Introduction
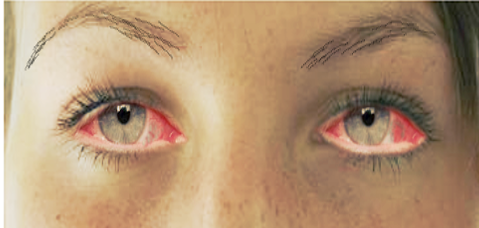
Conjunctivitis is one of the most common causes of red-eye and affects patients of all ages and socioeconomic class. Viral conjunctivitis is responsible for the majority of infectious conjunctivitis, accounting for up to 75% of cases. [1][2] Characteristics of viral conjunctivitis include redness, blood vessel engorgement, ocular discharge, pain, photophobia, and pseudomembranes. There is a considerable economic and societal impact due to the costs of visits to the emergency department or general practitioner, diagnostic tests, prescription treatment, and time lost from work or school. Prescribing antibiotics in cases of viral conjunctivitis is one of the major costs of any healthcare system. The rates of antibiotic treatment in the community for patients with infectious conjunctivitis in the United Kingdom range between 80% and 95%.[3][4] Improvement in diagnostic rates of viral conjunctivitis is estimated to have reduced inappropriate antibiotic prescribing and saved US $430 million per year in the United States.[2] Specific treatments for viral conjunctivitis are currently being assessed in clinical trials. Due to the non-specificity of signs and symptoms, a thorough medical and ophthalmic history with clinical examination should be obtained, especially in patients with atypical signs and a chronic course.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The conjunctiva is a thin semitransparent membrane that covers the white part of the eye called the sclera. The conjunctiva starts at the limbus of the cornea and covers both the sclera and posterior surface of the eyelids. The portion covering the scleral is referred to as the bulbar conjunctiva, and the portion on the posterior surface of the lids is the palpebral conjunctiva.
The most common cause of viral conjunctivitis is adenoviruses. The adenovirus is part of the Adenoviridae family that consists of a nonenveloped, double-stranded DNA virus. Frequently associated infections caused by the adenovirus include upper respiratory tract infections, eye infections, and diarrhea in children. Children are most susceptible to viral infections, and adults tend to get more bacterial infections. Viral conjunctivitis can be obtained by direct contact with the virus, airborne transmission, and reservoir such as swimming pools. [5][6]
Most cases of viral conjunctivitis are highly contagious for 10-14 days. Washing hands and avoidance of eye contact are key to preventing transmission to others.
Adenoviral Conjunctivitis
Up to 90% of viral conjunctivitis cases are caused by adenoviruses.[7] In children pharyngoconjunctival fever (PCF) due to HAdV types 3, 4, and 7 results in acute follicular conjunctivitis with fever, pharyngitis, periauricular lymphadenopathy. Epidemic keratoconjunctivitis (EKC) is the most severe ocular infection caused by adenovirus and is classically associated with serotypes 8, 19, and 37. The cornea can be affected by the viral replication in the epithelium and anterior stroma leading to superficial punctate keratopathy and subepithelial infiltrates.[8] Monotherapy with povidone-iodine 2% have demonstrated the resolution of symptoms.[9] Further combinations of povidone-iodine with corticosteroids are undergoing phase 3 randomized controlled studies. Visual symptoms caused by subepithelial infiltrates can be debilitating and the use of tacrolimus, 1% and 2% cyclosporine A eye drops have been shown to effective.[10][11][12]
Herpetic Conjunctivitis
Herpes conjunctivitis is common in adults and children and associated with follicular conjunctivitis. Herpes simplex virus (HSV) is estimated to be responsible for 1.3 - 4.8% of acute conjunctivitis cases.[13] Treatment with topical antiviral agents is aimed at reducing virus shedding and the development of keratitis. Varicella-zoster can cause conjunctivitis either by direct contact of the eye or skin lesions or inhalation of infected aerosolized particles, especially with the involvement of the first and second branches of the trigeminal nerve.
