Introduction
Chiari malformations are defined as a spectrum of hindbrain abnormalities involving the cerebellum, brainstem, skull base, and cervical cord. According to the type of herniation of the brain tissue displaced in the spinal canal and the characteristics of the anomalies of the brain or spine development, 4 types of Chiari malformations have been classified. Together with basilar invaginations, Chiari malformations represent the most common craniocervical junction malformations seen in adults. At the end of the nineteenth century, the pathologists Julius Arnold (1835-1915) and Hans Chiari (1851-1916) were the first to describe the condition as a complex clinical and pathological condition involving deformity of the cerebellum and brainstem in children.
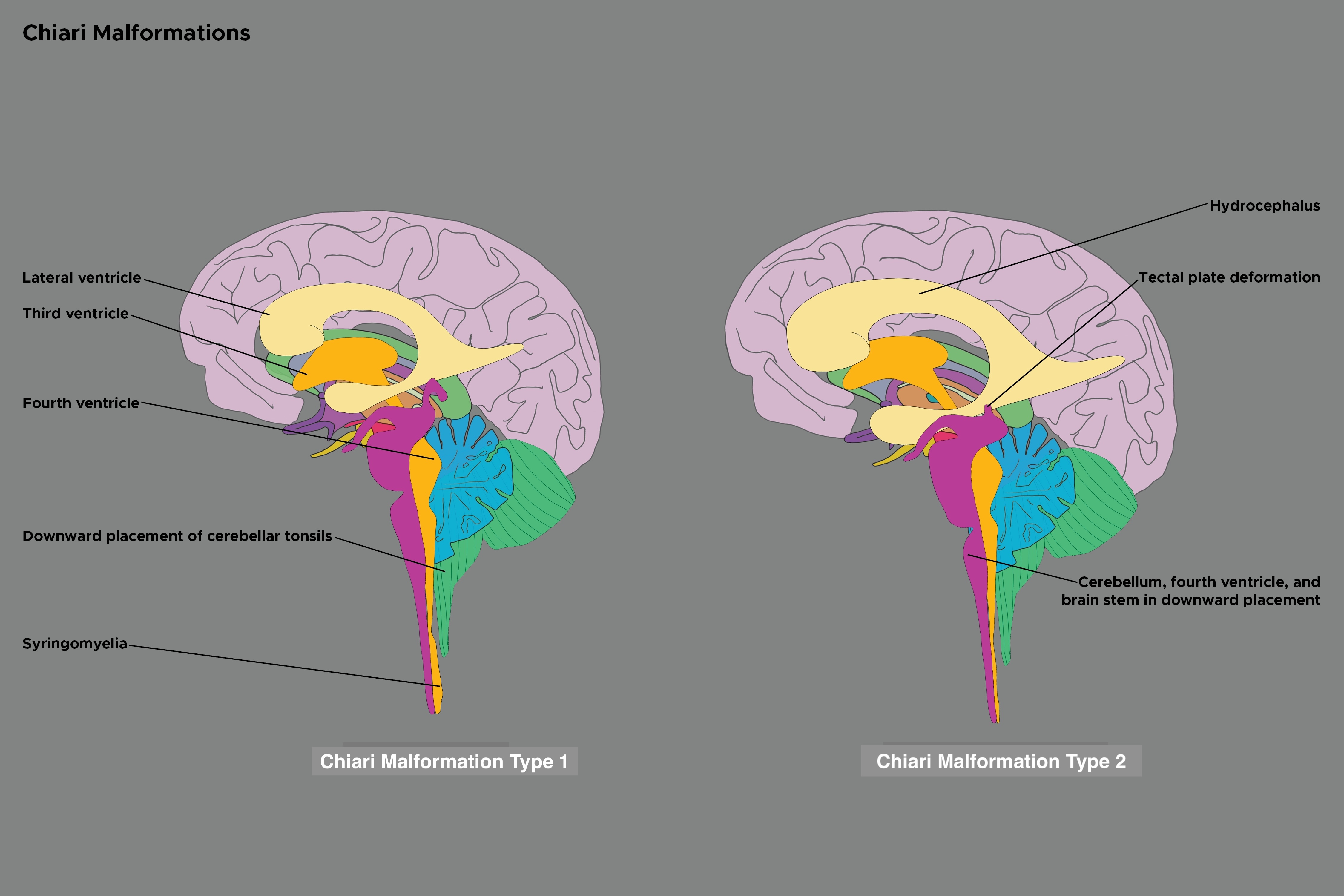
Among Chiari malformations, Chiari type 1 malformation is the more common variant. Chiari 1 malformation is characterized by the caudal descent of the cerebellar tonsils through the foramen magnum.[1] However, there is no accepted universal definition amongst clinicians as the malformation shows incongruity in clinic radiological correlation.[2] Some authors, for example, have recently proposed to refer to the Chiari 1 malformation as "Chiari syndrome," while the term malformation should be reserved for types 2 to 3.[3] (see Image. Chiari Malformation Types 1 and 2). Clinically, Chiari 1 malformation can be an asymptomatic hindbrain hernia or manifest from late childhood to adulthood with tussive headaches and focal neurological manifestations. On the other hand, Chiari types 2, 3, and 4 are congenital and clinically significant. The nosographic collocation of type 0 or 0.5 Chiari malformation or Chiari-like symptoms without tonsillar herniation, type 1.5 Chiari malformation between types 1 and 2, and complex Chiari is controversial and not universally accepted. (see Table. Chiari Malformation Types).[4]
Table. Chiari Malformation Types
| Chiari Type | Features |
| Chiari 0 |
|
| Chiari 0.5 |
|
| Chiari 1 |
|
| Chiari 1.5 |
|
| Chiari 2 (Arnold-Chiari malformation) |
|
| Chiari 3 |
|
| Chiari 3.5 |
|
| Chiari 4 |
|
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Chiari 1 malformation can have a genetic basis or be secondary to different conditions involving alterations in the basal skull, including craniosynostosis, craniocerebral disproportion, platybasia, secondary neurulation abnormalities, and bone metabolic disorders. This malformation can result from a build-up of pressure in the brain produced, for instance, by hydrocephalus or a tumor. Chiari malformation occurring due to hydrocephalus, idiopathic intracranial hypertension, pseudotumor cerebri, idiopathic intracranial hypotension, and an intracranial mass lesion is known as secondary Chiari malformation type 1.[5] Furthermore, iatrogenic Chiari 1, due to lumboperitoneal shunt for treatment of idiopathic intracranial hypertension, has also been reported.[6] An injury-related Chiari 1 type is a rare but possible condition.
