 Anatomy, Abdomen and Pelvis: Cardinal Ligaments (Mackenrodts, Transverse Cervical, or Lateral Cervical Ligaments)
Anatomy, Abdomen and Pelvis: Cardinal Ligaments (Mackenrodts, Transverse Cervical, or Lateral Cervical Ligaments)
Introduction
Primary Support
The muscles of the pelvic floor and the connective tissue of the pelvis, including pelvic fascia, provide stability to the pelvic floor and are essential for the support of pelvic viscera. The visceral layer of pelvic fascia and parametrium becomes condensed around the uterus to form primary support of the uterus in the form of true ligaments; these include:
- Anteriorly: Pubocervical ligament
- Laterally: Cardinal ligament
- Posteriorly: Uterosacral ligament
- Round ligament
The cardinal ligament and the uterosacral ligaments provide apical support for the uterus and upper vagina (see Image. Uterine Tubal Anatomy and Ligaments).[1] The cardinal ligament is a paired thickening of the parametrium and pelvic fascia at the base of the broad ligament, which extends between the cervix and vaginal fornix medially to the sidewall of the pelvis laterally. It is composed of loose areolar connective tissue surrounded by blood vessels, nerves, and lymphatics.[2] As per Terminologia Anatomica, the cardinal ligament has the name parametrium or paracervix; however, it is also referred to as Mackenrodt ligament, transverse cervical ligament, lateral cervical ligament, paracervical ligament, retinaculum uteri sustentaculum of Bonny or the web are the other terms also used for it.[3]
Secondary Support
Peritoneal folds related to the uterus form less important secondary support of the uterus in the form of peritoneal ligaments; these include:
- Anteriorly: Uterovesical fold (anterior ligament)
- Posteriorly: Rectouterine fold (posterior ligament)
- Laterally: Broad ligament
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Macroscopic Structure
The cardinal ligament is the bilateral fan-shaped condensation of the parametrium and endopelvic fascia at the base of the broad ligament with the following attachments:
- Medial (proximal) attachment: Lateral wall of the cervix and lower vagina [4][5]
- Lateral (distal) attachment: Lateral pelvic wall near the internal iliac vessel origin [4][5]
- Caudal attachment: With the superior fascia of the levator ani muscle [6]
- Cranial attachment: Broad ligament of the uterus [6]
- Posteriorly: Confluent with the attachment of the uterosacral ligament forming cardinal-uterosacral confluence (CUSC). [6]
From its medial attachment, it runs posterolateral; near the pelvic wall, it spreads out in a fan-shaped manner in the transverse plane.
Sections
The total average length of the cardinal ligament is around 10 cm, which is divisible into 3 sections.
- Distal (cervical) section: This is the most medial section, which is attached to the cervix & vagina. Posteriorly, this part is confluent with the uterosacral ligament to form the CUSC. CUSC is very important for vaginal vault support. The absence of significant neural or vascular structures makes this section suitable for surgical use. Its average length is 2.1 cm, and its average thickness is 2.0 cm.[6]
- Intermediate section: This section is related to the ureter. The ureter in this section is crossed superiorly by the uterine artery and vein, and the deep uterine vein may separate the ureter from the neural structures of the dorsal portion, so this section is not disturbed in surgery for pelvic organ prolapse. Its average length is 3.4 cm, and its average thickness is 1.8 cm.[6]
- Proximal (pelvic) section: This is the lateral most and thickest section, which is triangular on a cross-section. It is attached to the pelvic sidewall with an apex at the first branch of the internal iliac artery. Its average length is 4.6 cm, and the maximum average width is 2.1 cm.[6]
According to Tauchi, the cardinal ligament divides in a Y-shaped manner at about the middle of the proximal and distal attachments into 2 parts (branches).[7] One branch, which is composed of nerve fibers and the veins returning from the post-lateral wall of the bladder, is the vesical branch of the cardinal ligament, and the other branch, which is composed of nerve fibers and the veins returning from the uterine cervix, is the cervical branch of the cardinal ligament).