Acute Hemorrhagic Conjunctivitis (AHC)
This is a very contagious form of viral conjunctivitis and symptoms include foreign body sensation, epiphora, eyelid edema, conjunctival chemosis, and subconjunctival hemorrhage. A small proportion of patients experience systemic symptoms of fever, fatigue, limb pain. Transmission is primarily via hand to eye contact and fomites.[14] Picornaviruses EV70 and coxsackievirus A24 variant (CA24v) are thought to be the responsible pathogens.[15]
COVID-19 Conjunctivitis
The most recent isolated strain of coronavirus, COVID-19 has been reported to cause conjunctivitis along with fever, cough, respiratory distress, and death.[16] Retrospective and prospective studies show that 1% to 6% of patients display COVID-19 related conjunctivitis, with conjunctival swabs being positive in 2.5% of cases.[17] Transmission through ocular tissues is incompletely understood. Ophthalmologists are at higher risk for COVID-19 infection due to the close proximity to patients, equipment intense clinics, direct contact with patients' conjunctival mucosal surfaces, and high-volume clinics. Systemic COVID-19 is contracted through direct or airborne inhalation of respiratory droplets. Additional protective measures such as social distancing, wearing masks, reduced clinic volumes, and sterilization of surfaces should be practiced to reduce transmission risk.
Epidemiology
Conjunctivitis, whether bacterial or viral, is a common problem that affects millions of Americans each year. In the United States, it is estimated that 1% of visits of a primary care physicians are related to conjunctivitis. While viral conjunctivitis is the most common cause, bacterial conjunctivitis is the second most common cause and distinguishing the two can be a challenge for primary care physicians. Frequently antibiotics are prescribed without good indication which could present an unnecessary financial burden on the patient and increase drug-resistant bacteria. Employers and schools typically require those with conjunctivitis to remain out of their locations until the infection clears, potentially adding to the economic burden placed on those infected.[18]
Pathophysiology
Regardless of the etiology, most cases of conjunctivitis can be categorized as either papillary or follicular. Neither classification is pathognomonic for a particular disease entity. Papillary conjunctivitis produces a cobblestone arrangement of flattened nodules with central vascular cores. It is most commonly associated with an allergic immune response or is a response to a foreign body. Independent of the etiology, the histologic appearance of papillary conjunctivitis is the same: closely packed, flat-topped projections, with numerous eosinophils, lymphocytes, plasma cells, and mast cells in the stroma surrounding a central vascular channel.
Follicular conjunctivitis is seen in a variety of conditions, including inflammation caused by pathogens such as viruses, bacteria, toxins, and topical medications. In contrast to papillae, follicles are small, dome-shaped nodules without a prominent central vessel. Histologically, a lymphoid follicle is situated in the subepithelial region and consists of a germinal center with immature, proliferating lymphocytes surrounded by a ring of mature lymphocytes and plasma cells. The follicles in follicular conjunctivitis are typically most prominent in the inferior palpebral and forniceal conjunctiva.[19]
History and Physical
The diagnosis of viral conjunctivitis is based on clinical and laboratory signs. Correct and early identification of etiology allows appropriate treatment and the avoidance of longer-term complications.
Patients with viral conjunctivitis present with sudden onset foreign body sensation, red eyes, itching, light sensitivity, burning, and watery discharge. Whereas with bacterial conjunctivitis, patients present with all the above symptoms, but with mucopurulent discharge and mattering of the eyelids upon waking. Those presenting with viral conjunctivitis usually have a recent history of upper respiratory tract infection or recent contact with a sick individual. Visual acuity is usually at or near their baseline vision. The cornea can have subepithelial infiltrates that can decrease the vision and cause light sensitivity. The conjunctiva is injected (red) and can also be edematous. In some cases, a membrane or pseudomembrane can be appreciated in the tarsal conjunctiva. These are sheets of fibrin-rich exudates that are devoid of blood or lymphatic vessels. True membranes can lead to the development of subepithelial fibrosis and symblepharon, and also bleed heavily on removal.[20] Follicles, small, dome-shaped nodules without a prominent central vessel, can be seen on the palpebral conjunctiva. The majority of viral conjunctivitis patients will have follicles present, but the presence of papillae does not rule out a viral etiology.[21] Palpation of the preauricular lymph nodes may reveal a reactive lymph node that is tender to the touch and will help differentiate viral conjunctivitis versus bacterial. With HSV, vesicles may appear on the face or eyelids and vision may be affected. Corneal involvement may occur. With herpes zoster, there is a linear dermatomal pattern of vesicles. The conjunctiva is often red with a mucopurulent discharge.