In some cases, it is also possible that a traction mechanism from below is the cause of the disease. According to mechanisms of caudal traction or tethered cord, indeed, the lowering of the tonsils in Chiari 1 malformation could be provoked by traction by the filum terminal between the coccyx and the sacral part of the vertebral column, which pulls from the bone marrow and brainstem structures, causing, in turn, the descent of the cerebellar tonsils.[7]
When a genetic basis can be suggested, links to chromosomes 2, 9, 14, and 15 have been proposed.[8][9][10] For instance, a mutation in the NKX2-1 gene (14q13.3) that provides instructions for making the protein Nkx-2.1, a member of the homeobox protein family involved in the formation of body structures such as the forebrain during early embryonic development, has been recently identified, in a girl affected by Chiari 1 malformation.[11] Another potential mutation can involve EPAS1 (2p21) encoding the hypoxia-inducible factor 2-alpha (HIF-2-alpha), which is the major regulator of erythropoietin and is implicated in the endochondral and intramembranous ossification.[12] These genetic disorders likely impair the development of the para-axial mesoderm with herniation of the cerebellar tonsils, resulting in a small posterior fossa and a crowded foramen magnum. This is consistent with a proposed association with other mesodermal connective tissue disorders, for example, Ehlers-Danlos syndrome [13], although the relationship between this condition and Chiari 1 malformation is still unclear. Researchers from the Italian neurological Carlo Besta Institute have recently dissected different pathways (eg, disorders of the RAS/MAPK pathway) that can be found altered in Chiari 1 malformation and defined genetic syndromes.[14] Despite these data, the genetics of the Chiari 1 malformation needs more confirmation.[15] A recent exome sequencing identified the chromodomain genes CHD3 and CHD8 harboring numerous variants associated with CM1.[16] Multiple etiologic subtypes are likely, and Chiari 1 malformation can be heritable.
Epidemiology
Chiari 1 malformation is the most common Chiari malformation. This malformation type is estimated to occur in approximately 1 in 1000 live births, with a slight female: male predominance of 1.3 to 1.[17] The incidence is likely underestimated since many forms are paucisymptomatic and manifest clinically only in adulthood. Indeed, neuroimaging data suggest that the clinical condition may be more frequent, with an estimated prevalence of 1% in the pediatric population.[18][19]
Pathophysiology
Chiari 1 malformation is described according to the morphology of the hindbrain. Classic features are a >5 mm descent of the caudal tip of cerebellar tonsils past the foramen magnum; however, as little as <3 mm caudal cerebellar descent may be seen in a child presenting early with Chiari 1.[20][21][22][23] Of note, there is an associated herniation of the brainstem and spina bifida that characterize Chiari type 2, the classically described Chiari malformation; severe protrusion or herniation of the cerebellum and brainstem involving serious consequences on the development of the nervous system (ie, type 3); or incomplete or undeveloped cerebellum with structural alterations of the skull and spinal cord (ie, type 4).
In Chiari 1 malformation, the primary pathophysiology is tonsillar invagination and direct compression of neurological structures within the foramen magnum and upper spinal cord, with obstruction of cerebrospinal fluid (CSF) and potentially associated syringomyelia. This latter malformation, also termed Morvan disease, is myelopathy that consists of the abnormal formation of ≥1 cysts or cavities (ie, syrinxes) containing CSF inside the spinal cord and is detectable in 20% to 85% of Chiari 1 cases. Secondary features of syrinx formation may be further obstruction of spinal canal CSF outflow and further direct compression of neurovascular structures.[24] Regarding the location of syringomyelia development, the most commonly affected is the cervical region, followed by combined cervical and thoracic syringomyelia. The pathogenesis of syringomyelia must be well elucidated. A theory postulates the role of arterial pulsation that could induce a pressure dissociation between the subarachnoid spaces of the cranium and spinal cord. Again, other theories suggest that syrinx may represent the effect of the anatomical defect of the cerebellar tonsils or the consequence of the altered CSF flow.[25] Syringobulbia, which communicates with the fourth ventricle, has also been described.[26]
Because the foramen of Magendie can be obstructed, the fourth ventricle can enlarge. Hydrocephalus may occur in approximately 10% of patients. Skeletal associations may include platybasia or basilar invagination, Sprengel deformity, and atlantooccipital assimilation. Syndromic associations include Klippel-Feil, Gorham-Stout disease, Crouzon, and Pfeiffer syndromes.[21] Many of these conditions involve alterations of the basal skull and may be causes of the Chiari malformation.
