Introduction
Agenesis of corpus callosum (ACC) [OMIM 217990] is one of the most common congenital cerebral malformations, which is morphologically the complete or partial absence of corpus callosum and is not defined by functional or behavioral abnormalities (as in autism).
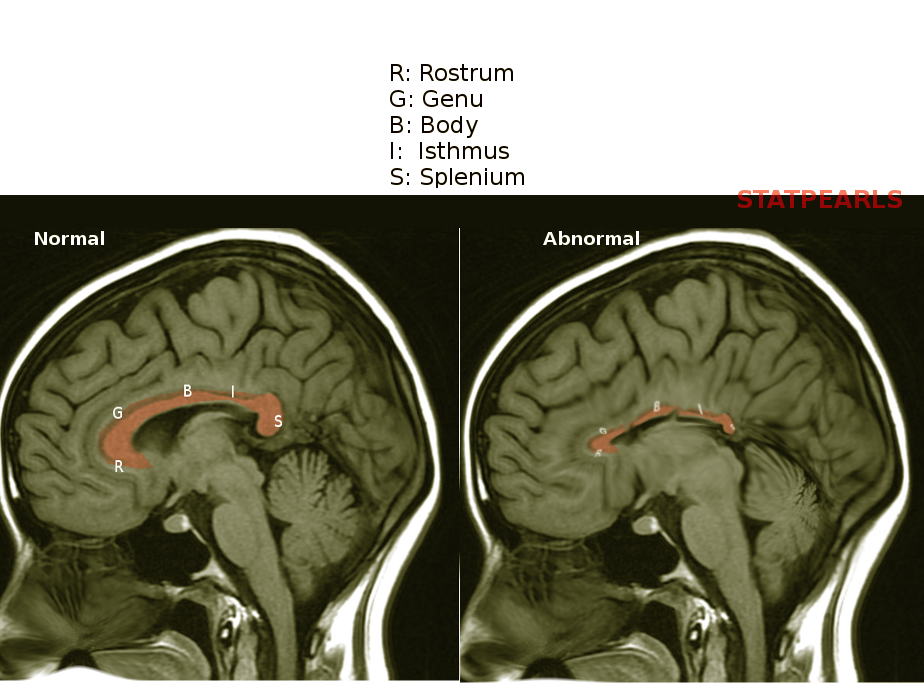
The corpus callosum is the largest white matter structure, containing 200 million axons [1] connecting the two hemispheres of the brain. Its formation starts by 74 days of gestation, with the first fibers crossing the midline at 11 to 12 weeks of gestation, development completed by 115 days, and the basic shape assumed by 18 to 20 weeks of gestational age.[2] The formation is primarily from anterior to posterior, starting with the genu and finishing with the rostrum.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Agenesis of the corpus callosum can present as an isolated condition or associated with other cerebral abnormalities. Several factors have correlations with the etiology of agenesis of the corpus callosum[3][4][1][5]:
- Maternal alcohol use during pregnancy
- Maternal phenylketonuria
- Chiari II malformation
- Genetic factors: Agenesis of the corpus callosum often correlates with several aneuploidy and non-aneuploidy syndromes. Chromosomal abnormalities are present in 20% of ACC, especially trisomies 18 and 13.
- Syndromes that include agenesis of the corpus callosum as an associated feature:
- Autosomal-dominant - e.g., Apert syndrome and basal cell nevus syndrome, Mowat-Wilson syndrome
- Autosomal-recessive - e.g., Joubert syndrome and Lyon syndrome
- X-linked - e.g., Aicardi syndrome and X-linked aqueductal stenosis or hydrocephalus
- Chromosomal rearrangements - e.g. trisomies, del(4)(p16), del(6)(q23), dup(8)(p21p23), dup(11)(q23qter)
- Mutations in the disrupted-in-schizophrenia 1 (DISC1) gene located at 1q42.1 have been recently described to be associated with agenesis of the corpus callosum.