Fever, malaise, fatigue, presence of enlarged lymph nodes, and other constitutional signs help to differentiate viral conjunctivitis from other causes. Anisocoria and photophobia are associated with serious eye conditions including anterior uveitis, keratitis, and scleritis.[22] Systemic diseases associated with conjunctivitis include skin and mucous membrane diseases (acne rosacea, ichthyosis, xeroderma pigmentosum), collagen vascular diseases (systemic lupus erythematosus, rheumatoid arthritis, Sjogren's disease, granulomatosis with polyangiitis), and autoimmunity (graft versus host disease, Steven-Johnson syndrome, and ocular cicatricial pemphigoid).
Evaluation
Laboratory testing is typically not indicated unless the symptoms are not resolving and infection last longer than 4 weeks. Laboratory testing can be indicated in certain situations such as a suspected chlamydial infection in a newborn, an immune-compromised patient, excessive amounts of discharge, or suspected gonorrhea co-infection. In the office, physicians can run tests to positively identify adenovirus with a specificity and sensitivity of 89% and 94%, respectively. However, ophthalmologists usually can make the diagnosis clinically with confirmational additional testing.[23]
Regarding adenovirus testing, the gold standard has traditionally been cell culture because once the virus is isolated, the diagnosis is definitive and the characterization of the virus can be undertaken.[24] Disadvantages include cost and increased time associated with cell culture-based testing. The mainstay of viral conjunctivitis testing in the developed world is the detection of viral DNA by polymerase chain reaction (PCR). PCR for adenovirus has been shown to be 93% sensitive and 97.3% specific from conjunctival swabs, with similar values, found for HSV diagnosis.[24] A recent development has been the creation of a rapid detection testing platform for adenovirus, the AdenoPlus assay (Rapid Pathogen Screening Inc., Sarasota, Florida, USA). This is a swift office-based test designed to detect 53 serotypes of adenovirus and provide a result within 10 minutes.[25] Studies have demonstrated high specificity values of 92% to 98% in detecting adenoviral conjunctivitis. [26][27][28] However, the test has lower sensitivity reported compared with PCR analysis.[26][27][28] Rapid detection testing can be more useful in the future once viral conjunctivitis treatments reach the clinical setting.[29]
Treatment / Management
Treatment for viral conjunctivitis is aimed at symptomatic relief and not to eradicate the self-limiting viral infection. The resolution of conjunctivitis can take up to 3 weeks. Treatment includes using artificial tears for lubrication four times a day or up to ten times a day with preservative-free tears. Cool compresses with a wet washcloth to the periocular area may provide symptomatic relief. Preventing the spread of infection to the other eye or other people requires the patient to practice good hand hygiene with frequent washing, avoidance of sharing towels or linens, and avoiding touching their eyes. A person is thought to shed the virus while their eyes are red and tearing.
If a membrane or pseudomembrane is present, it can be peeled at the slit lamp to improve patient comfort and prevent any scar formation from occurring. These membranes can either be peeled with a jeweler forceps or a cotton swab soaked with topical anesthetic. Topical steroids can help with the resolution of symptoms. However, they can also cause the shedding of the virus to last longer. Patients should be informed that they are highly contagious and should refrain from work or school until their symptoms resolve. While using steroids, they may still shed the virus without the visual symptoms that would indicate that they have an infection. Steroids should be reserved for patients with decreased vision due to their subepithelial infiltrates or severe conjunctival injection causing more the expected discomfort.[30][31](B3)
The use of povidone-iodine, a non-specific disinfectant, is a promising new treatment for adenoviral conjunctivitis.[25] This is an inexpensive and widely available antiseptic solution which is used as part of the aseptic preparation for ocular surgery. It is able to kill extracellular organisms but has no effect intracellularly. It does not induce drug resistance because its mechanism of action is not immunologically dependent. A single dose of 2.5% povidone-iodine in infants with adenoviral conjunctivitis resulted in a reduction in symptom severity and reduced recovery time without significant side effects.[32](B3)
Topical corticosteroids alone are contraindicated in epithelial herpes simplex keratitis and are associated with prolonged viral shedding and infection.[29] When used in combination with an anti-infective, corticosteroids have demonstrated good tolerability and efficacy in treating the inflammatory and infectious components of conjunctivitis.[33][34] (A1)
Differential Diagnosis
While the most common causes of conjunctivitis are viral or bacterial and due to allergic reactions, there are other causes of conjunctivitis that should be considered when treatment does not improve symptoms. Uveitis is a local autoimmune reaction that causes the eye to become inflamed and is commonly mistaken for conjunctivitis. Uveitis can be a local reaction that is idiopathic or a manifestation of a systemic autoimmune disease such as rheumatoid arthritis, lupus, or ankylosis spondylitis. Systemic autoimmune disease such Sjogren syndrome or Stevens-Johnson syndrome can also mimic conjunctivitis by presenting with conjunctival erythema and discharge.
