Introduction
Cardiac surgery is a medical specialty focused on the surgical treatment of heart and thoracic aorta pathologies. This surgery has become a routine practice for many heart conditions, with the median sternotomy approach remaining the gold standard for most open-heart procedures. Since the 19th century, the field has seen significant advancements, including the development of cardiopulmonary bypass (CPB), coronary artery bypass grafting (CABG), valve repairs, and minimally invasive techniques.[1][2]
Despite innovations, traditional methods remain crucial, especially in complex cases. Modern cardiac surgery addresses a wide range of conditions, from congenital heart defects to advanced coronary artery disease, necessitating interprofessional decision-making and careful patient selection to optimize outcomes. These advancements in cardiac surgery continue to evolve (see Image. Coronary Artery Bypass Surgery).[3][4]
Evolution of Cardiac Surgery
Billroth performed the first pericardiectomy in 1882. The first successful treatment of cardiac trauma was achieved by Ludwig Rehn in 1896 when he operated on a cardiac stab wound, challenging the then-prevailing belief that the heart was not an organ suitable for surgery. The development of CPB became essential for accessing critical cardiac structures, driven by the high mortality rates of early cardiac operations, such as the first embolectomy performed by Trendelenburg.[5]
Surgical revascularization is an option for relieving ischemic heart disease complicated by atherosclerosis.[6] Vineberg implanted the left internal mammary artery (LIMA) into the anterior free wall without forming direct anastomoses to the coronary vessels.[7] In earlier experiments, Vineberg observed that collaterals develop when ischemia is present. During the 1960s, several surgeons in different locations pioneered the first CABG operations.[8] The era of reversing coronary artery disease started with the invention of cardiac catheterization by Forssman in 1929 and the injection of contrast media by Shirey in 1962 to visualize coronary vessels and locate stenosis. Bypass grafting and interventional revascularization are now the 2 primary options for treating ischemic heart disease, alongside drug therapy.
Surgical treatment of valvulopathies began with closed mitral commissurotomy, where a finger or instrument was passed through the narrow orifice of the mitral stenosis to dilate or cut it, a procedure first performed by Cutler in 1923. The first artificial valve, the Hufnagel cage-and-ball valve, was introduced in 1952 and was placed in the descending thoracic aorta to prevent blood flow reversal in aortic regurgitation. In 1967, a similarly structured valve, the Starr-Edwards cage-and-ball valve, was implanted 1000 times for mitral valve disease.[9] Surgical techniques improved from early single-valve procedures to 4-valve replacement in 1992. Specialized techniques, such as the Ross procedure, were also introduced, which involved replacing the aortic valve with a pulmonic valve autograft. To treat proximal aortic dissection or aneurysm, Bentall developed a procedure that combines the implantation of an artificial aortic valve with an ascending aortic vessel prosthesis.
In 1944, cardiac surgeons Blalock, Taussig, and Thomas made their first venture into the field of congenital heart lesions by operating on a patient with tetralogy of Fallot—a cyanotic heart defect.[10] Pulmonary stenosis is another cyanotic heart lesion.[11] For cardiac arrhythmias, the Cox-Maze procedure provides a surgical treatment for atrial fibrillation. The development of cardiac pacemakers began with the application of external electrodes to stimulate the heart. Lillehei advanced this by placing electrodes directly into the heart during open-heart surgery. The first implanted pacemaker, however, lasted only 8 hours. Modern aggregates offer long-lasting solutions to diverse rhythm abnormalities.[12]
In 1967, several surgical teams worldwide performed the first heart transplants—Barnard in South Africa; Shumway at Stanford, who improved posttransplant survival with the addition of immunosuppressive treatment; and Kantrowitz, who pioneered pediatric heart transplantation in New York.[13] Some devices can supply mechanical circulatory support. Since 1963, the intra-aortic balloon pump has enhanced left ventricular function through counterpulsation. Open-heart surgery requires CPB to temporarily replace the function of the heart and lungs with an external circuit composed of pumps and an oxygenation membrane. Artificial hearts were first used extracorporeally in 1982, with subsequent devices enabling implantation.
Cardiac surgery carries high operative and perioperative risk, requiring professional staff and advanced equipment. Besides the diseases that require cardiac surgery, perioperative period often involves a range of complications, including systemic inflammatory response following CPB, myocardial stunning, low cardiac output syndrome, arrhythmias, massive transfusion needs, and multiorgan issues such as kidney injury, stroke, and respiratory distress.
With the rise of interventional and minimally invasive techniques for treating cardiac pathologies, both cardiology and cardiac surgery must adapt to these advancements.[14] As Lytle and Mack described in their 2005 editorial, "The times they are changing," the field of cardiac surgery is undergoing a fundamental transformation. In his presidential address, Guyton stated, "If we do not embrace innovation, we will become its victims." Recent developments include the establishment of cardiac arrest centers, broader and more accessible use of extracorporeal membrane oxygenation (ECMO), system process improvements, fast-track hospital stay, collaborative decision-making by interprofessional cardiovascular teams, and challenges posed by an aging patient population.[15][16][17][18]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The rib cage encases the chest organs, providing additional protection against external influences but making it more challenging for surgeons to access internal structures. The chest cavity is bordered by the ribs laterally, the sternum anteriorly, and the thoracic spine posteriorly. The chest cavity is divided into the bilateral pleural compartments and the mediastinum. The pleural spaces contain both wings of the lung. The mediastinum encloses several vital structures, including the esophagus, trachea, superior and inferior vena cavae, thoracic arteries, vagus nerve, azygos vein, lymphatic vessels, thymic remnant, and the pericardial sac containing the heart. The confined space within the pericardial sac places the heart at risk for tamponade physiology, which may occur when a hematoma compresses the heart, obstructing normal cardiac blood flow.[19]
As blood flows through the 4 chambers of the heart, it passes through 4 valves. Blood enters the right atrium via the superior and inferior vena cava, passes through the tricuspid valve into the right ventricle, and then flows through the pulmonary valve into the pulmonary circulation. The right side of the heart operates as a low-pressure system, unlike the left side, which supplies the systemic circulation and requires more myocardial tissue to generate higher pressure. Blood returns from the lungs through the 4 pulmonary veins into the left atrium, flows through the mitral valve into the left ventricle, and then passes through the aortic valve into the systemic circulation.[20] The aortic root comprises the sinuses of Valsalva, the interleaflet triangles, the sinotubular junction, and the aortic valve annulus, where the leaflets attach. The 3 leaflets are named according to their association with the right, left, and noncoronary cusps of the coronary arteries. As the components of the valve apparatus are interdependent, surgeons may need to address related structures to effectively treat the underlying pathology.
All cardiac valves are surrounded by an annulus, which poses challenges in creating artificial grafts that prevent leakage. Mitral valve replacement and the negative consequence of left ventricular outflow tract obstruction underscores the importance of understanding cardiac anatomy and physiology. While the aortic valve annulus is circular, the mitral valve annulus has a more crescent-shaped structure, necessitating more advanced prosthesis design and implantation techniques. Several artificial valve models illustrate this, each with distinct advantages and disadvantages related to anatomical, physiological, technical, and procedural factors. Additionally, the mitral valve features an annulus, and has anterior and posterior leaflets, each divided into 3 segments (A1 to A3 and P1 to P3). These segments are connected to the subvalvular apparatus, which includes chordae tendineae linking the valve leaflets to the papillary muscles.
Cardiac Electrical Conduction
The heart has an intrinsic rhythm that can be modulated by the autonomic nervous system: sympathetic stimulation accelerates the heart rate, whereas parasympathetic reaction slows it down. The cardiac electrical conduction is structured hierarchically, beginning with the sinus node, passing through the right atrium to the atrioventricular node, then traveling through the His bundle and Purkinje fibers to the ventricles. Understanding the anatomical and physiological aspects of this electrical activity is crucial for comprehending its clinical implications. Atrial fibrillation is common after cardiac surgery. The Maze procedure utilizes anatomical insights to disrupt uncontrolled atrial activity and address this condition. Additionally, the implantation of artificial heart valves can sometimes result in an atrioventricular block due to their proximity to the valve area.
Vessel Grafts
The quality of vessel grafts is vital for the outcome of CABG surgery. Surgeons can harvest various types of vessels, with arteries generally offering superior long-term durability compared to veins.[21] Preoperative assessment of graft quality is essential. Commonly used vessels include the left and right internal mammary arteries (LIMA and RIMA, respectively), radial arteries, and saphenous veins (saphenous vein grafts or SVGs). Due to vessel length, the RIMA is usually connected to the right coronary artery, while the LIMA is connected to the left anterior descending artery (LAD). Venous bypass grafts are commonly used to supply the posterior descending artery and the left circumflex artery. Additionally, venous grafts can be utilized to create bypasses to smaller branches, such as the diagonal branches of the LAD and the marginal branches of the left circumflex artery.[22]
Indications
Current guidelines outline the indications for cardiac surgery,[24][25] with general recommendations remaining consistent despite some variations. Decision-making is conducted by consensus, with cardiologists and surgeons collaborating as a heart team. Prior imaging—such as echocardiography, computed tomography (CT), or magnetic resonance imaging (MRI)—is routinely necessary to inform these decisions.
