Introduction
Descent of the brows plays a fundamental role in facial aging. During the aging process, the brow becomes ptotic, which may cause lateral upper eyelid hooding with or without visual field deficits. Moreover, patients with these characteristic signs of aging are often perceived by others as appearing fatigued or angry, despite being well-rested and in a good mood.[1] Currently, there exist several well-described surgical means of improving brow aesthetics, ranging from the traditional open approaches to newer endoscopic techniques. While each method has associated benefits and limitations, no clear evidence exists to indicate which type of brow lift surgery is superior.[2] The endoscopic brow lift was first described in the literature by Nicanor Isse in 1994, and since then, it has evolved both in technique and in popularity.[3] More than half of brow rejuvenation procedures today are performed endoscopically, which likely reflects the current trend toward minimally invasive cosmetic surgery.[4] Therefore, the modern aesthetic surgeon should thoroughly understand endoscopic brow lifting, a technique used to produce reliable and lasting brow restoration.[5]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Characteristic Signs of Aging in the Upper Face [6]
- Vertical glabellar lines: caused by the action of the transverse head of the corrugator supercilii muscle (CSM)
- Oblique glabellar lines: caused by the action of the brow depressors, including the oblique head of CSM, depressor supercilii muscle, and medial orbicularis oculi muscle (OOM)
- Transverse dorsal skin lines: caused by the action of the procerus muscle
- Lateral eyebrow ptosis: caused by gravity, galeal fat pad descent, instability of the superficial temporal fascia, and the actions of the CSM (transverse head) and the OOM (lateral portion)
- Pseudo-excess upper eyelid skin (lid hooding): a result of brow ptosis, particularly evident laterally. When the upper eyelid skin overhangs the lash line, it is often referred to as "pseudo-blepharoptosis."
- Transverse forehead skin lines: caused by the action of the frontalis muscle, the sole brow elevator
Structures Requiring Release During Endoscopic Brow Lift
- Zone of adhesion: A 6-mm-wide zone medial to the superior temporal fusion line of the skull where periosteum and galea are fixed to the bone
- Conjoint tendon: The fusion of the galea aponeurotica, superficial and deep temporal fascia, and periosteum (pericranium) within the anterior temporal region at the inferior end of the zone of adhesion. The conjoint tendon functions like a cutaneous retaining ligament
- Arcus marginalis: The fusion of the galea aponeurotica and frontal periosteum at the supraorbital rim, which functions to anchor the brow and acts as the peripheral attachment of the orbital septum
Anatomic Structures at Risk
- Supraorbital nerve: The trunk exits the superior orbit above the medial limbus and forms branches, providing innervation to the frontoparietal skin (deep branch) and upper eyelid (superficial branch). This nerve usually exits the skull through a notch but may traverse a foramen instead in 25 to 33% of patients and may exit through a notch on one side and a foramen on the other.
- Supratrochlear nerve: Located approximately 1 cm medially to the supraorbital nerve or 1.7 cm laterally to the midline, the supratrochlear nerve innervates the skin of the midline glabella, the medial upper eyelid, and a portion of the conjunctiva.
- Temporal branch of the facial nerve (CN VII): The temporal, or frontal, branch provides motor innervation to the musculature of the brow and the superior portion of the orbicularis oculi muscle. As the temporal branch courses superiorly to the zygomatic arch, it runs within or along the undersurface of the temporoparietal fascia. The anticipated path of the temporal branch can be estimated by Pitanguy's line, drawn from a point 5 mm inferior to the tragus to a point 15 mm superior to the lateral taper of the ipsilateral brow.[7]
- Sentinel vein: This perforating vein in the zygomaticotemporal venous system is located approximately 1 cm lateral to the frontozygomatic suture line and predictably falls within 2 mm of the temporal branch of the facial nerve.[8]
- Hair follicles: Alopecia is avoidable with incisions placed parallel to hair follicle orientation, tension-free closure of incision lines, and limited cauterization to the undersurface of hair-bearing areas.
Indications
Indications for Brow Lift Surgery
- Brow ptosis
- Deep rhytids and/or furrows traversing the forehead, glabella, and/or nasal radix
- The appearance of a heavy or redundant forehead or temporal skin
- Pseudo-blepharoptosis and/or visual field restriction
Indications for Endoscopic versus Open Techniques
- Patient preference for a less invasive procedure and/or less visible scarring
- Patient with a short forehead (less than 6 cm from brow to hairline)
Contraindications
Contraindications to Brow Lift Surgery
- Lagophthalmos
- More than 3-4 mm of brow height asymmetry. Because this technique raises the entire forehead as a unit, it is difficult to apply significantly more upward tension to one side compared to the other.