A systemic workup should be initiated if any of these diseases are suspected. The most life or sight-threatening masqueraders of conjunctivitis include cavernous carotid fistula, orbital cellulitis, and orbital hemorrhage. In cavernous carotid fistulas, an abnormal communication between the arterial and venous circulation form causing vasodilation of the venous system. Subsequently, the fistula can cause rupture and hemorrhage, leading to irreversible damage to the eye and/or death. Due to venostasis, the ophthalmic vein dilates and causes congestion of the episcleral vessels mimicking conjunctivitis. Proptosis and a pulsatile globe can help differentiate between a fistula and conjunctivitis. Orbital cellulitis is an infection posterior to the septum and involves the orbital contents. Patients present with similar symptoms of conjunctivitis, but will also have pain with eye movements or even restricted eye movements. Lastly, an orbital hemorrhage is an ophthalmic emergency. The cause is mostly traumatic, but it is possible to have a spontaneous hemorrhage, especially in patients on anticoagulants, that present with proptosis, tight eyelids, and erythema of the conjunctiva.
Prognosis
The majority of cases of virus conjunctivitis resolve on their own. In rare cases, chronic infection may occur. Most cases resolve within 14-30 days. In some patients, photophobia, diminished vision and glare may be a problem.
Complications
- Punctate keratitis
- Bacterial superinfection
- Conjunctival scarring
- Corneal ulceration
- Chronic infection
Deterrence and Patient Education
The vast majority of viral conjunctivitis is caused by adenoviruses, and frequent hand washing, disinfection, and isolation of conjunctivitis patients can reduce further community transmission. There is no single treatment modality for viral conjunctivitis. Symptom relief with artificial tears, cold-compresses, and antihistamines can be effective. Antibiotic drops can potentially increase bacterial resistance and membranes or pseudomembrane require removal to reduce discomfort and scarring. The use of topical corticosteroids is indicated in select cases in the presence of membrane formation and subepithelial infiltration associated with photophobia and decreased vision.
Enhancing Healthcare Team Outcomes
The majority of patients with viral conjunctivitis are first managed by the primary care giver, pediatrician or nurse practitioner. Even though viral conjunctivitis is a benign condition, it is contagious can be easily transmitted to others. The key is patient education.
Patients need to be educated that the condition is harmless and will resolve spontaneously. Hand washing should be emphasized since the infection is highly contagious. Parents and teachers should be educated on the importance of isolation in school to prevent epidemics. All patients with viral conjunctivitis who wear contact lenses should be told to refrain from wearing them until the symptoms have subsided.
The emergency department should have a special room for patients presenting with conjunctivitis to prevent spread to other patients. signs should be placed on the doors about not shaking hands and washing hands at every opportunity. Once the patient has been seen, he or she must be individually escorted out of the clinic to avoid contact with other patients. Many lawsuits have resulted in the past after patients in the emergency room acquired conjunctivitis from infected individuals, sitting in the same location.