History and Physical
Patients with Chiari 1 malformation are frequently asymptomatic. However, in those adult or young patients who are symptomatic, the most common symptom is pain or headache in the occipital or cervical region (ie, neck pain).[27] A history of headache or pain may be difficult to elicit in very young children whose symptoms are more likely to manifest as excessive crying, irritability, and failure to thrive.[22][28]
The Valsalva maneuver often exacerbates the headache associated with Chiari 1 malformation due to the reduced size of the foramen magnum. This should be differentiated from chronic headaches that do not vary with the Valsalva maneuver, which may be attributed to pathologies other than Chiari 1 malformation (eg, intracranial hypertension).[29][30] Individuals affected by Chiari 1 malformation have migraine headaches with a prevalence similar to that of the general population but with an earlier age of onset and a more severe clinical presentation.[31] Apart from headache and pain, a wide spectrum of clinical manifestations may characterize the malformation. In particular, signs and symptoms are mainly due to direct brainstem compression that may cause autonomic dysfunction.[32][33] Other signs (eg, scoliosis) are structural. Clinical features may include:
- Syncopal episodes and sinus bradycardia due to autonomic dysfunction
- Swallowing alterations and vomiting
- Balance difficulties with an unsteady gait
- Problems in hand coordination
- Sensorial manifestations (eg, numbness and tingling) in the extremities
- Dizziness
- Tinnitus
- Clinical manifestations of syringomyelia including progressive muscular weakness in the arms and legs, stiffness in the back, shoulders, arms, or legs, and acute paraparesis; syringobulbia can produce facial muscle weakness.
- Bladder and bowel disorders secondary to syrinx compression
- Scoliosis, particularly in pediatric patients, due to syringomyelia; recent studies found no association between syrinx length and holocord syrinx with scoliosis
- Nystagmus secondary Chiari 1 malformation with syringobulbia, though a nonspecific sign; gaze-evoked nystagmus may be due to cerebellar flocculus compressionde [32][33][34][27][35][36][37]
Adults and children with Chiari 1 malformation frequently have different presentations. Pediatric patients are more likely to present with brainstem dysfunction, sleep apnea, or feeding difficulty.[38] Feeding difficulties are typically due to glossopharyngeal and vagus nerve impairment, resulting in an absent gag reflex and hoarseness.[39] As the cerebellum is involved in higher cognitive functions, potential cognitive alterations have been recently investigated, and a generalized cognitive impairment in executive functioning, verbal fluency, spatial cognition, language, and memory processing has been reported.[40]
Evaluation
Imaging Studies
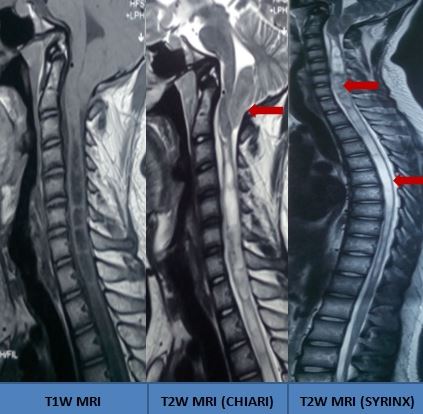
Magnetic resonance imaging (MRI) is the primary modality for Chiari 1 malformation diagnosis, depicting craniocervical junction anatomy and identifying secondary complications (eg, hydrocephalus or syringomyelia).[41] When the patient cannot undergo MRI scanning, other imaging modalities include CT myelography, noncontrast CT, and radiographs of the head and neck. In addition to tonsillar descent, there may be an appearance of "peg-like" or pointed tonsils in symptomatic and asymptomatic individuals on MRI.[42] Other findings include a cervicomedullary "kink," seen in up to 71% of symptomatic patients.[43] The greater the degree of cerebellar tonsil descent, the greater the likelihood that the patient is symptomatic.[21] (see Image. Chiari Malformation With Holocord Syrinx).
Asymptomatic patients who have incidental tonsillar ectopia may benefit from MRI with cerebral spinal fluid (CSF) flow studies. Positive findings on CSF flow include pulsatile systolic tonsillar descent and CSF flow obstruction at the level of the foramen magnum. These findings can provide further information to help assess whether the patient may benefit from surgery.[44] Chiari 1 malformation and syringomyelia may also be incidentally identified on routine obstetrical fetal anatomy ultrasounds.[45]
Ancillary Diagnostic Studies
Laboratory studies are not used to diagnose Chiari 1 malformation; however, these tests may be required for preoperative baseline assessment, including a complete blood count and comprehensive metabolic panel, in addition to other preoperative diagnostic studies (eg, chest x-ray and electrocardiogram). Other ancillary studies that may be considered include:
-
Sleep studies: Involves sleeping overnight in a room where they can monitor breathing, snoring, oxygenation, and seizure activity to identify evidence of sleep apnea.
-
Swallow studies: Fluoroscopy is used to watch the internal swallowing process to determine if an abnormality suggests lower brainstem dysfunction.
-
Brainstem auditory evoked potential: An electrical test to examine the function of the hearing apparatus and brainstem connections to determine if the brainstem is functioning correctly.
- Somatosensory evoked potentials: An electrical test of the nerves involved in sensation, giving information about peripheral nerve, spinal cord, and brain function.
Treatment / Management
A consensus on the precise algorithm for Chiari 1 malformation management has not been established. Generally, Chiari 1 malformation management encompasses a combination of conservative and surgical approaches through a multimodal dynamic strategy.