- History of dry-eye symptoms or previous blepharoplasty (increased risk of lagophthalmos)
- Unrealistic patient expectations. In women, the brow should be arched with its highest point between the lateral limbus and lateral canthus, and it should lie just above the supraorbital rim. However, this approach contrasts to working on men whose brows should be flatter and sit at the supraorbital rim. Nevertheless, a standardized ideal eyebrow does not exist; thus, surgeon-patient communication is essential to optimize outcomes.[9]
- Body dysmorphic disorder
Contraindications to Endoscopic Brow Lift Surgery
- Excessive hairline recession (endoscopic brow lifting may raise the hairline slightly)
- Excessively curved forehead and/or frontal bossing (inhibits the passing of endoscopic instruments to the periorbita)
Equipment
Preoperatively
- Alcohol solution or pad (cleanse skin before injection and marking the landmarks and incisions)
- Surgical marker (marking planned incision sites)
- Local anesthesia (such as 1% lidocaine with epinephrine 1:100,000; maximal dosage of lidocaine with epinephrine is 7 mg/kg)
- Tumescent solution (such as 0.1% lidocaine with epinephrine 1:100,0000 and saline)
- Topical antiseptics, such as povidone-iodine
- Corneal shield and lubrication to protect the eyes
Intraoperatively
- Endoscopic equipment (e.g., 5 mm, 30-degree rigid endoscope with retractor/cowling) with a video monitor
- Variety of curved dissectors and periosteal elevators, such as Daniel, Freer, and Ramirez elevators
- Fixation method: multiple options exist, including suture fixation to screws, plates, and bone tunnels, and resorbable tine-fixation devices are also available that engage both the periosteum and the underlying bone.[10]
- Scalpel (#15 blade)
- Forceps (with fine teeth for atraumatic soft tissue handling)
- Facelift scissors (or other dissecting scissors)
- Electrocoagulation/electrocautery device
- Skin hooks and/or small retractors
- Suture (absorbable and nonabsorbable) or staples
Postoperatively
- Petrolatum or antibiotic ointment
- Headwrap materials (non-stick dressing, kerlix wrap, ace wrap)
Personnel
- Surgeon
- Anesthesiologist
- Operating room nurse
- Scrub technician
- Surgical assistant
Preparation
Photographic views should be obtained using a 5-view head series with the patient in a seated and upright position with no facial animation. Close-up views of the eyes (closed/open/upward gaze/lateral gaze) also require documentation.[1]
Landmarks to identify include the supraorbital notch, the proposed highest point of the brow, the course of the frontal branch of the facial nerve, and the sentinel vein.
Incisions are marked. The placement of three frontal hairline incisions (1 median and two paramedian) is 1 cm posterior to the hairline, typically less than 2 cm in length. The paramedian incisions are marked vertically above and slightly medial to the planned highest point of the brow arch. Two temporal incisions are marked parallel and posterior to the temporal hairline on a line drawn from the ala through lateral canthus and extended into the hairline. Shaving is unnecessary and bothersome to patients, although hair ties may be used to control the hair on both sides of the proposed incision sites for improved visualization.
The patient is positioned supine with the endoscope monitor at the foot of the bed, within view of the surgeon.
Local anesthesia is infiltrated along the supraorbital and lateral orbital rims. Tumescent solution is injected subperiosteally from the supraorbital rim to the vertex between the superior temporal lines and then into the superficial temporal spaces bilaterally. The endoscopic brow lift may be performed entirely under local anesthesia; however, general anesthesia or intravenous sedation techniques are recommended to improve patient comfort. When using intravenous sedation, additional nerve blocks of the auriculotemporal and zygomaticotemporal nerves may reduce intra-operative and post-operative pain.
A single dose of intravenous antibiotics is the recommended for infection prophylaxis before the start of the procedure, particularly if implants are to be placed.
Technique or Treatment
The successful endoscopic brow lift requires the surgeon to utilize careful operative techniques, adhere to anatomic dissection planes, and directly visualize specific anatomic structures at key points in the procedure. Herein we present safe and reliable endoscopic brow lift techniques.[10][11][1]
The surgeon makes midline and paramedian incisions through all layers of the scalp, down to the cranium. The temporal incisions only proceed down to the fascia of the temporalis muscle (deep temporal fascia).
Using a curved periosteal elevator, the midline and paramedian ports are used to perform blind dissection (without the endoscope) to develop a full-thickness subperiosteal pocket between the temporal lines. Blind dissection proceeds anteriorly to a point 1 to 2 cm cephalic to the supraorbital rims and anterolaterally along the lateral orbital rims to the lateral canthus.
