, third ventricle, anterior commissure, columns of fornix, cavity of septum pellucidum, anterior cornu, and the corpus callosum.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
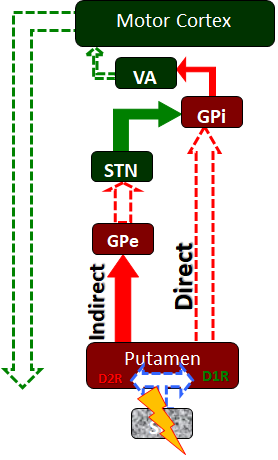
The basal ganglia circuitry as it is affected in Parkinson's disease. Neurodegenerative loss of the substantia nigra (SN) and its dopaminergic projections to the putamen lead to a decrease in activity in the direct pathway and an increase in activity in the indirect pathway. As a result, the subthalamic nucleus (STN) disproportionately stimulates the globus pallidus internus (GPi) which in turn inhibits the ventral anterior (VA) nucleus of the thalamus and a loss of activitation of the motor cortex and its corticospinal projections to the spinal cord alpha motor neurons. These patients experience deficits in the initiation of motor movement along with poor balance control and changes in gait, along with other signs and symptoms. Contributed by James W. H. Sonne, PhD
References
Ide S, Kakeda S, Yoneda T, Moriya J, Watanabe K, Ogasawara A, Futatsuya K, Ohnari N, Sato T, Hiai Y, Matsuyama A, Fujiwara H, Hisaoka M, Korogi Y. Internal Structures of the Globus Pallidus in Patients with Parkinson's Disease: Evaluation with Phase Difference-enhanced Imaging. Magnetic resonance in medical sciences : MRMS : an official journal of Japan Society of Magnetic Resonance in Medicine. 2017 Oct 10:16(4):304-310. doi: 10.2463/mrms.mp.2015-0091. Epub 2016 Dec 22 [PubMed PMID: 28003623]
Kita H. Globus pallidus external segment. Progress in brain research. 2007:160():111-33 [PubMed PMID: 17499111]
Level 3 (low-level) evidenceLanciego JL, Luquin N, Obeso JA. Functional neuroanatomy of the basal ganglia. Cold Spring Harbor perspectives in medicine. 2012 Dec 1:2(12):a009621. doi: 10.1101/cshperspect.a009621. Epub 2012 Dec 1 [PubMed PMID: 23071379]
Level 3 (low-level) evidenceVoytek B, Emergent basal ganglia pathology within computational models. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2006 Jul 12; [PubMed PMID: 16838428]
Level 3 (low-level) evidenceSong DD, Harlan RE. The development of enkephalin and substance P neurons in the basal ganglia: insights into neostriatal compartments and the extended amygdala. Brain research. Developmental brain research. 1994 Dec 16:83(2):247-61 [PubMed PMID: 7535204]
Level 3 (low-level) evidenceLo DC, Hughes RE, Paulson HL, Albin RL. Huntington’s Disease: Clinical Features and Routes to Therapy. Neurobiology of Huntington's Disease: Applications to Drug Discovery. 2011:(): [PubMed PMID: 21882418]
Steiner H, Gerfen CR. Role of dynorphin and enkephalin in the regulation of striatal output pathways and behavior. Experimental brain research. 1998 Nov:123(1-2):60-76 [PubMed PMID: 9835393]
Level 3 (low-level) evidenceAbuHasan Q, Reddy V, Siddiqui W. Neuroanatomy, Amygdala. StatPearls. 2023 Jan:(): [PubMed PMID: 30725787]
Fazl A, Fleisher J. Anatomy, Physiology, and Clinical Syndromes of the Basal Ganglia: A Brief Review. Seminars in pediatric neurology. 2018 Apr:25():2-9. doi: 10.1016/j.spen.2017.12.005. Epub 2017 Dec 27 [PubMed PMID: 29735113]
Vasović L, Ugrenović S, Jovanović I. Human fetal medial striate artery or artery of Heubner. Journal of neurosurgery. Pediatrics. 2009 Apr:3(4):296-301. doi: 10.3171/2008.12.PEDS08258. Epub [PubMed PMID: 19338407]
Djulejić V, Marinković S, Georgievski B, Stijak L, Aksić M, Puškaš L, Milić I. Clinical significance of blood supply to the internal capsule and basal ganglia. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2016 Mar:25():19-26. doi: 10.1016/j.jocn.2015.04.034. Epub 2015 Nov 16 [PubMed PMID: 26596401]
Ribas EC, Yağmurlu K, de Oliveira E, Ribas GC, Rhoton A. Microsurgical anatomy of the central core of the brain. Journal of neurosurgery. 2018 Sep:129(3):752-769. doi: 10.3171/2017.5.JNS162897. Epub 2017 Dec 22 [PubMed PMID: 29271710]
Da Mesquita S, Fu Z, Kipnis J. The Meningeal Lymphatic System: A New Player in Neurophysiology. Neuron. 2018 Oct 24:100(2):375-388. doi: 10.1016/j.neuron.2018.09.022. Epub [PubMed PMID: 30359603]