Conservative Therapy
Medical management in Chiari 1 malformation is limited to supportive symptomatic (eg, headaches or neck pain) treatment. Non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and physical support collars may provide symptomatic relief. However, these options offer little improvement of less common symptoms, for example, gait disturbance. Meditation, yoga, or mindfulness therapy have also been proposed for addressing pain.
Surgical strategies
Surgical treatment is typically reserved for patients who present with severe or worsening symptoms and who go on to have a confirmation of cerebellar descent on imaging and a Chiari malformation obstructing CSF flow confirmed by MRI. Surgery aims to provide decompression of the restricted cervicomedullary junction, allowing CSF flow to be restored to optimal levels. The primary approach involves performing a suboccipital craniectomy at the level of the C1 posterior arch (C1/2 laminectomy), with or without associated duraplasty.[46] Thus, this intervention, indicated as posterior fossa decompression (PFD), is the most adopted neurosurgical approach focused on restoring CSF flow across the foramen magnum. The procedure is performed in up to 99% of the literature.[47] A minimally invasive procedure allowing resection of submeningeal cerebellar tonsillar herniation followed by reconstruction of cisterna magna without craniectomy has been proposed for addressing Chiari 1 malformation with syringomyelia.[48] Of note, cine MRI has been proposed for guiding the intraoperative decision to realize duraplasty during PFD.[49] Among non-invasive approaches, several methods have also been proposed to decompress syringomyelia with distal drainage to the subarachnoid space (eg, syringosubarachnoid shunt).[50] The components of a standard 270-degree circumferential foramen magnum decompression include:[5]
- Suboccipital craniectomy
- C-1 laminectomy
- Resection of the suboccipital ligament
- Lateral decompression with the drilling of 1/5 of the occipital condyles
- Dural opening
- Arachnoid dissection
- Lateral decompression and opening of the foramina of Luschka
- Opening of the fourth ventricle
Posterior fossa decompression with duraplasty may be associated with superior long-term symptomatic relief, more significant syrinx reduction, and a lower need for revision decompression when compared to decompression without duraplasty. However, the former may result in a higher incidence of postoperative headache and nausea.[51] Ventral brainstem compression can be associated with Chiari 1 malformation due to osseo-ligamentous craniovertebral junction bony abnormalities that may result in ventral brainstem compression and instability. The initial reduction can be provided by crown halo traction under general anesthesia supplemented by neuromuscular blockade, after which an intraoperative distraction using occipitocervical instrumentation may further reduce the abnormality. Additionally, a fourth ventricle stent placement has been demonstrated to be a safe and effective treatment method.[52]
Differential Diagnosis
Important diagnoses to consider in the workup of Chiari 1 malformation include:
- Incidental tonsillar ectopia (ie, <5 mm)
- Chiari malformation types 2 to 4
- Idiopathic intracranial hypertension due to pseudotumor cerebri
- Craniospinal hypotension
- Basilar invagination
Prognosis
Surgical outcomes are favorable, with 73% of patients improving less than 1 year postoperatively and 79% at 1 to 3 years at follow-up.[53] PFD induced symptom improvement in about two-thirds of individuals, especially those without associated syringomyelia.[54]
Complications
The most common postoperative complications are CSF leakage and pseudomeningocele formation.[55][27] The latter may require revision surgery or shunt insertion.[56] Other complications include aseptic and bacterial meningitis, vertebral artery injury, neurologic deficits, and epidural hematoma formation.[57] Concerning the type of surgical approach, in a retrospective analysis, Farber et al found that meningitis occurred especially in decompression and duraplasty performed using bovine pericardial xenograft compared with the allograft method.[58]
Postoperative and Rehabilitation Care
Postoperatively, patients may experience headaches and neck pain due to the operation. Neck exercises may be given to aid in the return of full mobility as soon as possible. Patients typically return to work in 4 to 6 weeks, with a follow-up MRI performed around 6 months to 1 year. Full recovery from Chiari 1 malformation surgery may take months or longer. Patients should be instructed to slowly increase activity in a graded manner, avoiding strenuous lifting in the early phase of recovery.
Deterrence and Patient Education
While nothing can be done to prevent congenital Chiari 1 malformation, patient education plays a significant role in familiarising the patient with the signs and symptoms of the condition and helping increase awareness of the close family, friends, and carers who may spend significant periods with the patient. Patient education and counseling regarding conservative and surgical management strategies are also critical in the shared decision-making process.
Pearls and Other Issues
Facts to keep in mind regarding Chiari 1 malformation include the following:
- The Chiari 1 malformation is the most common Chiari manifestation resulting in hindbrain abnormality.
- While the genetic origin of the malformation requires more confirmation, the malformation can occur in several defined genetic syndromes.
- Many patients can be asymptomatic or paucisymptomatic, and the malformation is diagnosed more commonly in adolescents or adults.
- Patients may present with symptoms of occipital pain or chronic headache; however, they may also present with less specific symptoms such as swallow impairment or sleep apnea.
- MRI is the primary investigation of choice in these individuals, allowing complete visualization of the cervicomedullary junction.
- Because algorithms for managing Chiari 1 malformation are not well-established, combining medical and surgical approaches through a multimodal dynamic strategy is mandatory.
- Surgical decompression is performed successfully in symptomatic individuals, often significantly alleviating the patients presenting symptomatology and restoring full neurological function.