Subdivisions and Contents
The cardinal ligament is divisible into 2 parts: the cranial or superficial vascular part, which chiefly contains vessels, and the caudal or deep neural part, which contains inferior hypogastric plexus nerves.[8][9][10] The passage of the ureter in the intermediate section divides the cardinal ligament into two parts. Tissues that are situated and cross cranially over the ureter are categorized with the parametrium, and the tissues that are situated and cross underneath the ureter are categorized along with the paracervix. The former was considered to correspond to the cranial portion of the cardinal ligament, whereas the latter was considered to correspond to the caudal portion of the cardinal ligament.[4]
- Vascular part (the cranial portion of cardinal ligament, parametrium): An extension of the perivascular sheath of internal iliac vessel branches going to the genital tract that contains:
- Internal iliac artery
- Uterine artery and vein
- Vaginal artery
- Vesical artery
- Smooth muscle
- Connective tissue
- Lymph nodes
- Adipose tissue [4]
- Neural part (the caudal portion of cardinal ligament, paracervix): An extension of the inferior hypogastric plexus that contains:
- Autonomous nerve fibers
- Hypogastric nerve
- Extensions of the inferior hypogastric plexus (pelvic plexus)
- Vessels [4]
Microscopic Structure
According to Range et al., microscopically, the cardinal ligament is chiefly made up of blood vessels (mainly veins), nerves originating from the inferior hypogastric plexus, lymphatic vessels, and the surrounding loose areolar connective tissue.[2] It contains a network of collagen fibers and a few isolated elastic fibers with numerous cellular elements, particularly fibroblasts. They determined that it was not a ligament in the sense of a separate thickening of connective tissue. The cardinal ligaments of women with a prolapsed uterus showed a higher expression of collagen III and tenascin and lower quantities of elastin.[11] Altered connective tissue distribution in the cardinal ligaments with fewer and thinner collagen fibers has been reported in women with prolapse of the pelvic organ.[12]
Functions
In the standing position, the cardinal ligament has a vertical orientation, while the uterosacral ligaments are dorsally oriented, and together they provide apical support for the uterus and vagina.[13] It gives hammock-like support to the uterus that holds the cervix in position and prevents its downward displacement through the vagina.
Embryology
The lateral cervical ligament appears during the tenth week of intrauterine life.[14]
Surgical Considerations
The cardinal ligament is one of the pedicles the surgeon must secure during a hysterectomy. Due to the absence of basic neurovascular structure, the first pedicle of transvaginal hysterectomy involves a distal section of the cardinal ligament along with the CUSC. The presence of ureter and other neural and vascular structures make the intermediate section unsuitable for surgical use.[6] During a vaginal hysterectomy, the traction and cutting of the cardinal ligaments leads to the movement of the ureter out of the operative field. This action guards the ureter against possible iatrogenic injury.[5] After a hysterectomy, suspension of the vaginal vault to the CUSC provides surgical support of the vaginal vault and may reduce the chances of pelvic prolapse.[15]
Clinical Significance
Lymphatic vessels and lymph nodes in cardinal ligaments may be involved in cervical cancer, even up to the most lateral region near the pelvic sidewall. Therefore, in this condition, extensive resection of the cardinal ligament is a must to ensure a disease-free state.[16]
Media
(Click Image to Enlarge)
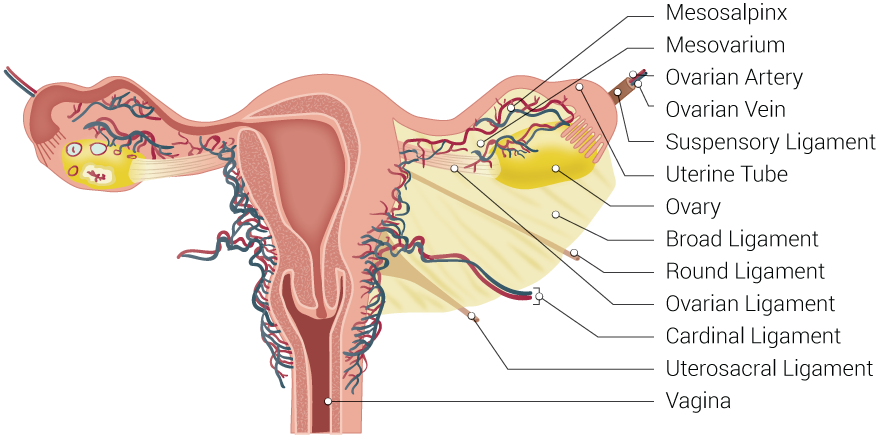
Uterine Tubal Anatomy and Ligaments. Shown in this illustration are anatomical structures surrounding the uterus and fallopian or uterine tubes, including the mesosalpinx, mesovarium, ovarian artery, ovarian vein, suspensory ligament, uterine tube, ovary, broad ligament, round ligament, ovarian ligament, cardinal ligament, uterosacral ligament, and vagina.