Valvular Disease Indicators for Cardiac Surgery
In valvular heart disease, stenotic lesions and regurgitation are differentiated through a systematic classification approach. Generally, valvulopathies are categorized into a 3-step approach—mild, moderate, and severe— unlike the 4-step angiographic grading used in catheterization laboratories. Severe valve regurgitation or stenosis necessitates intervention, with options for replacement or reconstruction depending on the affected valve.[23]
With the introduction of transcatheter aortic valve replacement (TAVR) by Cribier in 2002, cardiovascular teams now decide between surgical and interventional treatments for severe aortic stenosis.[24][25] Severe aortic stenosis is defined as an opening area of <1 cm². The operative risk is a crucial factor, and TAVR has emerged as a transformative option, especially for patients who are inoperable or at high risk for traditional surgical aortic valve replacement (SAVR). The EUROScore or Society of Thoracic Surgeons (STS) score helps determine that patients with high operative risk should receive TAVR.[26] Lower risk scores allow for SAVR. High operative risk is associated with conditions such as porcelain aorta, liver cirrhosis (Child-Pugh classes B and C), previous CABG with LIMA, and frailty. Aortic valve endocarditis also necessitates SAVR. Despite advancements in device technology and procedural techniques, complications such as paravalvular leakage, conduction disorders, coronary ostial obstruction, and cerebrovascular events persist with TAVR. These complications can significantly impact patient health and short- and long-term survival. Additionally, the incidence of surgical reinterventions following TAVR is increasing, with endocarditis and structural valve deterioration emerging as significant long-term issues.[27]
Decision-making for aortic regurgitation involves careful pathophysiologic assessment. Operative treatment is required for aortic regurgitation associated with enlargement of the ascending aorta. Additionally, surgery is necessary for patients with symptoms due to severe aortic regurgitation. Asymptomatic patients with decreased left ventricular ejection fraction (LVEF) or increased left ventricular residual volumes (ie, LVEF <50%, left ventricular end-diastolic diameter >70 mm, or left ventricular end-systolic diameter >50 mm) should also undergo surgery. For severe aortic stenosis, echocardiographic characteristics include a vena contracta greater than 6 mm, pressure half-time less than 200 ms, effective regurgitant orifice area greater than 30 mm², and regurgitant volume more than 60 mL.
Mitral stenosis is primarily caused by rheumatic heart disease, which is rare in industrialized countries. Mitral regurgitation is treated based on its etiology.[28] Primary mitral regurgitation describes the structural pathology of the mitral valve apparatus itself, including leaflets, annulus, chords, and papillary muscles. Primary mitral regurgitation is classified according to Carpentier. Secondary or functional mitral regurgitation is caused by left ventricular dilatation, ischemia, and tethering. In contrast to aortic valve pathology, mitral valve lesions are primarily treated with repair techniques, including Alfieri edge-to-edge repair, resection, annuloplasty, and notochordal repair. Severe mitral regurgitation is defined by echocardiographic criteria such as a vena contracta greater than 7 mm, a regurgitant volume greater than 60 mL, and a regurgitant fraction of more than 50%.[29]
Multivalvular disease presents challenging decision-making due to the limited number of studies available.[30] When surgery for left heart disease is planned, secondary tricuspid regurgitation may be addressed simultaneously. However, the criteria for evaluating the right ventricle and tricuspid valve to determine the need for surgery remain unclear. A tricuspid valve annulus diameter of more than 40 mm suggests the need for tricuspid valve repair if mitral valve surgery is also planned.[31][32][33][34][35][36]
Additional Indicators for Cardiac Surgery
Cardiac surgery helps treat various cardiac rhythm disturbances by implanting devices such as pacemakers, including dual chamber devices for atrioventricular blocks, defibrillators for ventricular arrhythmia, and cardiac synchronization therapy for advanced heart failure. Cardiac surgery is also indicated for congenital heart disease, categorized into cyanotic and non-cyanotic lesions. Surgical options include closing ventricular and atrial septal defects. Specialized techniques have been developed for certain genetic conditions, such as Ebstein anomaly, tetralogy of Fallot, and transposition of the great vessels.
Cardiac and pulmonary pathologies may require cardiovascular surgical treatment. The most common benign heart tumor is an atrial myxoma, while sarcoma is the most frequent malignant cardiac tumor. Secondary metastatic tumors are more common than primary cardiac tumors and may cause obstructive or embolic symptoms. Pulmonary thrombendarterectomy may be necessary as a final treatment option for severe pulmonary embolism. In cases involving the thoracic aorta, surgery for dissection, aneurysm repair, and vessel graft replacement may be indicated.
Surgical revascularization can be a preferred option for treating coronary artery disease.[39] The cardiovascular team, comprising cardiologists and cardiac surgeons, makes management decisions collaboratively. Decision aids, such as syntax scores, assess the complexity of coronary artery disease and guide the choice between treatment by CABG and percutaneous coronary intervention (PCI). CABG is commonly indicated for left main stem and triple vessel disease. High-risk PCI patients with complex stenotic lesions may still undergo percutaneous treatment despite their increased operative risk.
Terminal heart failure, despite optimal medical therapy, can be managed with cardiac resynchronization therapy, implantation of assist devices, or heart transplantation.[37] Resynchronization therapy is indicated for patients with severe left ventricular dysfunction (LVEF <35%), the New York Heart Association (NYHA) classes III and IV symptoms, and a QRS complex duration greater than 130 ms on electrocardiogram (ECG). In periods of organ shortage, assist devices are increasingly utilized as a treatment option.[38][39] Studies have shown comparable outcomes between treatment options.[40] The REMATCH trial demonstrated a 2-year survival advantage with assist devices (23%) compared to medical therapy (8%). Slaughter et al found that continuous flow assist devices had a median support duration of 1.7 years versus 0.6 years for pulsatile flow left ventricular assist devices, with 88% and 79% of time spent outside the hospital, respectively.[41] Timing and patient selection for assisted device implantation or heart transplantation remain challenging. The INTERMACS classification and the Lietz-Miller score or the Destination Therapy Risk score are valuable tools for selecting appropriate patients.
Contraindications
During operation preparation, risk factors and contraindications are carefully evaluated. As cardiac surgery is typically reserved for advanced cardiac diseases, the benefits of the procedure often outweigh the risks when considered as a last treatment option. The EuroScore risk stratification tool is commonly used to assess operative risk, along with other tools such as the Parsonnet score and the STS score, to determine patient eligibility for surgery.[42][43][44]
Operations may be postponed in patients with unstable conditions. Determining the optimal timing for CABG in a patient with myocardial infarction can be challenging. In cases of endocarditis requiring valve replacement, surgery may need to be performed on a septic patient to control the infection.
Equipment
Cardiac surgery requires sophisticated equipment. For diagnostic purposes, tools such as pulmonary artery catheters, thermodilution techniques, pulse contour analysis, and ultrasound can be used to assess cardiac performance and disease. Critical issues related to cardiac output, volume responsiveness, and tissue oxygenation must be addressed.[45]
Equipment for treatment includes pacemakers, assist devices, ECMO, and CPB. The application of CPB started in the 1930s when Gibbon used an external pump circuit to sustain life in Boston, though initial setbacks interrupted its development. In 1951, Dogliotti introduced a partial heart and lung machine capable of a 1 L/min flow, marking a significant step forward in the evolution of CPB technology. Lewis first used the hypothermic technique in 1952 to reduce metabolic demand and minimize heart injury while closing an atrial septal defect. Lillehei introduced the concept of cross-circulation, temporarily replacing a dog's circulation by sharing it with another. A broader application became feasible with Kirklin's modification of the IBM Gibbon machine, significantly increasing survival rates. CPB enables heart venting and a clear operating area.[46]
However, CPB is associated with adverse effects, including a systemic inflammatory response triggered by exposure to the circuit.[47] Modifications to surgical techniques, such as reducing the duration and size of CPB and altering the tubing surface, have shown beneficial effects. The inflammatory response triggered by CPB is similar to that seen in infections, characterized by elevated inflammatory markers and shock-like symptoms. However, the timing differs, with the inflammatory response peaking on the first postoperative day and gradually decreasing afterward.[48] Cuthbertson described SIRS due to CPB as an "ebb and flow" process, with an initial phase of reduced metabolic activity lasting 2 to 3 days, followed by a hypermetabolic phase that can persist for over a week. To mitigate these effects, various strategies have been proposed, including the use of aprotinin, heparin-coated CPB circuits, hemofiltration, leukofiltration, and off-pump coronary artery bypass (OPCAB).[49][50]
The use of CPB and assist devices necessitates frequent coagulation tests. In addition to routine coagulation diagnostics, such as the international normalized ratio and partial thromboplastin time, more detailed laboratory assessments may be required. These can include rotational thromboelastography, activated clotting time, and the measurement of specific coagulation factors such as antithrombin III, fibrinogen, and factor VII, especially in cases of postoperative bleeding.[51]
Veno-venous ECMO includes an oxygenator, supporting the respiratory system by adding oxygen and removing carbon dioxide. Veno-arterial ECMO (VA-ECMO) provides both oxygenation and decarboxylation while partially replacing cardiac output. Cannulation for VA-ECMO can be placed centrally in the ascending aorta during sternotomy, producing antegrade flow, or peripherally with cannulas in the external iliac artery and vein. ECMO can be used as a bridge to recovery, a bridge to another intervention, or a bridge to transplant. The use of intra-aortic balloon pumps has decreased as studies failed to demonstrate a mortality benefit. Initially, the physiological consideration was improved diastolic coronary perfusion of the coronaries and pull effect during systole via counterpulsation of a balloon placed in the descending thoracic aorta.