Enhancing Healthcare Team Outcomes
The Chiari 1 malformation is a rare developmental disorder best managed by an interprofessional team that includes a neurologist, pediatrician, surgeon, social worker, nurse, and physical therapist. These patients tend to have many physical and functional limitations, including impairment in swallowing, speaking, and even walking. While the prognosis for most patients is good, when clinically suspected, appropriate investigations should be performed promptly to facilitate a proper level of treatment (ie, conservative versus surgical) and, in turn, to prevent future deterioration.
In the management of Chiari 1 malformation, a collaborative and skilled interprofessional healthcare team is crucial to ensuring patient-centered care, positive outcomes, safety, and optimal team performance. The strategy involves interdisciplinary collaboration, fostering regular case discussions, and collaborative decision-making to integrate insights from various specialties. Treatment planning is comprehensive, addressing not only neurological aspects but also considering psychological and social components. Long-term management protocols are established, emphasizing continuous monitoring, follow-up, and adjustments to treatment plans as needed.
Care coordination is achieved through a patient-centered approach that prioritizes patient preferences and involves them in shared decision-making for personalized care plans. Streamlining the referral process between specialists ensures timely and coordinated care, supported by efficient health information exchange systems for secure sharing of patient information among team members.
By integrating these strategies, fostering interprofessional communication, and coordinating care effectively, healthcare professionals create a collaborative environment that enhances patient-centered care for Chiari 1 malformation. This approach promotes positive outcomes, patient safety, and optimal team performance in addressing the complex needs of individuals with this neuroanatomical condition.
Media
References
Abd-El-Barr MM, Strong CI, Groff MW. Chiari malformations: diagnosis, treatments and failures. Journal of neurosurgical sciences. 2014 Dec:58(4):215-21 [PubMed PMID: 25418275]
Muzumdar D. Chiari 1 malformation: Revisited. Journal of pediatric neurosciences. 2019 Oct-Dec:14(4):179. doi: 10.4103/jpn.JPN_146_19. Epub 2019 Dec 3 [PubMed PMID: 31908657]
Frič R, Eide PK. Chiari type 1-a malformation or a syndrome? A critical review. Acta neurochirurgica. 2020 Jul:162(7):1513-1525. doi: 10.1007/s00701-019-04100-2. Epub 2019 Oct 28 [PubMed PMID: 31656982]
Cools MJ, Wellons JC 3rd, Iskandar BJ. The Nomenclature of Chiari Malformations. Neurosurgery clinics of North America. 2023 Jan:34(1):1-7. doi: 10.1016/j.nec.2022.08.003. Epub 2022 Nov 2 [PubMed PMID: 36424049]
Arnautovic A, Pojskić M, Arnautović KI. Adult Chiari Malformation Type I: Surgical Anatomy, Microsurgical Technique, and Patient Outcomes. Neurosurgery clinics of North America. 2023 Jan:34(1):91-104. doi: 10.1016/j.nec.2022.09.004. Epub [PubMed PMID: 36424069]
Hentati A, Badri M, Bahri K, Zammel I. Acquired Chiari I malformation due to lumboperitoneal shunt: A case report and review of literature. Surgical neurology international. 2019:10():78. doi: 10.25259/SNI-234-2019. Epub 2019 May 10 [PubMed PMID: 31528416]
Level 3 (low-level) evidenceYan H, Han X, Jin M, Liu Z, Xie D, Sha S, Qiu Y, Zhu Z. Morphometric features of posterior cranial fossa are different between Chiari I malformation with and without syringomyelia. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2016 Jul:25(7):2202-9. doi: 10.1007/s00586-016-4410-y. Epub 2016 Jan 28 [PubMed PMID: 26821142]
Level 2 (mid-level) evidenceSpeer MC, George TM, Enterline DS, Franklin A, Wolpert CM, Milhorat TH. A genetic hypothesis for Chiari I malformation with or without syringomyelia. Neurosurgical focus. 2000 Mar 15:8(3):E12 [PubMed PMID: 16676924]
Abbott D, Brockmeyer D, Neklason DW, Teerlink C, Cannon-Albright LA. Population-based description of familial clustering of Chiari malformation Type I. Journal of neurosurgery. 2018 Feb:128(2):460-465. doi: 10.3171/2016.9.JNS161274. Epub 2017 Feb 3 [PubMed PMID: 28156254]
Boyles AL, Enterline DS, Hammock PH, Siegel DG, Slifer SH, Mehltretter L, Gilbert JR, Hu-Lince D, Stephan D, Batzdorf U, Benzel E, Ellenbogen R, Green BA, Kula R, Menezes A, Mueller D, Oro' JJ, Iskandar BJ, George TM, Milhorat TH, Speer MC. Phenotypic definition of Chiari type I malformation coupled with high-density SNP genome screen shows significant evidence for linkage to regions on chromosomes 9 and 15. American journal of medical genetics. Part A. 2006 Dec 15:140(24):2776-85 [PubMed PMID: 17103432]