While long-term sequelae are rare, chronic viral conjunctivitis can lead to a poor quality of life. Most cases take 1-4 weeks to recover without treatment. The morbidity is rare but can include corneal ulceration and punctate keratitis. Follow up with an ophthalmologist is recommended to ensure that no complications have occurred.[35][36] (Level V)
Media
(Click Image to Enlarge)
References
Keen M, Thompson M. Treatment of Acute Conjunctivitis in the United States and Evidence of Antibiotic Overuse: Isolated Issue or a Systematic Problem? Ophthalmology. 2017 Aug:124(8):1096-1098. doi: 10.1016/j.ophtha.2017.05.029. Epub [PubMed PMID: 28734327]
Level 1 (high-level) evidenceUdeh BL, Schneider JE, Ohsfeldt RL. Cost effectiveness of a point-of-care test for adenoviral conjunctivitis. The American journal of the medical sciences. 2008 Sep:336(3):254-64. doi: 10.1097/MAJ.0b013e3181637417. Epub [PubMed PMID: 18794621]
Rietveld RP, ter Riet G, Bindels PJ, Schellevis FG, van Weert HC. Do general practitioners adhere to the guideline on infectious conjunctivitis? Results of the Second Dutch National Survey of General Practice. BMC family practice. 2007 Sep 16:8():54 [PubMed PMID: 17868475]
Level 3 (low-level) evidenceEveritt H, Little P. How do GPs diagnose and manage acute infective conjunctivitis? A GP survey. Family practice. 2002 Dec:19(6):658-60 [PubMed PMID: 12429670]
Level 3 (low-level) evidenceLi J, Lu X, Jiang B, Du Y, Yang Y, Qian H, Liu B, Lin C, Jia L, Chen L, Wang Q. Adenovirus-associated acute conjunctivitis in Beijing, China, 2011-2013. BMC infectious diseases. 2018 Mar 20:18(1):135. doi: 10.1186/s12879-018-3014-z. Epub 2018 Mar 20 [PubMed PMID: 29558885]
Level 2 (mid-level) evidenceSow AS, Kane H, Ka AM, Hanne FT, Ndiaye JMM, Diagne JP, Nguer M, Sow S, Saheli Y, Sy EHM, De Meideros Quenum ME, Ndoye Roth PA, Ba EA, Ndiaye PA. [Senegalese experience with acute viral conjunctivitis]. Journal francais d'ophtalmologie. 2017 Apr:40(4):297-302. doi: 10.1016/j.jfo.2016.12.008. Epub 2017 Mar 23 [PubMed PMID: 28342559]
Azari AA, Barney NP. Conjunctivitis: a systematic review of diagnosis and treatment. JAMA. 2013 Oct 23:310(16):1721-9. doi: 10.1001/jama.2013.280318. Epub [PubMed PMID: 24150468]
Level 1 (high-level) evidenceChigbu DI, Labib BA. Pathogenesis and management of adenoviral keratoconjunctivitis. Infection and drug resistance. 2018:11():981-993. doi: 10.2147/IDR.S162669. Epub 2018 Jul 17 [PubMed PMID: 30046247]
Trinavarat A, Atchaneeyasakul LO. Treatment of epidemic keratoconjunctivitis with 2% povidone-iodine: a pilot study. Journal of ocular pharmacology and therapeutics : the official journal of the Association for Ocular Pharmacology and Therapeutics. 2012 Feb:28(1):53-8. doi: 10.1089/jop.2011.0082. Epub 2011 Sep 14 [PubMed PMID: 21916618]
Level 3 (low-level) evidenceLevinger E, Slomovic A, Sansanayudh W, Bahar I, Slomovic AR. Topical treatment with 1% cyclosporine for subepithelial infiltrates secondary to adenoviral keratoconjunctivitis. Cornea. 2010 Jun:29(6):638-40. doi: 10.1097/ICO.0b013e3181c33034. Epub [PubMed PMID: 20458220]