Choosing the appropriate prosthetic heart valve for replacement is crucial. Mechanical valves, which offer greater resistance to structural degeneration, require lifelong anticoagulation and are generally recommended for younger patients. In contrast, bioprosthetic valves made from porcine or pericardial tissue do not necessitate anticoagulation but may experience earlier degeneration and require reoperation.[52] Bioprosthetic heart valves are typically indicated for women planning to have children and older patients. The Ross procedure, involving a pulmonic autograft for the aortic position, is another option for aortic valve replacement.[53]
Personnel
After completing medical school, graduates can apply for cardiac surgery training, which varies in length and content. For those with prior general surgical experience, an additional 2 years of specialization is required. Alternatively, 6-year training programs offer subspecialty training in areas such as minimally invasive surgery, adult and pediatric and congenital cardiac surgery, vascular surgery, endovascular interventions, general thoracic surgery, and heart failure surgery.
Training in cardiac surgery is highly competitive and demanding due to the specialty's evolving nature, an increasingly elderly and multimorbid population, working hour restrictions, and the introduction of new interventional methods. Recent evaluations have predicted shortages of healthcare professionals in various countries over the coming decades. The cardiac perioperative team comprises cardiac surgeons and extracorporeal technologists, cardiac anesthesiologists, cardiac intensive care unit (ICU) clinicians, surgical nurses, cardiologists, and radiologists, each with specialized training.
Preparation
When preparing a patient for cardiac surgery, the following evaluations should be conducted:
- Blood tests to assess various body functions, including kidney and liver function tests, coagulation, complete blood count, and electrolytes.
- ECG to check for regular cardiac rhythmic activity.
- Echocardiography and cardiac catheterization to detect coronary artery disease and valvulopathies.
- Chest x-ray or chest CT to visualize thoracic comorbidities and plan the operative technique.
- Ultrasound of the neck vessels to evaluate stroke risk.
- Ultrasound of lower extremity veins to assess potential grafts.
- CT imaging to evaluate vascular and bony structures.
Carotid Doppler ultrasound should be performed in patients with left main disease, peripheral vascular disease, carotid bruits, a history of cerebrovascular accident, and heavy tobacco use, as well as in patients aged 65 or older. If significant stenosis is detected, further testing may be required, and endarterectomy might be considered.
CT imaging can significantly improve CABG surgical planning by providing a comprehensive understanding of the surgical field, which aids in optimizing the procedure and assessing potential risks and outcomes. Each CABG approach—such as primary sternotomy, redo sternotomy, and minimally invasive thoracotomy—presents unique challenges and risks. A preoperative CT scan aids in defining these considerations. Additionally, CT and CT angiography, with or without intravenous (IV) contrast, provide a noninvasive method to assess vascular and bony structures, guiding surgical planning effectively.[54]
Anticoagulation during the perioperative period requires careful management and special consideration. Platelet-inhibiting drugs should be discontinued before surgery based on the medication type; for instance, clopidogrel should be stopped 5 days before the procedure, while ASA and heparin may be continued until the operation. The benefits of revascularization must be weighed against bleeding risks. Strategies to mitigate bleeding complications in patients requiring urgent surgery while on anticoagulants include OPCAB, tailored coagulation diagnostics and management, administration of coagulation factors and platelet transfusions, and the use of antifibrinolytic agents.[55][56][57][58][59]
Technique or Treatment
Open heart surgery traditionally involves accessing the heart by opening the thorax via sternotomy or upper hemisternotomy. CABG is among the most common surgical procedures globally. Once the pericardial sac is opened with an inverted T incision, while sparing both phrenic nerves, cannulation, CPB, and cardioplegia are applied, allowing the heart to be mobilized for identifying the target arteries. Epiaortic ultrasound is used to assess atherosclerosis of the ascending aorta. After harvesting the grafts, they can be connected directly or using a T-graft technique to the coronary arteries and the aorta. Following anastomosis, success is confirmed by assessing flow rates through the grafts. After completing CPB, the thorax is closed, and the sternum is secured with wires. Pleural and mediastinal suction drains are left in place for the postoperative period. Intraoperatively placed epicardial electrodes connected to an external pacemaker help manage rhythmic complications but are removed before hospital discharge.
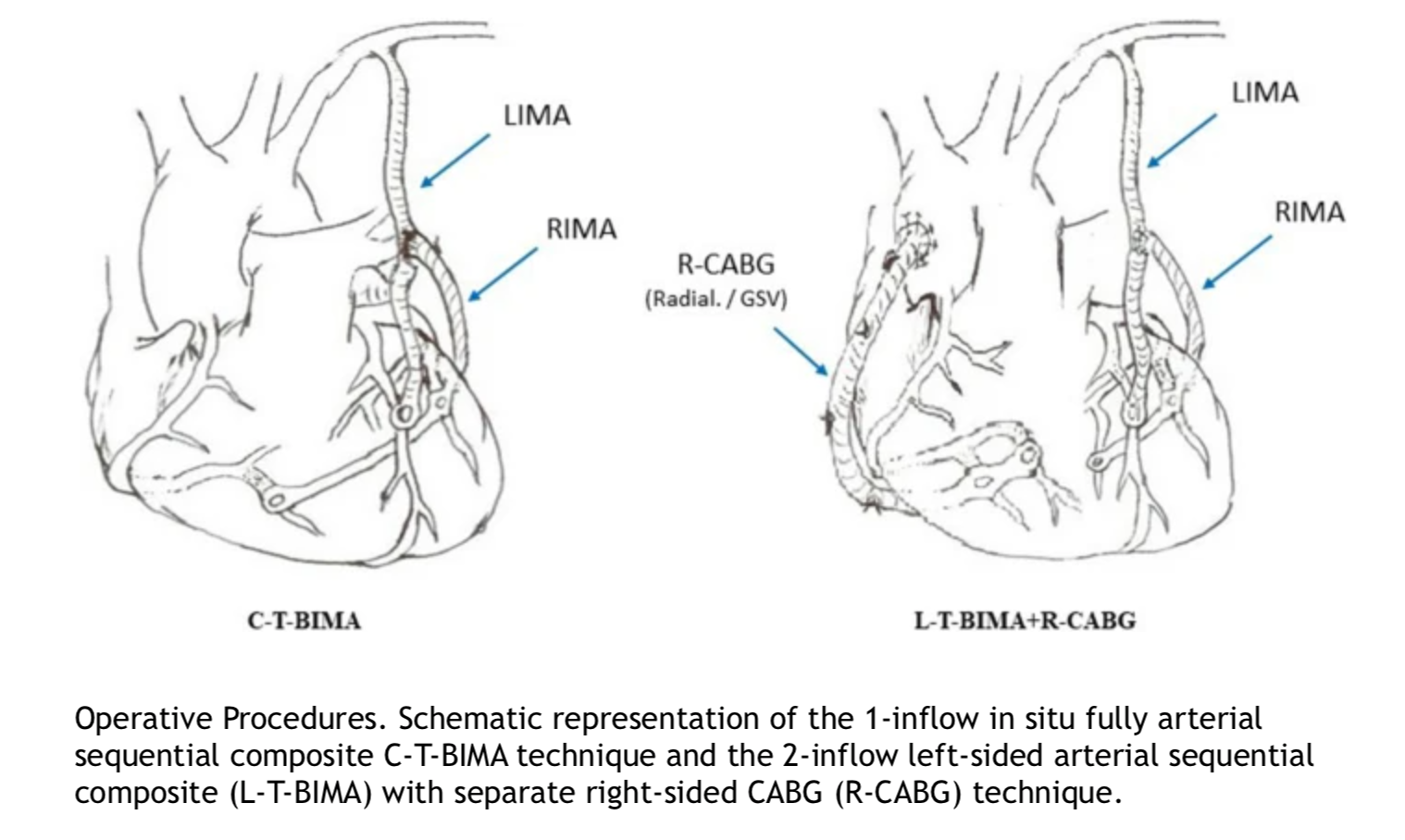
OPCAB is particularly beneficial for patients with high operative risk [60] and significant atherosclerosis of the ascending aorta, as clamping during CPB can release thrombogenic material and potentially cause a stroke. The no-touch technique minimizes manipulation of the potentially thromboembolic endothelial surface of the ascending aorta by using the internal mammary or innominate artery. This approach requires stabilizers and positioners for precise anastomosis to the coronary vessels, making it especially useful for high-risk patients. For these patients, surgical LIMA-to-LAD anastomosis combined with later PCI to other affected arteries, as part of hybrid coronary staged revascularization, may offer advantages over conventional CABG.[61][62] Although the inflammatory response is similar between on-pump and off-pump surgery, off-pump procedures have been associated with reduced transfusion requirements and other benefits. While off-pump bypass may be feasible in up to 95% of CABG patients, it has been performed in only about 20% of surgical revascularization cases recently (see Image. Coronary Revascularization Procedures).