Gonçalves D, Lourenço L, Guardiano M, Castro-Correia C, Sampaio M, Leão M. Chiari Malformation Type I in a Patient with a Novel NKX2-1 Mutation. Journal of pediatric neurosciences. 2019 Jul-Sep:14(3):169-172. doi: 10.4103/jpn.JPN_108_18. Epub 2019 Sep 27 [PubMed PMID: 31649781]
Rosenblum JS, Maggio D, Pang Y, Nazari MA, Gonzales MK, Lechan RM, Smirniotopoulos JG, Zhuang Z, Pacak K, Heiss JD. Chiari Malformation Type 1 in EPAS1-Associated Syndrome. International journal of molecular sciences. 2019 Jun 10:20(11):. doi: 10.3390/ijms20112819. Epub 2019 Jun 10 [PubMed PMID: 31185588]
Milhorat TH, Bolognese PA, Nishikawa M, McDonnell NB, Francomano CA. Syndrome of occipitoatlantoaxial hypermobility, cranial settling, and chiari malformation type I in patients with hereditary disorders of connective tissue. Journal of neurosurgery. Spine. 2007 Dec:7(6):601-9 [PubMed PMID: 18074684]
Level 2 (mid-level) evidenceSaletti V, Viganò I, Melloni G, Pantaleoni C, Vetrano IG, Valentini LG. Chiari I malformation in defined genetic syndromes in children: are there common pathways? Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2019 Oct:35(10):1727-1739. doi: 10.1007/s00381-019-04319-5. Epub 2019 Jul 30 [PubMed PMID: 31363831]
Capra V, Iacomino M, Accogli A, Pavanello M, Zara F, Cama A, De Marco P. Chiari malformation type I: what information from the genetics? Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2019 Oct:35(10):1665-1671. doi: 10.1007/s00381-019-04322-w. Epub 2019 Aug 5 [PubMed PMID: 31385087]
Sadler B, Wilborn J, Antunes L, Kuensting T, Hale AT, Gannon SR, McCall K, Cruchaga C, Harms M, Voisin N, Reymond A, Cappuccio G, Brunetti-Pierri N, Tartaglia M, Niceta M, Leoni C, Zampino G, Ashley-Koch A, Urbizu A, Garrett ME, Soldano K, Macaya A, Conrad D, Strahle J, Dobbs MB, Turner TN, Shannon CN, Brockmeyer D, Limbrick DD, Gurnett CA, Haller G. Rare and de novo coding variants in chromodomain genes in Chiari I malformation. American journal of human genetics. 2021 Jan 7:108(1):100-114. doi: 10.1016/j.ajhg.2020.12.001. Epub 2020 Dec 21 [PubMed PMID: 33352116]
Langridge B, Phillips E, Choi D. Chiari Malformation Type 1: A Systematic Review of Natural History and Conservative Management. World neurosurgery. 2017 Aug:104():213-219. doi: 10.1016/j.wneu.2017.04.082. Epub 2017 Apr 21 [PubMed PMID: 28435116]
Level 1 (high-level) evidencePertl B, Eder S, Stern C, Verheyen S. The Fetal Posterior Fossa on Prenatal Ultrasound Imaging: Normal Longitudinal Development and Posterior Fossa Anomalies. Ultraschall in der Medizin (Stuttgart, Germany : 1980). 2019 Dec:40(6):692-721. doi: 10.1055/a-1015-0157. Epub 2019 Dec 3 [PubMed PMID: 31794996]
Aitken LA, Lindan CE, Sidney S, Gupta N, Barkovich AJ, Sorel M, Wu YW. Chiari type I malformation in a pediatric population. Pediatric neurology. 2009 Jun:40(6):449-54. doi: 10.1016/j.pediatrneurol.2009.01.003. Epub [PubMed PMID: 19433279]
Level 2 (mid-level) evidenceHidalgo JA, Tork CA, Varacallo M. Arnold-Chiari Malformation. StatPearls. 2024 Jan:(): [PubMed PMID: 28613730]
Elster AD, Chen MY. Chiari I malformations: clinical and radiologic reappraisal. Radiology. 1992 May:183(2):347-53 [PubMed PMID: 1561334]
Tubbs RS, Lyerly MJ, Loukas M, Shoja MM, Oakes WJ. The pediatric Chiari I malformation: a review. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2007 Nov:23(11):1239-50 [PubMed PMID: 17639419]
Barkovich AJ, Wippold FJ, Sherman JL, Citrin CM. Significance of cerebellar tonsillar position on MR. AJNR. American journal of neuroradiology. 1986 Sep-Oct:7(5):795-9 [PubMed PMID: 3096099]
Level 2 (mid-level) evidenceDlouhy BJ, Dawson JD, Menezes AH. Intradural pathology and pathophysiology associated with Chiari I malformation in children and adults with and without syringomyelia. Journal of neurosurgery. Pediatrics. 2017 Dec:20(6):526-541. doi: 10.3171/2017.7.PEDS17224. Epub 2017 Oct 13 [PubMed PMID: 29027876]
Koyanagi I, Houkin K. Pathogenesis of syringomyelia associated with Chiari type 1 malformation: review of evidences and proposal of a new hypothesis. Neurosurgical review. 2010 Jul:33(3):271-84; discussion 284-5. doi: 10.1007/s10143-010-0266-5. Epub 2010 Jun 8 [PubMed PMID: 20532585]
Menezes AH, Greenlee JDW, Dlouhy BJ. Syringobulbia in pediatric patients with Chiari malformation type I. Journal of neurosurgery. Pediatrics. 2018 Jul:22(1):52-60. doi: 10.3171/2018.1.PEDS17472. Epub 2018 Apr 27 [PubMed PMID: 29701558]