- Syndromes that include agenesis of the corpus callosum as an associated feature:
Epidemiology
Agenesis of the corpus callosum is one of the most common human brain malformations. It has an incidence of 0.5 to 70 in 10000, and its prevalence in children with developmental disabilities is about 230 in 10000 (2.3%).[6] It presents in 1 in 19000 autopsies.[7][8] Agenesis of the corpus callosum is more prevalent among males than females.[9]
Pathophysiology
Research has not yet determined the precise mechanism underlying the isolated occurrence of agenesis of the corpus callosum. It is an abnormality of prosencephalic midline development, and there are more than 200 congenital syndromes associated with ACC.
Histopathology
Depending on the part of the corpus callosum affected, agenesis of the corpus callosum may be classified into one of two varieties:
- Complete agenesis
- Partial agenesis (hypogenesis or dysgenesis), in which usually the splenium (the posterior part) is absent.
As a rule of thumb, primary agenesis of the corpus callosum (total agenesis) can be excluded by the presence of the rostrum. One exception is holoprosencephaly. In this condition, there may be atypical callosal dysgenesis, in which anterior parts of the corpus callosum are absent.
The other developmental abnormalities of the corpus callosum include:
- Dysgenesis - Abnormal shape
- Hypoplasia - Decreased thickness
Morphologically, agenesis of the corpus callosum is classified into two types:
- Type 1 - Axons form, but these are unable to cross the midline. Hence, they form large aberrant Probst bundle fibers along the medial hemispheric walls.
- Type 2 - Commissural axons fail to form, so Probst fiber bundles are not found.
Probst fiber bundles run parallel to the medial walls of the lateral ventricles and enlarge and deform their medial borders, especially at the level of the frontal horns. Recently, a reduction in the number of von Economo neurons, which are large spindle-shaped neurons localized to the anterior cingulate cortex and frontoinsular cortex, has been described in agenesis of the corpus callosum. Partial agenesis of the corpus callosum has correlations with 'sigmoid bundles,' which asymmetrically connect the frontal lobe with the contralateral occipitoparietal cortex.[10]
History and Physical
The affected patients are mostly asymptomatic. Most of the patients present within the first two years of life.
The core syndrome of primary agenesis of corpus callosum consists of the following symptoms[11]:
- Reduction in the interhemispheric transfer of sensory-motor information
- Delay in cognitive processing and
- Decrease in the complex information analysis and unacquainted task performance: increased vulnerability to elevation in cognitive demands.
Patients with agenesis of corpus callosum usually present with:
- Mental retardation (60%)
- Vision problems (33%)
- Delay in the development of speech (29%)
- Seizures (25%)
- Feeding problems (20%)
- Impaired hand-eye coordination and
- Socio-behavioral disorders like attention-deficit-hyperactivity disorder (ADHD) and psychosis
Isolated agenesis of corpus callosum patients may have normal intelligence quotient but may have some cognitive deficits, which group under the "core syndrome," which includes[11]:
- Reduced interhemispheric transfer of sensory-motor information
- Reduced cognitive processing speed
- Deficits in complex reasoning and novel problem-solving
Evaluation
Fetal ultrasound can detect agenesis of the corpus callosum as early as the 16th week of gestation.[2] However, it is associated with a false-positive rate of 0 to 20%.[12]
An antenatal ultrasound scan may show some findings suggestive of agenesis of the corpus callosum:
- Dilated and elevated third ventricle
- Lateral ventricles may appear as widely spaced parallel bodies with small frontal horns
- Colpocephaly gives rise to a "teardrop" configuration on axial scans.
- Absent septum pellucidum with widened interhemispheric fissure
- Color Doppler may show that the normal semicircular arterial loop, formed by the pericallosal artery, along with the superior surface of the corpus callosum, is missing or distorted.
Magnetic resonance imaging of the brain is the investigation of choice for agenesis of the corpus callosum.