Minimally invasive surgery and endoscopic CABG involve smaller incisions, video guidance, and specialized instruments. These techniques require additional training and are available only at select centers. Patients may experience reduced surgical trauma and faster postoperative recovery with these approaches. Many procedures can be performed using minimally invasive techniques, and with the advent of robotic surgery, robotic systems have also become a part of the cardiac operating room.
The myocardium can be protected during cardiac surgery using cardioplegia and hypothermia.[63] Various cardioplegic solutions are available, and cardioplegia can be administered either anterogradely via the aortic root or retrogradely through the coronary sinus.[64][65][66] Brain protection is achieved by enhancing brain perfusion, reducing thrombogenicity through modifications to blood constituents, and administering appropriate anticoagulation.[67][68][69]
Several valve-repair techniques have been established, including bicuspidization, DeVega, and the clover technique for the tricuspid valve, as well as the Alfieri edge-to-edge, foldoplasty, neochordae, and sliding plasty technique for the mitral valve. Depending on whether the aortic valve needs to be replaced or preserved, aneurysms and dissections of the ascending aorta may be addressed using the David, Yacoub, or Bentall techniques.[70][71]
Complications
The overall mortality rate in cardiac surgery ranges from 2% to 3%. Significant complications include postoperative bleeding, stroke,[72][73] renal failure,[74] mesenteric ischemia, atrial fibrillation,[75] cardiogenic shock,[76] and respiratory distress. Postoperative bleeding and hemorrhagic shock, along with coagulation disorders like heparin-induced thrombocytopenia, contribute to 10% to 20% of national blood product usage in cardiac surgery. Acute kidney injury affects up to 18% of patients undergoing cardiac procedures, with approximately 2% requiring renal replacement therapy. The incidence of these complications can serve as a quality indicator and impact both reimbursement and patient decision-making.
A nationally representative study has shown an increase in the incidence of postoperative stroke complications following CABG, corresponding with a rise in overall baseline patient risks. Among 2,569,597 CABG procedures, ischemic stroke occurred in 47,279 patients (1.8%), with the incidence rising from 1.2% in 2004 to 2.3% in 2015 (P < .001). Patient risk profiles have worsened over time, with stroke patients exhibiting higher Charlson comorbidity scores. Stroke was independently associated with a 3-fold increase in in-hospital mortality, an extended hospital stay of approximately 6 days, and an increase in total hospitalization costs by about $80,000. The strongest predictors of stroke were age 60 years or older and female sex (both P < .001).[77]
Myocardial infarction following cardiac surgery is classified as type 5 myocardial infarction according to the universal classification. The incidence ranges from 5% to 10%. Diagnosing postoperative myocardial infarction can be challenging due to routinely elevated cardiac enzyme levels from surgical manipulation and symptoms influenced by the postoperative status. Therefore, alternative diagnostic modalities, such as ECG, echocardiography, and coronary angiography, are crucial for assessing bypass patency. Echocardiography may reveal septal wall motion abnormalities that are not necessarily related to myocardial ischemia. Refractory shock and arrhythmias are highly suggestive of myocardial infarction. Myocardial infarction following CABG can be classified into graft-related and non-graft–related categories. Early graft dysfunction occurs in up to 3% of cases. Non-graft-related causes include inadequate myocardial protection and embolization. Treatment strategies for type 5 myocardial infarction include conservative medical treatment, PCI, and redo CABG.[78][79][80]
Following mitral valve replacement, left ventricular outflow tract obstruction can occur, characterized by systolic anterior motion of the anterior mitral leaflet. Treatment is approached in a stepwise manner, beginning with beta-blockers, increasing afterload with fluids, allowing hypertension, and, if necessary, proceeding to reoperation. Surgical techniques for reoperation include edge-to-edge repair, posterior leaflet shortening, short neochord, sliding plasty, and ellipsoid excision of the anterior leaflet.[81] Preoperative risk factors for this complication include a thick basal interventricular septum, a small left ventricle, a short distance between the interventricular septum and the mitral leaflet coaptation point, a tall posterior leaflet, and an aorta-mitral angle of less than 120 degrees.[82][83]
Postoperative pain management is crucial in cardiac surgery due to the intense stress and discomfort associated with these procedures. Ensuring patient comfort and calmness is vital for overall well-being, as it supports the immune response to the new graft and ensures the proper functioning of the heart, which in turn impacts the health of all other organs in the body. Effective postoperative pain management in cardiac patients is crucial for both medical professionals and patients, as it can significantly impact recovery and survival. Research shows that cardiac patients often experience their most intense postoperative pain about an hour after extubation. During this period, the highest doses of analgesics are typically administered to manage pain effectively. Pain intensity generally decreases over time, reaching its lowest point approximately an hour after the patient is transferred from the ICU to the ward.[84]
A range of early mobilization strategies is available for post-surgery patients, and while many have proven effective in enhancing recovery, optimal protocols are still under investigation. Early mobilization is crucial for improving outcomes after cardiac surgery and is now standard practice in many hospitals. This approach has been shown to safely and effectively enhance tissue perfusion, preserve muscle strength and mass, reduce the risk of pulmonary complications, shorten hospital stays, improve quality of life, and decrease mortality rates. Additionally, early mobilization has been found to reduce the incidence of delirium, a significant contributor to cognitive impairment associated with ICU stays.[85]
After a sternotomy, patients are typically advised to restrict certain activities to allow the sternum sufficient time to heal and prevent complications from physical exertion. These guidelines, often referred to as "sternal precautions," generally include avoiding lifting, pushing, or pulling objects weighing more than 5 to 10 pounds, driving, or using the arms to assist with sitting or standing. Patients are also encouraged to protect their chest by crossing their arms over it when moving or coughing. These precautions are usually recommended for up to 12 weeks post-surgery until the sternum fully recovers. However, some experts have raised concerns that these restrictions may be overly limiting, potentially leading to issues such as muscle atrophy and difficulty resuming daily activities.
A new movement protocol, "Keep Your Move in the Tube," is designed for patients recovering from sternotomy. This focuses on limiting arm extension to reduce strain on the healing sternum. The protocol emphasizes minimizing humeral movement to avoid tension on the surgical site. This approach is rooted in ergonomics and emphasizes patient education rather than strict directives. This encourages patients to keep their upper arms close to their body, as if modifying their movements within an imaginary tube around the torso. This helps avoid placing excessive stress on the sternum while allowing for functional movement.[86] Fever, edema, and increased inflammatory markers are commonly observed in postoperative patients, making it challenging to differentiate between confirmed infections and evolving sepsis.[87] The time course can give additional information. If signs and symptoms of infection appear after the second or third postoperative day, further investigation for infection should be initiated.[88]
Perioperative antibiotic prophylaxis is essential to reduce the risk of postoperative infections. Guidelines generally recommend administering cephalosporins during the 24 to 48-hour perioperative period. Fortunately, deep sternal wound infection is a rare complication of cardiac surgery, occurring in 0.4% to 4% of cases. However, if left untreated, it can progress to mediastinitis, which carries a significant mortality risk. Treatment for deep sternal wound infection involves pathogen-specific antibiotics (with common strains including Staphylococcus aureus or S epidermidis, often treated with clindamycin or according to resistance patterns), surgical exploration, and negative-pressure wound therapy.
The exact cause of postoperative cognitive decline remains unclear but is believed to be related to the body's stress and inflammatory responses to surgery and anesthesia. Postoperative cognitive impairment involves a reduction in the ability to orient oneself, focus, perceive surroundings, maintain consciousness, and make decisions. Risk factors for developing this condition include advanced age, female gender, significant blood loss, and elevated creatinine levels following surgery. Cognitive impairment is a common complication after surgery, with patients undergoing CABG being particularly vulnerable. A systematic review and meta-analysis revealed that cognitive impairment was observed in over 40% of patients within the first 4 days after CABG surgery. This rate decreased to about 25% at the 1-year mark but increased again to around 40% between 1 and 5 years after surgery. In the long term, beyond 5 years post-surgery, cognitive impairment was reported in 16% of patients—a rate notably lower than other long-term estimates, likely due to patient attrition and mortality during the follow-up period.[85][89]
Although rare, coronary obstruction is a potentially devastating complication of TAVR, most frequently occurring at the left coronary artery ostium. Detection can be challenging, as some patients may not exhibit noticeable clinical symptoms. Research indicates that a significant increase in peak diastolic flow velocity in the left main coronary artery is associated with substantial stenosis in these lesions.[90] Depending on hemodynamic stability, the patient's symptoms, and ECG findings, PCI or surgical revascularization may be indicated. If a coronary ostial iatrogenic injury occurs during surgical AVR, it is generally preferable to perform surgical revascularization rather than attempt to repair or reconstruct the coronary ostium.