Contributed by B Palmer
References
DeLancey JO. Anatomic aspects of vaginal eversion after hysterectomy. American journal of obstetrics and gynecology. 1992 Jun:166(6 Pt 1):1717-24; discussion 1724-8 [PubMed PMID: 1615980]
RANGE RL, WOODBURNE RT. THE GROSS AND MICROSCOPIC ANATOMY OF THE TRANSVERSE CERVICAL LIGAMENT. American journal of obstetrics and gynecology. 1964 Oct 15:90():460-7 [PubMed PMID: 14217646]
Ercoli A, Delmas V, Fanfani F, Gadonneix P, Ceccaroni M, Fagotti A, Mancuso S, Scambia G. Terminologia Anatomica versus unofficial descriptions and nomenclature of the fasciae and ligaments of the female pelvis: a dissection-based comparative study. American journal of obstetrics and gynecology. 2005 Oct:193(4):1565-73 [PubMed PMID: 16202758]
Level 2 (mid-level) evidenceRamanah R, Berger MB, Parratte BM, DeLancey JO. Anatomy and histology of apical support: a literature review concerning cardinal and uterosacral ligaments. International urogynecology journal. 2012 Nov:23(11):1483-94. doi: 10.1007/s00192-012-1819-7. Epub 2012 May 23 [PubMed PMID: 22618209]
Cruikshank SH, Kovac SR. Role of the uterosacral-cardinal ligament complex in protecting the ureter during vaginal hysterectomy. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 1993 Feb:40(2):141-4 [PubMed PMID: 8094684]
Samaan A, Vu D, Haylen BT, Tse K. Cardinal ligament surgical anatomy: cardinal points at hysterectomy. International urogynecology journal. 2014 Feb:25(2):189-95. doi: 10.1007/s00192-013-2248-y. Epub 2013 Oct 30 [PubMed PMID: 24170225]
Tauchi K. [Studies on preservation of the vesical branch of the cardinal ligament in total hysterectomy for malignant uterine tumors]. Nihon Gan Chiryo Gakkai shi. 1989 Jul 20:24(7):1454-66 [PubMed PMID: 2809376]
Yabuki Y, Sasaki H, Hatakeyama N, Murakami G. Discrepancies between classic anatomy and modern gynecologic surgery on pelvic connective tissue structure: harmonization of those concepts by collaborative cadaver dissection. American journal of obstetrics and gynecology. 2005 Jul:193(1):7-15 [PubMed PMID: 16021052]
Kato T, Murakami G, Yabuki Y. Does the cardinal ligament of the uterus contain a nerve that should be preserved in radical hysterectomy? Anatomical science international. 2002 Sep:77(3):161-8 [PubMed PMID: 12422408]
Kato T, Murakami G, Yabuki Y. A new perspective on nerve-sparing radical hysterectomy: nerve topography and over-preservation of the cardinal ligament. Japanese journal of clinical oncology. 2003 Nov:33(11):589-91 [PubMed PMID: 14711985]
Level 3 (low-level) evidenceEwies AA, Al-Azzawi F, Thompson J. Changes in extracellular matrix proteins in the cardinal ligaments of post-menopausal women with or without prolapse: a computerized immunohistomorphometric analysis. Human reproduction (Oxford, England). 2003 Oct:18(10):2189-95 [PubMed PMID: 14507843]
Level 2 (mid-level) evidenceEid S, Iwanaga J, Oskouian RJ, Loukas M, Tubbs RS. Comprehensive Review of the Cardinal Ligament. Cureus. 2018 Jun 20:10(6):e2846. doi: 10.7759/cureus.2846. Epub 2018 Jun 20 [PubMed PMID: 30140597]
Chen L, Ramanah R, Hsu Y, Ashton-Miller JA, Delancey JO. Cardinal and deep uterosacral ligament lines of action: MRI based 3D technique development and preliminary findings in normal women. International urogynecology journal. 2013 Jan:24(1):37-45. doi: 10.1007/s00192-012-1801-4. Epub 2012 May 23 [PubMed PMID: 22618207]
Pietryga E, Woźniak W. The development of the uterine ligaments in human fetuses. Folia morphologica. 1992:51(2):181-93 [PubMed PMID: 1478574]
Sloth SB, Schroll JB, Settnes A, Gimbel H, Rudnicki M, Topsoee MF, Joergensen A, Nortvig H, Moeller C. Systematic review of the limited evidence for different surgical techniques at benign hysterectomy: A clinical guideline initiated by the Danish Health Authority. European journal of obstetrics, gynecology, and reproductive biology. 2017 Sep:216():169-177. doi: 10.1016/j.ejogrb.2017.07.012. Epub 2017 Jul 21 [PubMed PMID: 28779691]
Level 1 (high-level) evidenceGirardi F, Lichtenegger W, Tamussino K, Haas J. The importance of parametrial lymph nodes in the treatment of cervical cancer. Gynecologic oncology. 1989 Aug:34(2):206-11 [PubMed PMID: 2753426]