Tubbs RS, Beckman J, Naftel RP, Chern JJ, Wellons JC 3rd, Rozzelle CJ, Blount JP, Oakes WJ. Institutional experience with 500 cases of surgically treated pediatric Chiari malformation Type I. Journal of neurosurgery. Pediatrics. 2011 Mar:7(3):248-56. doi: 10.3171/2010.12.PEDS10379. Epub [PubMed PMID: 21361762]
Level 2 (mid-level) evidenceListernick R, Tomita T. Persistent crying in infancy as a presentation of Chiari type I malformation. The Journal of pediatrics. 1991 Apr:118(4 Pt 1):567-9 [PubMed PMID: 2007932]
Level 3 (low-level) evidenceMcGirt MJ, Nimjee SM, Floyd J, Bulsara KR, George TM. Correlation of cerebrospinal fluid flow dynamics and headache in Chiari I malformation. Neurosurgery. 2005 Apr:56(4):716-21; discussion 716-21 [PubMed PMID: 15792510]
Chiapparini L, Saletti V, Solero CL, Bruzzone MG, Valentini LG. Neuroradiological diagnosis of Chiari malformations. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2011 Dec:32 Suppl 3():S283-6. doi: 10.1007/s10072-011-0695-0. Epub [PubMed PMID: 21800079]
Jokonya L, Makarawo S, Mduluza-Jokonya TL, Ngwende G. Fatal status migrainosus in Chiari 1 malformation. Surgical neurology international. 2019:10():243. doi: 10.25259/SNI_491_2019. Epub 2019 Dec 13 [PubMed PMID: 31893144]
Weig SG, Buckthal PE, Choi SK, Zellem RT. Recurrent syncope as the presenting symptom of Arnold-Chiari malformation. Neurology. 1991 Oct:41(10):1673-4 [PubMed PMID: 1922816]
Selmi F, Davies KG, Weeks RD. Type I Chiari deformity presenting with profound sinus bradycardia: case report and literature review. British journal of neurosurgery. 1995:9(4):543-5 [PubMed PMID: 7576283]
Level 3 (low-level) evidenceSchneider B, Birthi P, Salles S. Arnold-Chiari 1 malformation type 1 with syringohydromyelia presenting as acute tetraparesis: a case report. The journal of spinal cord medicine. 2013 Mar:36(2):161-5. doi: 10.1179/2045772312Y.0000000047. Epub [PubMed PMID: 23809533]
Level 3 (low-level) evidenceTubbs RS, Doyle S, Conklin M, Oakes WJ. Scoliosis in a child with Chiari I malformation and the absence of syringomyelia: case report and a review of the literature. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2006 Oct:22(10):1351-4 [PubMed PMID: 16532361]
Level 3 (low-level) evidenceStrahle JM, Taiwo R, Averill C, Torner J, Shannon CN, Bonfield CM, Tuite GF, Bethel-Anderson T, Rutlin J, Brockmeyer DL, Wellons JC, Leonard JR, Mangano FT, Johnston JM, Shah MN, Iskandar BJ, Tyler-Kabara EC, Daniels DJ, Jackson EM, Grant GA, Couture DE, Adelson PD, Alden TD, Aldana PR, Anderson RCE, Selden NR, Baird LC, Bierbrauer K, Chern JJ, Whitehead WE, Ellenbogen RG, Fuchs HE, Guillaume DJ, Hankinson TC, Iantosca MR, Oakes WJ, Keating RF, Khan NR, Muhlbauer MS, McComb JG, Menezes AH, Ragheb J, Smith JL, Maher CO, Greene S, Kelly M, O'Neill BR, Krieger MD, Tamber M, Durham SR, Olavarria G, Stone SSD, Kaufman BA, Heuer GG, Bauer DF, Albert G, Greenfield JP, Wait SD, Van Poppel MD, Eskandari R, Mapstone T, Shimony JS, Dacey RG, Smyth MD, Park TS, Limbrick DD. Radiological and clinical predictors of scoliosis in patients with Chiari malformation type I and spinal cord syrinx from the Park-Reeves Syringomyelia Research Consortium. Journal of neurosurgery. Pediatrics. 2019 Aug 16:():1-8. doi: 10.3171/2019.5.PEDS18527. Epub 2019 Aug 16 [PubMed PMID: 31419800]
Dobkin BH. The adult Chiari malformation. Bulletin of the Los Angeles neurological societies. 1977 Mar:42(1):23-7 [PubMed PMID: 610783]
Level 3 (low-level) evidenceGreenlee JD, Donovan KA, Hasan DM, Menezes AH. Chiari I malformation in the very young child: the spectrum of presentations and experience in 31 children under age 6 years. Pediatrics. 2002 Dec:110(6):1212-9 [PubMed PMID: 12456921]
Level 3 (low-level) evidenceDyste GN, Menezes AH, VanGilder JC. Symptomatic Chiari malformations. An analysis of presentation, management, and long-term outcome. Journal of neurosurgery. 1989 Aug:71(2):159-68 [PubMed PMID: 2746341]
García M, Lázaro E, López-Paz JF, Martínez O, Pérez M, Berrocoso S, Al-Rashaida M, Amayra I. Cognitive Functioning in Chiari Malformation Type I Without Posterior Fossa Surgery. Cerebellum (London, England). 2018 Oct:17(5):564-574. doi: 10.1007/s12311-018-0940-7. Epub [PubMed PMID: 29766459]
McVige JW, Leonardo J. Neuroimaging and the clinical manifestations of Chiari Malformation Type I (CMI). Current pain and headache reports. 2015 Jun:19(6):18. doi: 10.1007/s11916-015-0491-2. Epub [PubMed PMID: 26017710]
Aboulezz AO, Sartor K, Geyer CA, Gado MH. Position of cerebellar tonsils in the normal population and in patients with Chiari malformation: a quantitative approach with MR imaging. Journal of computer assisted tomography. 1985 Nov-Dec:9(6):1033-6 [PubMed PMID: 4056132]