Clinical Significance
Cardiac surgery is crucial for cardiovascular health, addressing the growing prevalence of cardiovascular diseases driven by epidemiologic transitions, such as atherosclerosis, hypertension, and lifestyle risk factors. In the United States, cardiac surgery accounts for 1% to 2% of the healthcare budget, with an average inpatient cost of $40,000, totaling approximately $20 billion. The rising demand for specialized healthcare professionals in cardiology and cardiac surgery underscores the need for increased expertise in these fields.[91]
Media
(Click Image to Enlarge)
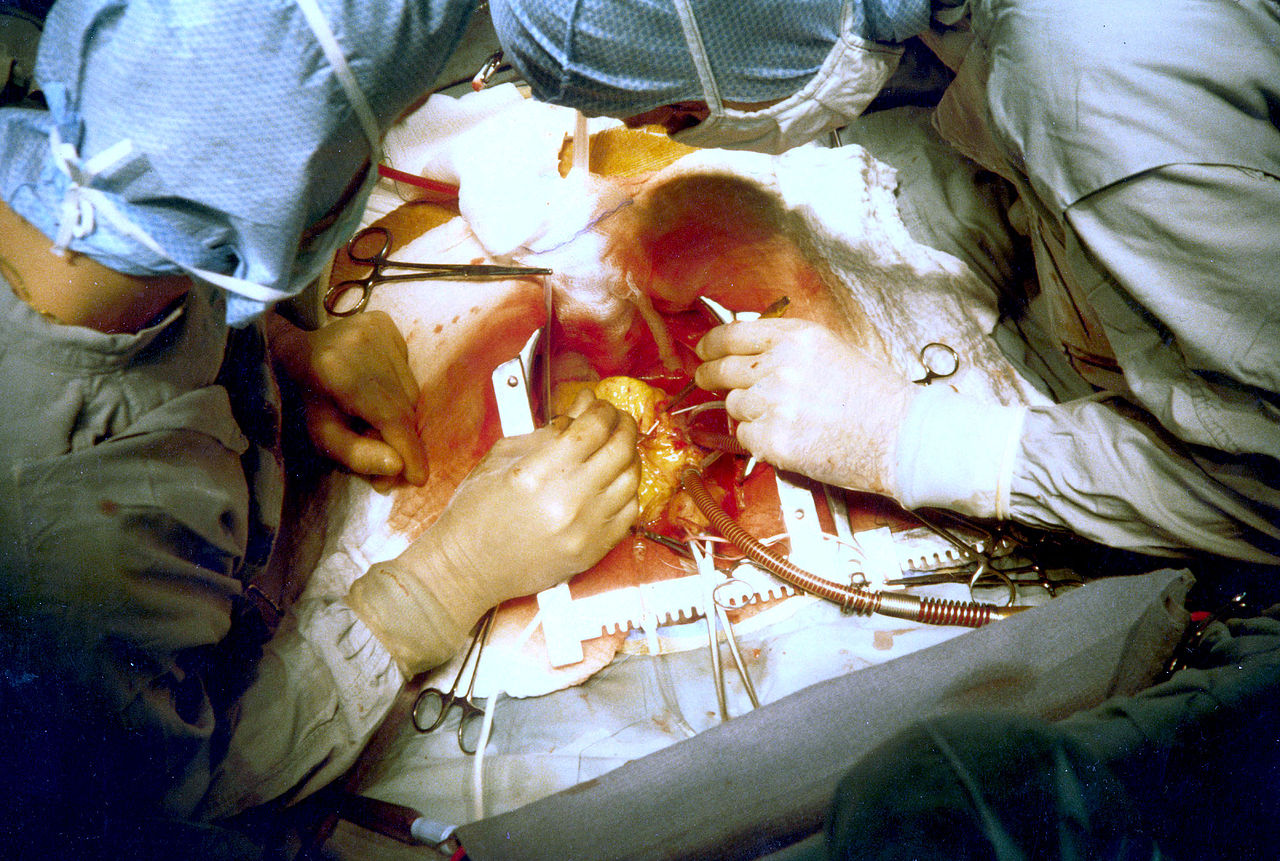
Coronary Artery Bypass Surgery. The image captures a moment during cardiac surgery where 2 surgeons are seen performing coronary artery bypass grafting.
PhilippN, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Aris A. Francisco Romero, the first heart surgeon. The Annals of thoracic surgery. 1997 Sep:64(3):870-1 [PubMed PMID: 9307502]
Braile DM, Godoy MF. History of heart surgery in the world. 1996. Revista brasileira de cirurgia cardiovascular : orgao oficial da Sociedade Brasileira de Cirurgia Cardiovascular. 2012 Jan-Mar:27(1):125-36 [PubMed PMID: 22729311]
Weisse AB. Cardiac surgery: a century of progress. Texas Heart Institute journal. 2011:38(5):486-90 [PubMed PMID: 22163121]
Richenbacher WE, Myers JL, Waldhausen JA. Current status of cardiac surgery: a 40 year review. Journal of the American College of Cardiology. 1989 Sep:14(3):535-44 [PubMed PMID: 2671092]
Hessel EA 2nd. A Brief History of Cardiopulmonary Bypass. Seminars in cardiothoracic and vascular anesthesia. 2014 Jun:18(2):87-100. doi: 10.1177/1089253214530045. Epub 2014 Apr 10 [PubMed PMID: 24728884]
Beck CS. THE DEVELOPMENT OF A NEW BLOOD SUPPLY TO THE HEART BY OPERATION. Annals of surgery. 1935 Nov:102(5):801-13 [PubMed PMID: 17856670]
VINEBERG A. Coronary vascular anastomoses by internal mammary arter implantation. Canadian Medical Association journal. 1958 Jun 1:78(11):871-9 [PubMed PMID: 13536944]
Konstantinov IE. Robert H. Goetz: the surgeon who performed the first successful clinical coronary artery bypass operation. The Annals of thoracic surgery. 2000 Jun:69(6):1966-72 [PubMed PMID: 10892969]
Level 3 (low-level) evidenceSTARR A, EDWARDS ML. Mitral replacement: clinical experience with a ball-valve prosthesis. Annals of surgery. 1961 Oct:154(4):726-40 [PubMed PMID: 13916361]
Lillehei CW, Varco RL, Cohen M, Warden HE, Gott VL, DeWall RA, Patton C, Moller JH. The first open heart corrections of tetralogy of Fallot. A 26-31 year follow-up of 106 patients. Annals of surgery. 1986 Oct:204(4):490-502 [PubMed PMID: 3767482]
Level 3 (low-level) evidenceBROCK RC. Pulmonary valvulotomy for the relief of congenital pulmonary stenosis; report of three cases. British medical journal. 1948 Jun 12:1(4562):1121-6 [PubMed PMID: 18865959]
Level 3 (low-level) evidenceAquilina O. A brief history of cardiac pacing. Images in paediatric cardiology. 2006 Apr:8(2):17-81 [PubMed PMID: 22368662]
DiBardino DJ. The history and development of cardiac transplantation. Texas Heart Institute journal. 1999:26(3):198-205 [PubMed PMID: 10524743]
Level 3 (low-level) evidenceNguyen TC, George I. Beyond the hammer: the future of cardiothoracic surgery. The Journal of thoracic and cardiovascular surgery. 2015 Mar:149(3):675-7. doi: 10.1016/j.jtcvs.2014.11.091. Epub 2014 Dec 4 [PubMed PMID: 25623909]
Mullany D, Shekar K, Platts D, Fraser J. The rapidly evolving use of extracorporeal life support (ECLS) in adults. Heart, lung & circulation. 2014 Nov:23(11):1091-2. doi: 10.1016/j.hlc.2014.04.009. Epub 2014 Apr 24 [PubMed PMID: 25070684]
Level 3 (low-level) evidenceParissis H. Cardiac surgery: what the future holds? Journal of cardiothoracic surgery. 2011 Jul 27:6():93. doi: 10.1186/1749-8090-6-93. Epub 2011 Jul 27 [PubMed PMID: 21794111]
Level 3 (low-level) evidenceDrury NE, Nashef SA. Outcomes of cardiac surgery in the elderly. Expert review of cardiovascular therapy. 2006 Jul:4(4):535-42 [PubMed PMID: 16918272]
Pierri MD, Capestro F, Zingaro C, Torracca L. The changing face of cardiac surgery patients: an insight into a Mediterranean region. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2010 Oct:38(4):407-13. doi: 10.1016/j.ejcts.2010.02.040. Epub [PubMed PMID: 20399675]
Level 2 (mid-level) evidenceLeiva EH, Carreño M, Bucheli FR, Bonfanti AC, Umaña JP, Dennis RJ. Factors associated with delayed cardiac tamponade after cardiac surgery. Annals of cardiac anaesthesia. 2018 Apr-Jun:21(2):158-166. doi: 10.4103/aca.ACA_147_17. Epub [PubMed PMID: 29652277]
Sievers HH, Hemmer W, Beyersdorf F, Moritz A, Moosdorf R, Lichtenberg A, Misfeld M, Charitos EI, Working Group for Aortic Valve Surgery of German Society of Thoracic and Cardiovascular Surgery. The everyday used nomenclature of the aortic root components: the tower of Babel? European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2012 Mar:41(3):478-82. doi: 10.1093/ejcts/ezr093. Epub 2011 Dec 1 [PubMed PMID: 22345173]
Parsa CJ, Shaw LK, Rankin JS, Daneshmand MA, Gaca JG, Milano CA, Glower DD, Smith PK. Twenty-five-year outcomes after multiple internal thoracic artery bypass. The Journal of thoracic and cardiovascular surgery. 2013 Apr:145(4):970-975. doi: 10.1016/j.jtcvs.2012.11.093. Epub 2013 Feb 10 [PubMed PMID: 23402687]
Puskas JD, Yanagawa B, Taggart DP. Advancing the State of the Art in Surgical Coronary Revascularization. The Annals of thoracic surgery. 2016 Feb:101(2):419-21. doi: 10.1016/j.athoracsur.2015.10.046. Epub [PubMed PMID: 26777919]
Maganti K, Rigolin VH, Sarano ME, Bonow RO. Valvular heart disease: diagnosis and management. Mayo Clinic proceedings. 2010 May:85(5):483-500. doi: 10.4065/mcp.2009.0706. Epub [PubMed PMID: 20435842]
Thourani VH, Ailawadi G, Szeto WY, Dewey TM, Guyton RA, Mack MJ, Kron IL, Kilgo P, Bavaria JE. Outcomes of surgical aortic valve replacement in high-risk patients: a multiinstitutional study. The Annals of thoracic surgery. 2011 Jan:91(1):49-55; discussion 55-6. doi: 10.1016/j.athoracsur.2010.09.040. Epub [PubMed PMID: 21172485]
Level 2 (mid-level) evidenceHolmes DR Jr, Nishimura RA, Grover FL, Brindis RG, Carroll JD, Edwards FH, Peterson ED, Rumsfeld JS, Shahian DM, Thourani VH, Tuzcu EM, Vemulapalli S, Hewitt K, Michaels J, Fitzgerald S, Mack MJ, STS/ACC TVT Registry. Annual Outcomes With Transcatheter Valve Therapy: From the STS/ACC TVT Registry. Journal of the American College of Cardiology. 2015 Dec 29:66(25):2813-2823. doi: 10.1016/j.jacc.2015.10.021. Epub 2015 Nov 30 [PubMed PMID: 26652232]
Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Brown DL, Block PC, Guyton RA, Pichard AD, Bavaria JE, Herrmann HC, Douglas PS, Petersen JL, Akin JJ, Anderson WN, Wang D, Pocock S, PARTNER Trial Investigators. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. The New England journal of medicine. 2010 Oct 21:363(17):1597-607. doi: 10.1056/NEJMoa1008232. Epub 2010 Sep 22 [PubMed PMID: 20961243]
Level 1 (high-level) evidenceZou Q, Wei Z, Sun S. Complications in transcatheter aortic valve replacement: A comprehensive analysis and management strategies. Current problems in cardiology. 2024 May:49(5):102478. doi: 10.1016/j.cpcardiol.2024.102478. Epub 2024 Mar 2 [PubMed PMID: 38437930]
O'Gara PT, Grayburn PA, Badhwar V, Afonso LC, Carroll JD, Elmariah S, Kithcart AP, Nishimura RA, Ryan TJ, Schwartz A, Stevenson LW. 2017 ACC Expert Consensus Decision Pathway on the Management of Mitral Regurgitation: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. Journal of the American College of Cardiology. 2017 Nov 7:70(19):2421-2449. doi: 10.1016/j.jacc.2017.09.019. Epub 2017 Oct 18 [PubMed PMID: 29055505]
Level 3 (low-level) evidenceArgulian E, Borer JS, Messerli FH. Misconceptions and Facts About Mitral Regurgitation. The American journal of medicine. 2016 Sep:129(9):919-23. doi: 10.1016/j.amjmed.2016.03.010. Epub 2016 Apr 5 [PubMed PMID: 27059381]
Unger P, Clavel MA, Lindman BR, Mathieu P, Pibarot P. Pathophysiology and management of multivalvular disease. Nature reviews. Cardiology. 2016 Jul:13(7):429-40. doi: 10.1038/nrcardio.2016.57. Epub 2016 Apr 28 [PubMed PMID: 27121305]
Huttin O, Voilliot D, Mandry D, Venner C, Juillière Y, Selton-Suty C. All you need to know about the tricuspid valve: Tricuspid valve imaging and tricuspid regurgitation analysis. Archives of cardiovascular diseases. 2016 Jan:109(1):67-80. doi: 10.1016/j.acvd.2015.08.007. Epub 2015 Dec 23 [PubMed PMID: 26711544]
Dreyfus GD. Functional tricuspid pathology: To treat or not to treat? That is the question. The Journal of thoracic and cardiovascular surgery. 2017 Jul:154(1):123-124. doi: 10.1016/j.jtcvs.2017.03.015. Epub 2017 Mar 10 [PubMed PMID: 28365014]
Calafiore AM, Gallina S, Iacò AL, Contini M, Bivona A, Gagliardi M, Bosco P, Di Mauro M. Mitral valve surgery for functional mitral regurgitation: should moderate-or-more tricuspid regurgitation be treated? a propensity score analysis. The Annals of thoracic surgery. 2009 Mar:87(3):698-703. doi: 10.1016/j.athoracsur.2008.11.028. Epub [PubMed PMID: 19231373]
Level 2 (mid-level) evidenceTaramasso M, Vanermen H, Maisano F, Guidotti A, La Canna G, Alfieri O. The growing clinical importance of secondary tricuspid regurgitation. Journal of the American College of Cardiology. 2012 Feb 21:59(8):703-10. doi: 10.1016/j.jacc.2011.09.069. Epub [PubMed PMID: 22340261]
McCarthy PM. Evolving Approaches to Tricuspid Valve Surgery: Moving To Europe? Journal of the American College of Cardiology. 2015 May 12:65(18):1939-40 [PubMed PMID: 25936266]
Unger P, Rosenhek R, Dedobbeleer C, Berrebi A, Lancellotti P. Management of multiple valve disease. Heart (British Cardiac Society). 2011 Feb:97(4):272-7. doi: 10.1136/hrt.2010.212282. Epub 2010 Dec 13 [PubMed PMID: 21156677]
Rousse N, Juthier F, Pinçon C, Hysi I, Banfi C, Robin E, Fayad G, Jegou B, Prat A, Vincentelli A. ECMO as a bridge to decision: Recovery, VAD, or heart transplantation? International journal of cardiology. 2015:187():620-7. doi: 10.1016/j.ijcard.2015.03.283. Epub 2015 Mar 20 [PubMed PMID: 25863737]
Fang JC. Rise of the machines--left ventricular assist devices as permanent therapy for advanced heart failure. The New England journal of medicine. 2009 Dec 3:361(23):2282-5. doi: 10.1056/NEJMe0910394. Epub 2009 Nov 17 [PubMed PMID: 19920052]
Stone ME, Pawale A, Ramakrishna H, Weiner MM. Implantable Left Ventricular Assist Device Therapy-Recent Advances and Outcomes. Journal of cardiothoracic and vascular anesthesia. 2018 Aug:32(4):2019-2028. doi: 10.1053/j.jvca.2017.11.003. Epub 2017 Nov 4 [PubMed PMID: 29338999]
Level 3 (low-level) evidencePinney SP, Anyanwu AC, Lala A, Teuteberg JJ, Uriel N, Mehra MR. Left Ventricular Assist Devices for Lifelong Support. Journal of the American College of Cardiology. 2017 Jun 13:69(23):2845-2861. doi: 10.1016/j.jacc.2017.04.031. Epub [PubMed PMID: 28595702]
Slaughter MS, Rogers JG, Milano CA, Russell SD, Conte JV, Feldman D, Sun B, Tatooles AJ, Delgado RM 3rd, Long JW, Wozniak TC, Ghumman W, Farrar DJ, Frazier OH, HeartMate II Investigators. Advanced heart failure treated with continuous-flow left ventricular assist device. The New England journal of medicine. 2009 Dec 3:361(23):2241-51. doi: 10.1056/NEJMoa0909938. Epub 2009 Nov 17 [PubMed PMID: 19920051]
Level 1 (high-level) evidenceHein OV, Birnbaum J, Wernecke K, England M, Konertz W, Spies C. Prolonged intensive care unit stay in cardiac surgery: risk factors and long-term-survival. The Annals of thoracic surgery. 2006 Mar:81(3):880-5 [PubMed PMID: 16488688]
Level 2 (mid-level) evidenceAzarfarin R, Ashouri N, Totonchi Z, Bakhshandeh H, Yaghoubi A. Factors influencing prolonged ICU stay after open heart surgery. Research in cardiovascular medicine. 2014 Nov:3(4):e20159. doi: 10.5812/cardiovascmed.20159. Epub 2014 Oct 14 [PubMed PMID: 25785249]
Shahian DM, O'Brien SM, Filardo G, Ferraris VA, Haan CK, Rich JB, Normand SL, DeLong ER, Shewan CM, Dokholyan RS, Peterson ED, Edwards FH, Anderson RP, Society of Thoracic Surgeons Quality Measurement Task Force. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 1--coronary artery bypass grafting surgery. The Annals of thoracic surgery. 2009 Jul:88(1 Suppl):S2-22. doi: 10.1016/j.athoracsur.2009.05.053. Epub [PubMed PMID: 19559822]
Carl M, Alms A, Braun J, Dongas A, Erb J, Goetz A, Goepfert M, Gogarten W, Grosse J, Heller AR, Heringlake M, Kastrup M, Kroener A, Loer SA, Marggraf G, Markewitz A, Reuter D, Schmitt DV, Schirmer U, Wiesenack C, Zwissler B, Spies C. S3 guidelines for intensive care in cardiac surgery patients: hemodynamic monitoring and cardiocirculary system. German medical science : GMS e-journal. 2010 Jun 15:8():Doc12. doi: 10.3205/000101. Epub 2010 Jun 15 [PubMed PMID: 20577643]
KIRKLIN JW, DONALD DE, HARSHBARGER HG, HETZEL PS, PATRICK RT, SWAN HJ, WOOD EH. Studies in extracorporeal circulation. I. Applicability of Gibbon-type pump-oxygenator to human intracardiac surgery: 40 cases. Annals of surgery. 1956 Jul:144(1):2-8 [PubMed PMID: 13327835]
Level 3 (low-level) evidenceSugita J, Fujiu K. Systemic Inflammatory Stress Response During Cardiac Surgery. International heart journal. 2018:59(3):457-459. doi: 10.1536/ihj.18-210. Epub [PubMed PMID: 29848891]
Asimakopoulos G. Systemic inflammation and cardiac surgery: an update. Perfusion. 2001 Sep:16(5):353-60 [PubMed PMID: 11565890]