The following signs are suggestive of the diagnosis[13][14]:
- Racing car sign: Axial imaging of the lateral ventricles will show the similarity to a Formula One car viewed from above
- "Moose head appearance" or "Viking helmet sign" or "Longhorn appearance": Coronal views at the level of the frontal horns have this characteristic appearance due to CCA and eversion of bilateral cingulate gyri into the frontal horns
- Sunray appearance: Sagittal imaging shows gyri radiating outward in a radial pattern from the ventricle
- Lateral ventricles appear to be parallel to each other and non-converging
- ACC is also typically accompanied by colpocephaly (dilatation of the trigones and occipital horns)
- High-riding third ventricle
- Along the superomedial surface of lateral ventricles, inverted Probst bundles may be present.
Neuropsychological evaluation of all patients with agenesis of the corpus callosum is mandatory.
Treatment / Management
Treatment is mainly symptomatic and supportive.
The main line of treatment includes:
- Antiepileptic medications
- Special education
- Physiotherapy
- Ventriculoperitoneal shunt if hydrocephalus is present
- Genetic counseling to family members
- Surgeries for associated syndromic morphological abnormalities
- Speech and visual rehabilitation
- Psychological and psychiatric therapies as appropriate
Differential Diagnosis
The primary imaging differential diagnoses are holoprosencephaly and septo-optic dysplasia.
The main feature that helps to differentiate between the absence of septum pellucidum and agenesis of the corpus callosum is the presence of fused or communicating frontal horns and of the corpus callosum.(which may sometimes appear thinned).
The presence of fused frontal horns, an abnormal anterior cerebral artery (azygos anterior cerebral artery), and the absence of a normally developed interhemispheric fissure anteriorly in holoprosencephaly assist in differentiating it from isolated and complete agenesis of the corpus callosum.
Midline interhemispheric cysts may also be associated with agenesis of the corpus callosum. The differential diagnosis of such cysts are:
- Cavum septum pellucidum
- Cavum vergae
- Cavum velum interpositum and
- Interhemispheric arachnoid cyst
Sometimes, these conditions can cause difficulty in diagnosis as a dilated third ventricle with a dorsal cyst can also appear the same. However, the presence of a choroid plexus in the roof of the third ventricle helps in differentiating the latter.
Prognosis
The prognosis is determined primarily by the associated malformations.
Agenesis of the corpus callosum is associated with the following intracranial anomalies (in decreasing order of frequency)[15]:
- Interhemispheric cyst with hydrocephalus
- Dandy-Walker malformation
- Neuronal migration disorder
- Agenesis of the inferior vermis
- Encephalocele
- Lipoma of the interhemispheric fissure
Children with isolated agenesis of the corpus callosum without any significant neurologic sequelae have the best prognosis.
Children with agenesis of corpus callosum associated with the neuronal migration disorder with or without Dandy-Walker malformation have the worst prognosis.
Complications
Complications are more likely to occur due to the associated disorders. Some of these include:
- Aspiration pneumonia
- Seizures
- Schizophrenia and
- Cerebral palsy
Deterrence and Patient Education
Patients with developmental delays and intellectual disabilities may benefit from early intervention services, special education, and other supportive therapies.
Enhancing Healthcare Team Outcomes
An interprofessional approach involves the obstetrician for the antenatal care of the mother, neonatologist, pediatric neurologist, pediatric neurosurgeon, geneticist, maxillofacial surgeon, ophthalmologist, otorhinolaryngologist, plastic surgeon, pediatric psychiatrist and psychologist, dietician, and pediatric neuro nurse, working collaboratively in an interprofessional team approach can help to provide a good outcome for the patient with agenesis of the corpus callosum.