Sun BL, Wang LH, Yang T, Sun JY, Mao LL, Yang MF, Yuan H, Colvin RA, Yang XY. Lymphatic drainage system of the brain: A novel target for intervention of neurological diseases. Progress in neurobiology. 2018 Apr-May:163-164():118-143. doi: 10.1016/j.pneurobio.2017.08.007. Epub 2017 Sep 10 [PubMed PMID: 28903061]
Naganawa S, Nakane T, Kawai H, Taoka T. Differences in Signal Intensity and Enhancement on MR Images of the Perivascular Spaces in the Basal Ganglia versus Those in White Matter. Magnetic resonance in medical sciences : MRMS : an official journal of Japan Society of Magnetic Resonance in Medicine. 2018 Oct 10:17(4):301-307. doi: 10.2463/mrms.mp.2017-0137. Epub 2018 Jan 18 [PubMed PMID: 29343658]
Miyachi S. [Cortico-basal ganglia circuits--parallel closed loops and convergent/divergent connections]. Brain and nerve = Shinkei kenkyu no shinpo. 2009 Apr:61(4):351-9 [PubMed PMID: 19378804]
Level 3 (low-level) evidenceCarne RP, Vogrin S, Litewka L, Cook MJ. Cerebral cortex: an MRI-based study of volume and variance with age and sex. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2006 Jan:13(1):60-72 [PubMed PMID: 16410199]
Giedd JN, Snell JW, Lange N, Rajapakse JC, Casey BJ, Kozuch PL, Vaituzis AC, Vauss YC, Hamburger SD, Kaysen D, Rapoport JL. Quantitative magnetic resonance imaging of human brain development: ages 4-18. Cerebral cortex (New York, N.Y. : 1991). 1996 Jul-Aug:6(4):551-60 [PubMed PMID: 8670681]
Level 3 (low-level) evidenceSzabó CA, Lancaster JL, Xiong J, Cook C, Fox P. MR imaging volumetry of subcortical structures and cerebellar hemispheres in normal persons. AJNR. American journal of neuroradiology. 2003 Apr:24(4):644-7 [PubMed PMID: 12695196]
Murphy DG, DeCarli C, Schapiro MB, Rapoport SI, Horwitz B. Age-related differences in volumes of subcortical nuclei, brain matter, and cerebrospinal fluid in healthy men as measured with magnetic resonance imaging. Archives of neurology. 1992 Aug:49(8):839-45 [PubMed PMID: 1343082]
Cury RG, Kalia SK, Shah BB, Jimenez-Shahed J, Prashanth LK, Moro E. Surgical treatment of dystonia. Expert review of neurotherapeutics. 2018 Jun:18(6):477-492. doi: 10.1080/14737175.2018.1478288. Epub 2018 May 28 [PubMed PMID: 29781334]
Hedera P. Treatment of Wilson's disease motor complications with deep brain stimulation. Annals of the New York Academy of Sciences. 2014 May:1315():16-23. doi: 10.1111/nyas.12372. Epub 2014 Feb 18 [PubMed PMID: 24547944]
Ahn JH, Kim AR, Kim NKD, Park WY, Kim JS, Kim M, Park J, Lee JI, Cho JW, Cho KR, Youn J. The Effect of Globus Pallidus Interna Deep Brain Stimulation on a Dystonia Patient with the GNAL Mutation Compared to Patients with DYT1 and DYT6. Journal of movement disorders. 2019 May:12(2):120-124. doi: 10.14802/jmd.19006. Epub 2019 May 30 [PubMed PMID: 31158945]
Combs HL, Folley BS, Berry DT, Segerstrom SC, Han DY, Anderson-Mooney AJ, Walls BD, van Horne C. Cognition and Depression Following Deep Brain Stimulation of the Subthalamic Nucleus and Globus Pallidus Pars Internus in Parkinson's Disease: A Meta-Analysis. Neuropsychology review. 2015 Dec:25(4):439-54. doi: 10.1007/s11065-015-9302-0. Epub 2015 Oct 12 [PubMed PMID: 26459361]
Level 1 (high-level) evidenceAzriel A, Farrand S, Di Biase M, Zalesky A, Lui E, Desmond P, Evans A, Awad M, Moscovici S, Velakoulis D, Bittar RG. Tractography-Guided Deep Brain Stimulation of the Anteromedial Globus Pallidus Internus for Refractory Obsessive-Compulsive Disorder: Case Report. Neurosurgery. 2020 Jun 1:86(6):E558-E563. doi: 10.1093/neuros/nyz285. Epub [PubMed PMID: 31313803]
Level 3 (low-level) evidenceOertel W, Schulz JB. Current and experimental treatments of Parkinson disease: A guide for neuroscientists. Journal of neurochemistry. 2016 Oct:139 Suppl 1():325-337. doi: 10.1111/jnc.13750. Epub 2016 Aug 30 [PubMed PMID: 27577098]
Syka M, Keller J, Klempíř J, Rulseh AM, Roth J, Jech R, Vorisek I, Vymazal J. Correlation between relaxometry and diffusion tensor imaging in the globus pallidus of Huntington's disease patients. PloS one. 2015:10(3):e0118907. doi: 10.1371/journal.pone.0118907. Epub 2015 Mar 17 [PubMed PMID: 25781024]
Alquist CR, McGoey R, Bastian F, Newman W 3rd. Bilateral globus pallidus lesions. The Journal of the Louisiana State Medical Society : official organ of the Louisiana State Medical Society. 2012 May-Jun:164(3):145-6 [PubMed PMID: 22866355]
Level 3 (low-level) evidence