Level 3 (low-level) evidenceTatoulis J, Rice S, Davis P, Goldblatt JC, Marasco S. Patterns of postoperative systemic vascular resistance in a randomized trial of conventional on-pump versus off-pump coronary artery bypass graft surgery. The Annals of thoracic surgery. 2006 Oct:82(4):1436-44 [PubMed PMID: 16996948]
Level 1 (high-level) evidenceRossaint J, Berger C, Van Aken H, Scheld HH, Zahn PK, Rukosujew A, Zarbock A. Cardiopulmonary bypass during cardiac surgery modulates systemic inflammation by affecting different steps of the leukocyte recruitment cascade. PloS one. 2012:7(9):e45738. doi: 10.1371/journal.pone.0045738. Epub 2012 Sep 19 [PubMed PMID: 23029213]
Murphy DA, Hockings LE, Andrews RK, Aubron C, Gardiner EE, Pellegrino VA, Davis AK. Extracorporeal membrane oxygenation-hemostatic complications. Transfusion medicine reviews. 2015 Apr:29(2):90-101. doi: 10.1016/j.tmrv.2014.12.001. Epub 2014 Dec 18 [PubMed PMID: 25595476]
Chaikof EL. The development of prosthetic heart valves--lessons in form and function. The New England journal of medicine. 2007 Oct 4:357(14):1368-71 [PubMed PMID: 17914037]
Rahimtoola SH. Choice of prosthetic heart valve in adults an update. Journal of the American College of Cardiology. 2010 Jun 1:55(22):2413-26. doi: 10.1016/j.jacc.2009.10.085. Epub [PubMed PMID: 20510209]
Level 3 (low-level) evidenceMiller CL, Kocher M, Koweek LH, Zwischenberger BA. Use of computed tomography (CT) for preoperative planning in patients undergoing coronary artery bypass grafting (CABG). Journal of cardiac surgery. 2022 Dec:37(12):4150-4157. doi: 10.1111/jocs.17000. Epub 2022 Oct 2 [PubMed PMID: 36183391]
Fitchett D, Eikelboom J, Fremes S, Mazer D, Singh S, Bittira B, Brister S, Graham J, Gupta M, Karkouti K, Lee A, Love M, McArthur R, Peterson M, Verma S, Yau T. Dual antiplatelet therapy in patients requiring urgent coronary artery bypass grafting surgery: a position statement of the Canadian Cardiovascular Society. The Canadian journal of cardiology. 2009 Dec:25(12):683-9 [PubMed PMID: 19960127]
Sousa-Uva M, Storey R, Huber K, Falk V, Leite-Moreira AF, Amour J, Al-Attar N, Ascione R, Taggart D, Collet JP, ESC Working Group on Cardiovascular Surgery and ESC Working Group on Thrombosis. Expert position paper on the management of antiplatelet therapy in patients undergoing coronary artery bypass graft surgery. European heart journal. 2014 Jun 14:35(23):1510-4. doi: 10.1093/eurheartj/ehu158. Epub 2014 Apr 18 [PubMed PMID: 24748565]
Capodanno D, Angiolillo DJ. Management of antiplatelet therapy in patients with coronary artery disease requiring cardiac and noncardiac surgery. Circulation. 2013 Dec 24:128(25):2785-98. doi: 10.1161/CIRCULATIONAHA.113.003675. Epub [PubMed PMID: 24366588]
Nagashima Z, Tsukahara K, Uchida K, Hibi K, Karube N, Ebina T, Imoto K, Kimura K, Umemura S. Impact of preoperative dual antiplatelet therapy on bleeding complications in patients with acute coronary syndromes who undergo urgent coronary artery bypass grafting. Journal of cardiology. 2017 Jan:69(1):156-161. doi: 10.1016/j.jjcc.2016.02.013. Epub 2016 Mar 15 [PubMed PMID: 26987791]
Dalén M, Ivert T, Holzmann MJ, Sartipy U. Long-term survival after off-pump coronary artery bypass surgery: a Swedish nationwide cohort study. The Annals of thoracic surgery. 2013 Dec:96(6):2054-60. doi: 10.1016/j.athoracsur.2013.07.014. Epub 2013 Sep 25 [PubMed PMID: 24075498]
Level 2 (mid-level) evidencePuskas JD, Thourani VH, Kilgo P, Cooper W, Vassiliades T, Vega JD, Morris C, Chen E, Schmotzer BJ, Guyton RA, Lattouf OM. Off-pump coronary artery bypass disproportionately benefits high-risk patients. The Annals of thoracic surgery. 2009 Oct:88(4):1142-7. doi: 10.1016/j.athoracsur.2009.04.135. Epub [PubMed PMID: 19766798]
Level 2 (mid-level) evidenceBonaros N, Schachner T, Wiedemann D, Weidinger F, Lehr E, Zimrin D, Friedrich G, Bonatti J. Closed chest hybrid coronary revascularization for multivessel disease - current concepts and techniques from a two-center experience. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2011 Oct:40(4):783-7. doi: 10.1016/j.ejcts.2011.01.055. Epub 2011 Apr 3 [PubMed PMID: 21459599]
Verhaegh AJ, Accord RE, van Garsse L, Maessen JG. Hybrid coronary revascularization as a safe, feasible, and viable alternative to conventional coronary artery bypass grafting: what is the current evidence? Minimally invasive surgery. 2013:2013():142616. doi: 10.1155/2013/142616. Epub 2013 Apr 3 [PubMed PMID: 23691303]
Mentzer RM Jr. Myocardial protection in heart surgery. Journal of cardiovascular pharmacology and therapeutics. 2011 Sep-Dec:16(3-4):290-7. doi: 10.1177/1074248411410318. Epub [PubMed PMID: 21821531]
Level 3 (low-level) evidenceLi Y, Lin H, Zhao Y, Li Z, Liu D, Wu X, Ji B, Gao B. Del Nido Cardioplegia for Myocardial Protection in Adult Cardiac Surgery: A Systematic Review and Meta-Analysis. ASAIO journal (American Society for Artificial Internal Organs : 1992). 2018 May/Jun:64(3):360-367. doi: 10.1097/MAT.0000000000000652. Epub [PubMed PMID: 28863040]
Level 1 (high-level) evidenceVaage J. Retrograde cardioplegia: when and how. A review. Scandinavian journal of thoracic and cardiovascular surgery. Supplementum. 1993:41():59-66 [PubMed PMID: 8184295]
Yamamoto H, Yamamoto F. Myocardial protection in cardiac surgery: a historical review from the beginning to the current topics. General thoracic and cardiovascular surgery. 2013 Sep:61(9):485-96. doi: 10.1007/s11748-013-0279-4. Epub 2013 Jul 23 [PubMed PMID: 23877427]
Abah U, Large S. Stroke prevention in cardiac surgery. Interactive cardiovascular and thoracic surgery. 2012 Jul:15(1):155-7. doi: 10.1093/icvts/ivs012. Epub 2012 Apr 21 [PubMed PMID: 22523135]
Grogan K, Stearns J, Hogue CW. Brain protection in cardiac surgery. Anesthesiology clinics. 2008 Sep:26(3):521-38. doi: 10.1016/j.anclin.2008.03.003. Epub [PubMed PMID: 18765221]
Lelis RG, Auler Júnior JO. [Pathophysiology of neurological injuries during heart surgery: aspectos fisiopatológicos.]. Revista brasileira de anestesiologia. 2004 Aug:54(4):607-17 [PubMed PMID: 19471768]
DeBakey ME. The development of vascular surgery. American journal of surgery. 1979 Jun:137(6):697-738 [PubMed PMID: 313164]
Livesay JJ, Messner GN, Vaughn WK. Milestones in the treatment of aortic aneurysm: Denton A. Cooley, MD, and the Texas Heart Institute. Texas Heart Institute journal. 2005:32(2):130-4 [PubMed PMID: 16107099]
Salazar JD, Wityk RJ, Grega MA, Borowicz LM, Doty JR, Petrofski JA, Baumgartner WA. Stroke after cardiac surgery: short- and long-term outcomes. The Annals of thoracic surgery. 2001 Oct:72(4):1195-201; discussion 1201-2 [PubMed PMID: 11603436]
McKhann GM, Grega MA, Borowicz LM Jr, Baumgartner WA, Selnes OA. Stroke and encephalopathy after cardiac surgery: an update. Stroke. 2006 Feb:37(2):562-71 [PubMed PMID: 16373636]