Media
References
Schell-Apacik CC, Wagner K, Bihler M, Ertl-Wagner B, Heinrich U, Klopocki E, Kalscheuer VM, Muenke M, von Voss H. Agenesis and dysgenesis of the corpus callosum: clinical, genetic and neuroimaging findings in a series of 41 patients. American journal of medical genetics. Part A. 2008 Oct 1:146A(19):2501-11. doi: 10.1002/ajmg.a.32476. Epub [PubMed PMID: 18792984]
Kaplan P. X linked recessive inheritance of agenesis of the corpus callosum. Journal of medical genetics. 1983 Apr:20(2):122-4 [PubMed PMID: 6682447]
Level 3 (low-level) evidenceSowell ER, Mattson SN, Thompson PM, Jernigan TL, Riley EP, Toga AW. Mapping callosal morphology and cognitive correlates: effects of heavy prenatal alcohol exposure. Neurology. 2001 Jul 24:57(2):235-44 [PubMed PMID: 11468307]
Levy HL, Lobbregt D, Barnes PD, Poussaint TY. Maternal phenylketonuria: magnetic resonance imaging of the brain in offspring. The Journal of pediatrics. 1996 Jun:128(6):770-5 [PubMed PMID: 8648535]
Level 3 (low-level) evidenceOsbun N, Li J, O'Driscoll MC, Strominger Z, Wakahiro M, Rider E, Bukshpun P, Boland E, Spurrell CH, Schackwitz W, Pennacchio LA, Dobyns WB, Black GC, Sherr EH. Genetic and functional analyses identify DISC1 as a novel callosal agenesis candidate gene. American journal of medical genetics. Part A. 2011 Aug:155A(8):1865-76. doi: 10.1002/ajmg.a.34081. Epub 2011 Jul 7 [PubMed PMID: 21739582]
Level 3 (low-level) evidenceJeret JS, Serur D, Wisniewski K, Fisch C. Frequency of agenesis of the corpus callosum in the developmentally disabled population as determined by computerized tomography. Pediatric neuroscience. 1985-1986:12(2):101-3 [PubMed PMID: 2428024]
Grogono JL. Children with agenesis of the corpus callosum. Developmental medicine and child neurology. 1968 Oct:10(5):613-6 [PubMed PMID: 5304353]
Freytag E, Lindenberg R. Neuropathologic findings in patients of a hospital for the mentally deficient. A survey of 359 cases. The Johns Hopkins medical journal. 1967 Dec:121(6):379-92 [PubMed PMID: 4228863]
Level 3 (low-level) evidenceNagwa S, Saran S, Sharma Y, Kharbanda A. Imaging features of complete agenesis of corpus callosum in a 3-year-old child. Sudanese journal of paediatrics. 2018:18(2):69-71. doi: 10.24911/SJP.106-1523336915. Epub [PubMed PMID: 30799905]
Tovar-Moll F, Moll J, de Oliveira-Souza R, Bramati I, Andreiuolo PA, Lent R. Neuroplasticity in human callosal dysgenesis: a diffusion tensor imaging study. Cerebral cortex (New York, N.Y. : 1991). 2007 Mar:17(3):531-41 [PubMed PMID: 16627861]
Brown WS, Paul LK. The Neuropsychological Syndrome of Agenesis of the Corpus Callosum. Journal of the International Neuropsychological Society : JINS. 2019 Mar:25(3):324-330. doi: 10.1017/S135561771800111X. Epub 2019 Jan 29 [PubMed PMID: 30691545]
Santo S, D'Antonio F, Homfray T, Rich P, Pilu G, Bhide A, Thilaganathan B, Papageorghiou AT. Counseling in fetal medicine: agenesis of the corpus callosum. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2012 Nov:40(5):513-21. doi: 10.1002/uog.12315. Epub [PubMed PMID: 23024003]
Level 1 (high-level) evidenceCherian EV, Shenoy KV, Bukelo MJ, Thomas DA. Racing car brings tear drops in the moose. BMJ case reports. 2013 Feb 21:2013():. doi: 10.1136/bcr-2012-008165. Epub 2013 Feb 21 [PubMed PMID: 23436891]
Level 3 (low-level) evidenceKazi AZ, Joshi PC, Kelkar AB, Mahajan MS, Ghawate AS. MRI evaluation of pathologies affecting the corpus callosum: A pictorial essay. The Indian journal of radiology & imaging. 2013 Oct:23(4):321-32. doi: 10.4103/0971-3026.125604. Epub [PubMed PMID: 24604936]
Singh S, Garge S. Agenesis of the corpus callosum. Journal of pediatric neurosciences. 2010 Jan:5(1):83-5. doi: 10.4103/1817-1745.66662. Epub [PubMed PMID: 21042520]