Level 2 (mid-level) evidenceBerisa Prado S, Riestra Ayora AC, Lisa Fernández C, Chacón Rodríguez M, Merayo-Lloves J, Alfonso Sánchez JF. Topical Tacrolimus for Corneal Subepithelial Infiltrates Secondary to Adenoviral Keratoconjunctivitis. Cornea. 2017 Sep:36(9):1102-1105. doi: 10.1097/ICO.0000000000001279. Epub [PubMed PMID: 28704319]
Arici C, Mergen B. Late-term topical tacrolimus for subepithelial infiltrates resistant to topical steroids and ciclosporin secondary to adenoviral keratoconjunctivitis. The British journal of ophthalmology. 2021 May:105(5):614-618. doi: 10.1136/bjophthalmol-2020-316196. Epub 2020 Jun 20 [PubMed PMID: 32563992]
Sheikh A, Hurwitz B, van Schayck CP, McLean S, Nurmatov U. Antibiotics versus placebo for acute bacterial conjunctivitis. The Cochrane database of systematic reviews. 2012 Sep 12:(9):CD001211. doi: 10.1002/14651858.CD001211.pub3. Epub 2012 Sep 12 [PubMed PMID: 22972049]
Level 1 (high-level) evidenceLangford MP, Anders EA, Burch MA. Acute hemorrhagic conjunctivitis: anti-coxsackievirus A24 variant secretory immunoglobulin A in acute and convalescent tear. Clinical ophthalmology (Auckland, N.Z.). 2015:9():1665-73. doi: 10.2147/OPTH.S85358. Epub 2015 Sep 10 [PubMed PMID: 26392747]
Zhang L, Zhao N, Huang X, Jin X, Geng X, Chan TC, Liu S. Molecular epidemiology of acute hemorrhagic conjunctivitis caused by coxsackie A type 24 variant in China, 2004-2014. Scientific reports. 2017 Mar 23:7():45202. doi: 10.1038/srep45202. Epub 2017 Mar 23 [PubMed PMID: 28332617]
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London, England). 2020 Feb 15:395(10223):497-506. doi: 10.1016/S0140-6736(20)30183-5. Epub 2020 Jan 24 [PubMed PMID: 31986264]
Danesh-Meyer HV, McGhee CNJ. Implications of COVID-19 for Ophthalmologists. American journal of ophthalmology. 2021 Mar:223():108-118. doi: 10.1016/j.ajo.2020.09.027. Epub 2020 Sep 22 [PubMed PMID: 32976847]
Binder AM,Biggs HM,Haynes AK,Chommanard C,Lu X,Erdman DD,Watson JT,Gerber SI, Human Adenovirus Surveillance - United States, 2003-2016. MMWR. Morbidity and mortality weekly report. 2017 Oct 6 [PubMed PMID: 28981484]
Alfonso SA, Fawley JD, Alexa Lu X. Conjunctivitis. Primary care. 2015 Sep:42(3):325-45. doi: 10.1016/j.pop.2015.05.001. Epub 2015 Jul 29 [PubMed PMID: 26319341]
Chintakuntlawar AV, Chodosh J. Cellular and tissue architecture of conjunctival membranes in epidemic keratoconjunctivitis. Ocular immunology and inflammation. 2010 Oct:18(5):341-5. doi: 10.3109/09273948.2010.498658. Epub [PubMed PMID: 20735288]
Marinos E, Cabrera-Aguas M, Watson SL. Viral conjunctivitis: a retrospective study in an Australian hospital. Contact lens & anterior eye : the journal of the British Contact Lens Association. 2019 Dec:42(6):679-684. doi: 10.1016/j.clae.2019.07.001. Epub 2019 Jul 9 [PubMed PMID: 31300283]
Level 2 (mid-level) evidenceNarayana S,McGee S, Bedside Diagnosis of the 'Red Eye': A Systematic Review. The American journal of medicine. 2015 Nov [PubMed PMID: 26169885]
Level 1 (high-level) evidenceSethuraman U, Kamat D. The red eye: evaluation and management. Clinical pediatrics. 2009 Jul:48(6):588-600. doi: 10.1177/0009922809333094. Epub 2009 Apr 8 [PubMed PMID: 19357422]
Elnifro EM, Cooper RJ, Klapper PE, Yeo AC, Tullo AB. Multiplex polymerase chain reaction for diagnosis of viral and chlamydial keratoconjunctivitis. Investigative ophthalmology & visual science. 2000 Jun:41(7):1818-22 [PubMed PMID: 10845603]