Crosina J, Lerner J, Ho J, Tangri N, Komenda P, Hiebert B, Choi N, Arora RC, Rigatto C. Improving the Prediction of Cardiac Surgery-Associated Acute Kidney Injury. Kidney international reports. 2017 Mar:2(2):172-179. doi: 10.1016/j.ekir.2016.10.003. Epub 2016 Oct 21 [PubMed PMID: 29142955]
Lomivorotov VV, Efremov SM, Karaskov AM. Pharmacokinetics of Magnesium in Cardiac Surgery: Implications for Prophylaxis Against Atrial Fibrillation. Journal of cardiothoracic and vascular anesthesia. 2018 Jun:32(3):1295-1296. doi: 10.1053/j.jvca.2017.09.023. Epub 2017 Sep 20 [PubMed PMID: 29217237]
Werdan K, Ruß M, Buerke M, Delle-Karth G, Geppert A, Schöndube FA, German Cardiac Society, German Society of Intensive Care and Emergency Medicine, German Society for Thoracic and Cardiovascular Surgery, (Austrian Society of Internal and General Intensive Care Medicine, German Interdisciplinary Association of Intensive Care and Emergency Medicine, Austrian Society of Cardiology, German Society of Anaesthesiology and Intensive Care Medicine, German Society of Preventive Medicine and Rehabilitation. Cardiogenic shock due to myocardial infarction: diagnosis, monitoring and treatment: a German-Austrian S3 Guideline. Deutsches Arzteblatt international. 2012 May:109(19):343-51. doi: 10.3238/arztebl.2012.0343. Epub 2012 May 11 [PubMed PMID: 22675405]
Mohamed MO, Hirji S, Mohamed W, Percy E, Braidley P, Chung J, Aranki S, Mamas MA. Incidence and predictors of postoperative ischemic stroke after coronary artery bypass grafting. International journal of clinical practice. 2021 May:75(5):e14067. doi: 10.1111/ijcp.14067. Epub 2021 Feb 6 [PubMed PMID: 33534146]
Laflamme M, DeMey N, Bouchard D, Carrier M, Demers P, Pellerin M, Couture P, Perrault LP. Management of early postoperative coronary artery bypass graft failure. Interactive cardiovascular and thoracic surgery. 2012 Apr:14(4):452-6. doi: 10.1093/icvts/ivr127. Epub 2012 Jan 5 [PubMed PMID: 22223760]
Level 2 (mid-level) evidenceRedfors B, Généreux P, Witzenbichler B, McAndrew T, Diamond J, Huang X, Maehara A, Weisz G, Mehran R, Kirtane AJ, Stone GW. Percutaneous Coronary Intervention of Saphenous Vein Graft. Circulation. Cardiovascular interventions. 2017 May:10(5):. pii: e004953. doi: 10.1161/CIRCINTERVENTIONS.117.004953. Epub [PubMed PMID: 28495896]
Welsh RC, Granger CB, Westerhout CM, Blankenship JC, Holmes DR Jr, O'Neill WW, Hamm CW, Van de Werf F, Armstrong PW, APEX AMI Investigators. Prior coronary artery bypass graft patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. JACC. Cardiovascular interventions. 2010 Mar:3(3):343-51. doi: 10.1016/j.jcin.2009.12.008. Epub [PubMed PMID: 20298996]
Level 1 (high-level) evidenceVarghese R, Anyanwu AC, Itagaki S, Milla F, Castillo J, Adams DH. Management of systolic anterior motion after mitral valve repair: an algorithm. The Journal of thoracic and cardiovascular surgery. 2012 Apr:143(4 Suppl):S2-7. doi: 10.1016/j.jtcvs.2012.01.063. Epub [PubMed PMID: 22423603]
Level 2 (mid-level) evidenceMiura T, Eishi K, Yamachika S, Hashizume K, Hazama S, Ariyoshi T, Taniguchi S, Izumi K, Hashimoto W, Odate T. Systolic anterior motion after mitral valve repair: predicting factors and management. General thoracic and cardiovascular surgery. 2011 Nov:59(11):737-42. doi: 10.1007/s11748-011-0833-x. Epub 2011 Nov 15 [PubMed PMID: 22083691]
Level 2 (mid-level) evidenceAlfieri O, Lapenna E. Systolic anterior motion after mitral valve repair: where do we stand in 2015? European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2015 Sep:48(3):344-6. doi: 10.1093/ejcts/ezv230. Epub 2015 Jul 4 [PubMed PMID: 26142473]
Jannati M, Attar A. Analgesia and sedation post-coronary artery bypass graft surgery: a review of the literature. Therapeutics and clinical risk management. 2019:15():773-781. doi: 10.2147/TCRM.S195267. Epub 2019 Jun 20 [PubMed PMID: 31417264]
Allahbakhshian A, Khalili AF, Gholizadeh L, Esmealy L. Comparison of early mobilization protocols on postoperative cognitive dysfunction, pain, and length of hospital stay in patients undergoing coronary artery bypass graft surgery: A randomized controlled trial. Applied nursing research : ANR. 2023 Oct:73():151731. doi: 10.1016/j.apnr.2023.151731. Epub 2023 Aug 23 [PubMed PMID: 37722799]
Level 1 (high-level) evidencePark L, Coltman C, Agren H, Colwell S, King-Shier KM. "In the tube" following sternotomy: A quasi-experimental study. European journal of cardiovascular nursing. 2021 Feb 1:20(2):160–166. doi: 10.1177/1474515120951981. Epub [PubMed PMID: 33611341]
Howitt SH, Herring M, Malagon I, McCollum CN, Grant SW. Incidence and outcomes of sepsis after cardiac surgery as defined by the Sepsis-3 guidelines. British journal of anaesthesia. 2018 Mar:120(3):509-516. doi: 10.1016/j.bja.2017.10.018. Epub 2017 Nov 24 [PubMed PMID: 29452807]
Paternoster G, Guarracino F. Sepsis After Cardiac Surgery: From Pathophysiology to Management. Journal of cardiothoracic and vascular anesthesia. 2016 Jun:30(3):773-80. doi: 10.1053/j.jvca.2015.11.009. Epub 2015 Nov 10 [PubMed PMID: 26947713]
Greaves D, Psaltis PJ, Ross TJ, Davis D, Smith AE, Boord MS, Keage HAD. Cognitive outcomes following coronary artery bypass grafting: A systematic review and meta-analysis of 91,829 patients. International journal of cardiology. 2019 Aug 15:289():43-49. doi: 10.1016/j.ijcard.2019.04.065. Epub 2019 Apr 24 [PubMed PMID: 31078353]
Level 1 (high-level) evidenceNomura T, Teruo I, Miyasaka M, Hirose S, Enta Y, Ishii K, Nakashima M, Saigan M, Toki Y, Sakurai M, Munehisa Y, Hata M, Taguri M, Toyoda S, Tada N. Detection of left coronary ostial obstruction during transcatheter aortic valve replacement by coronary flow velocity measurement in the left main trunk by intraoperative transesophageal echocardiography. Journal of cardiology. 2023 Jan:81(1):97-104. doi: 10.1016/j.jjcc.2022.08.009. Epub 2022 Sep 14 [PubMed PMID: 36114119]
Lee JJ, Park NH, Lee KS, Chee HK, Sim SB, Kim MJ, Choi JS, Kim M, Park CS. Projections of Demand for Cardiovascular Surgery and Supply of Surgeons. The Korean journal of thoracic and cardiovascular surgery. 2016 Dec:49(Suppl 1):S37-S43. doi: 10.5090/kjtcs.2016.49.S1.S37. Epub 2016 Dec 5 [PubMed PMID: 28035296]
Authors/Task Force Members, Kunst G, Milojevic M, Boer C, De Somer FMJJ, Gudbjartsson T, van den Goor J, Jones TJ, Lomivorotov V, Merkle F, Ranucci M, Puis L, Wahba A, EACTS/EACTA/EBCP Committee Reviewers, Alston P, Fitzgerald D, Nikolic A, Onorati F, Rasmussen BS, Svenmarker S. 2019 EACTS/EACTA/EBCP guidelines on cardiopulmonary bypass in adult cardiac surgery. British journal of anaesthesia. 2019 Dec:123(6):713-757. doi: 10.1016/j.bja.2019.09.012. Epub 2019 Oct 2 [PubMed PMID: 31585674]