Spinos E, Laster DW, Moody DM, Ball MR, Witcofski RL, Kelly DL Jr. MR evaluation of Chiari I malformations at 0.15 T. AJR. American journal of roentgenology. 1985 Jun:144(6):1143-8 [PubMed PMID: 3873794]
Hofkes SK, Iskandar BJ, Turski PA, Gentry LR, McCue JB, Haughton VM. Differentiation between symptomatic Chiari I malformation and asymptomatic tonsilar ectopia by using cerebrospinal fluid flow imaging: initial estimate of imaging accuracy. Radiology. 2007 Nov:245(2):532-40 [PubMed PMID: 17890352]
Level 3 (low-level) evidenceIruretagoyena JI, Trampe B, Shah D. Prenatal diagnosis of Chiari malformation with syringomyelia in the second trimester. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians. 2010 Feb:23(2):184-6. doi: 10.3109/14767050903061769. Epub [PubMed PMID: 19572237]
Level 3 (low-level) evidenceSiasios J, Kapsalaki EZ, Fountas KN. Surgical management of patients with Chiari I malformation. International journal of pediatrics. 2012:2012():640127. doi: 10.1155/2012/640127. Epub 2012 Jun 28 [PubMed PMID: 22811732]
Arnautovic A, Splavski B, Boop FA, Arnautovic KI. Pediatric and adult Chiari malformation Type I surgical series 1965-2013: a review of demographics, operative treatment, and outcomes. Journal of neurosurgery. Pediatrics. 2015 Feb:15(2):161-77. doi: 10.3171/2014.10.PEDS14295. Epub 2014 Dec 5 [PubMed PMID: 25479580]
Lou Y, Yang J, Wang L, Chen X, Xin X, Liu Y. The clinical efficacy study of treatment to Chiari malformation type I with syringomyelia under the minimally invasive surgery of resection of Submeningeal cerebellar Tonsillar Herniation and reconstruction of Cisterna magna. Saudi journal of biological sciences. 2019 Dec:26(8):1927-1931. doi: 10.1016/j.sjbs.2019.07.012. Epub 2019 Jul 25 [PubMed PMID: 31885484]
Delavari N, Wang AC, Bapuraj JR, Londy F, Muraszko KM, Garton HJL, Maher CO. Intraoperative Phase Contrast MRI Analysis of Cerebrospinal Fluid Velocities During Posterior Fossa Decompression for Chiari I Malformation. Journal of magnetic resonance imaging : JMRI. 2020 May:51(5):1463-1470. doi: 10.1002/jmri.26953. Epub 2019 Oct 30 [PubMed PMID: 31667928]
Amarouche M, Minichini V, Davis H, Giamouriadis A, Bassi S. Syringosubarachnoid shunt: insertion technique. British journal of neurosurgery. 2023 Jun:37(3):476-479. doi: 10.1080/02688697.2019.1700407. Epub 2019 Dec 18 [PubMed PMID: 31852253]
Giannakaki V, Wildman J, Thejasvin K, Pexas G, Nissen J, Ross N, Mitchell P. Foramen Magnum Decompression for Chiari Malformation Type 1: Is There a Superior Surgical Technique? World neurosurgery. 2023 Feb:170():e784-e790. doi: 10.1016/j.wneu.2022.11.119. Epub 2022 Nov 29 [PubMed PMID: 36455845]
Sun P, Zhou M, Liu Y, Du J, Zeng G. Fourth ventricle stent placement for treatment of type I Chiari malformation in children. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2023 Mar:39(3):671-676. doi: 10.1007/s00381-022-05793-0. Epub 2022 Dec 26 [PubMed PMID: 36572815]
Greenberg JK, Yarbrough CK, Radmanesh A, Godzik J, Yu M, Jeffe DB, Smyth MD, Park TS, Piccirillo JF, Limbrick DD. The Chiari Severity Index: a preoperative grading system for Chiari malformation type 1. Neurosurgery. 2015 Mar:76(3):279-85; discussion 285. doi: 10.1227/NEU.0000000000000608. Epub [PubMed PMID: 25584956]
De Vlieger J, Dejaegher J, Van Calenbergh F. Multidimensional, patient-reported outcome after posterior fossa decompression in 79 patients with Chiari malformation type I. Surgical neurology international. 2019:10():242. doi: 10.25259/SNI_377_2019. Epub 2019 Dec 13 [PubMed PMID: 31893143]
Rocque BG, Oakes WJ. Surgical Treatment of Chiari I Malformation. Neurosurgery clinics of North America. 2015 Oct:26(4):527-31. doi: 10.1016/j.nec.2015.06.010. Epub 2015 Aug 4 [PubMed PMID: 26408062]
Lei ZW, Wu SQ, Zhang Z, Han Y, Wang JW, Li F, Shu K. Clinical Characteristics, Imaging Findings and Surgical Outcomes of Chiari Malformation Type I in Pediatric and Adult Patients. Current medical science. 2018 Apr:38(2):289-295. doi: 10.1007/s11596-018-1877-2. Epub 2018 Apr 30 [PubMed PMID: 30074187]
Tubbs RS, Smyth MD, Wellons JC 3rd, Oakes WJ. Distances from the atlantal segment of the vertebral artery to the midline in children. Pediatric neurosurgery. 2003 Dec:39(6):330-4 [PubMed PMID: 14734868]
Farber H, McDowell MM, Alhourani A, Agarwal N, Friedlander RM. Duraplasty Type as a Predictor of Meningitis and Shunting After Chiari I Decompression. World neurosurgery. 2018 Oct:118():e778-e783. doi: 10.1016/j.wneu.2018.07.050. Epub 2018 Jul 17 [PubMed PMID: 30026145]