Kaufman HE. Adenovirus advances: new diagnostic and therapeutic options. Current opinion in ophthalmology. 2011 Jul:22(4):290-3. doi: 10.1097/ICU.0b013e3283477cb5. Epub [PubMed PMID: 21537185]
Level 3 (low-level) evidenceKam KY, Ong HS, Bunce C, Ogunbowale L, Verma S. Sensitivity and specificity of the AdenoPlus point-of-care system in detecting adenovirus in conjunctivitis patients at an ophthalmic emergency department: a diagnostic accuracy study. The British journal of ophthalmology. 2015 Sep:99(9):1186-9. doi: 10.1136/bjophthalmol-2014-306508. Epub 2015 Mar 30 [PubMed PMID: 25824258]
Sambursky R, Trattler W, Tauber S, Starr C, Friedberg M, Boland T, McDonald M, DellaVecchia M, Luchs J. Sensitivity and specificity of the AdenoPlus test for diagnosing adenoviral conjunctivitis. JAMA ophthalmology. 2013 Jan:131(1):17-22. doi: 10.1001/2013.jamaophthalmol.513. Epub [PubMed PMID: 23307204]
Level 1 (high-level) evidenceHoltz KK, Townsend KR, Furst JW, Myers JF, Binnicker MJ, Quigg SM, Maxson JA, Espy MJ. An Assessment of the AdenoPlus Point-of-Care Test for Diagnosing Adenoviral Conjunctivitis and Its Effect on Antibiotic Stewardship. Mayo Clinic proceedings. Innovations, quality & outcomes. 2017 Sep:1(2):170-175. doi: 10.1016/j.mayocpiqo.2017.06.001. Epub 2017 Jul 25 [PubMed PMID: 30225413]
Level 2 (mid-level) evidenceJhanji V, Chan TC, Li EY, Agarwal K, Vajpayee RB. Adenoviral keratoconjunctivitis. Survey of ophthalmology. 2015 Sep-Oct:60(5):435-43. doi: 10.1016/j.survophthal.2015.04.001. Epub 2015 May 5 [PubMed PMID: 26077630]
Level 3 (low-level) evidenceUsher P, Keefe J, Crock C, Chan E. Appropriate prescribing for viral conjunctivitis. Australian family physician. 2014 Nov:43(11):748-9 [PubMed PMID: 25551873]
Level 3 (low-level) evidenceShiota H, Ohno S, Aoki K, Azumi A, Ishiko H, Inoue Y, Usui N, Uchio E, Kaneko H, Kumakura S, Tagawa Y, Tanifuji Y, Nakagawa H, Hinokuma R, Yamazaki S, Yokoi N. [Guideline for the nosocomial infections of adenovirus conjunctivitis]. Nippon Ganka Gakkai zasshi. 2009 Jan:113(1):25-46 [PubMed PMID: 19227929]
Özen Tunay Z, Ozdemir O, Petricli IS. Povidone iodine in the treatment of adenoviral conjunctivitis in infants. Cutaneous and ocular toxicology. 2015 Mar:34(1):12-5. doi: 10.3109/15569527.2014.888077. Epub 2014 Mar 31 [PubMed PMID: 24678746]
Kovalyuk N, Kaiserman I, Mimouni M, Cohen O, Levartovsky S, Sherbany H, Mandelboim M. Treatment of adenoviral keratoconjunctivitis with a combination of povidone-iodine 1.0% and dexamethasone 0.1% drops: a clinical prospective controlled randomized study. Acta ophthalmologica. 2017 Dec:95(8):e686-e692. doi: 10.1111/aos.13416. Epub 2017 Mar 25 [PubMed PMID: 28342227]
Level 1 (high-level) evidenceFaraldi F, Papa V, Rasà D, Santoro D, Russo S. Netilmicin/dexamethasone fixed combination in the treatment of conjunctival inflammation. Clinical ophthalmology (Auckland, N.Z.). 2013:7():1239-44. doi: 10.2147/OPTH.S44455. Epub 2013 Jun 24 [PubMed PMID: 23836952]
Levine J, Snyder RW. Practical ophthalmic microbiology. Journal of ophthalmic nursing & technology. 1999 Mar-Apr:18(2):50-9; quiz 74-5 [PubMed PMID: 10409996]
Uçakhan Ö,Yanik Ö, The Use of Bandage Contact Lenses in Adenoviral Keratoconjunctivitis. Eye [PubMed PMID: 26671622]