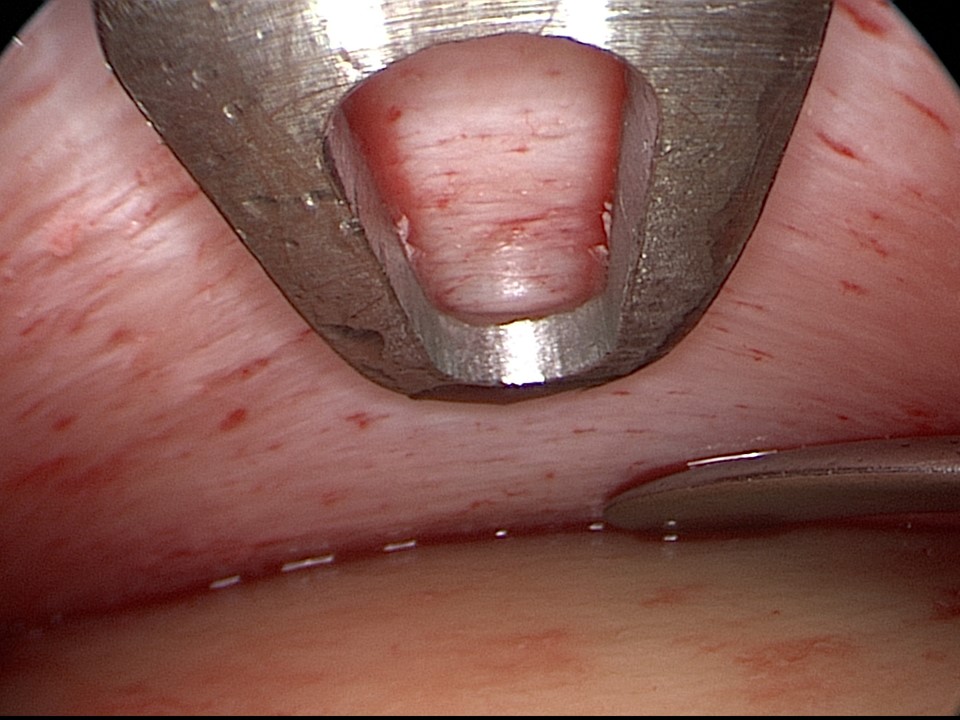
The 30-degree endoscope (inserted through the midline port) and endoscopic instruments (inserted through the paramedian ports) are used to fully release the arcus marginalis while taking care not to violate the supraorbital neurovascular bundles.
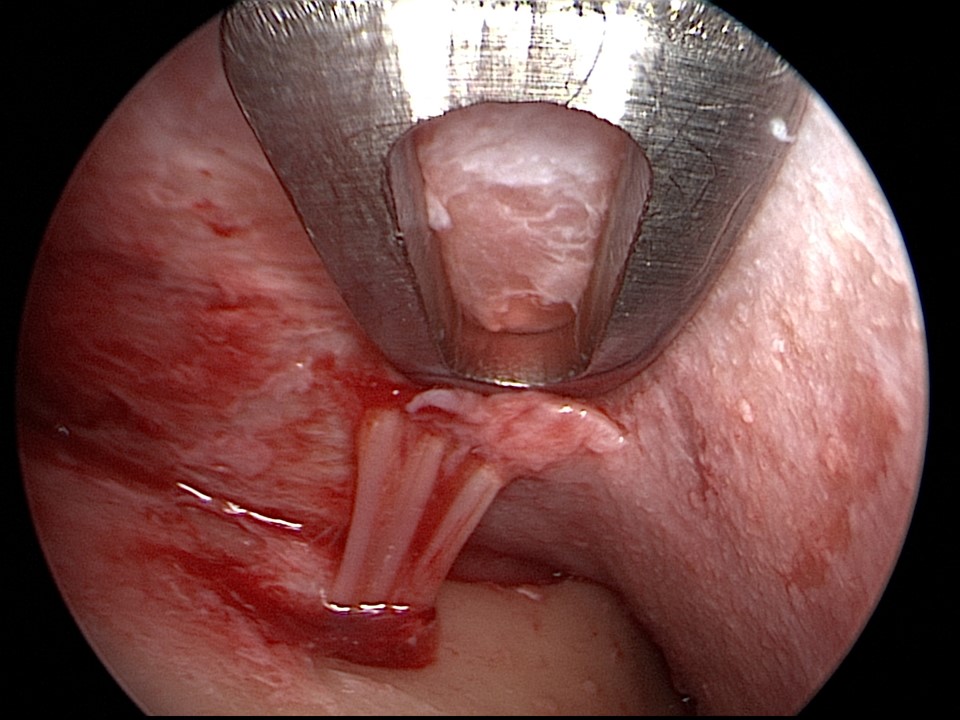
With the completion of periosteum elevation, resection or ablation of the frontalis, corrugators, and procerus muscles may follow if desired, a maneuver typically reserved for patients with deep forehead and glabellar rhytids.[12] Note: Aggressive release of the corrugators has the risk of widening the inter-brow distance (see figure).
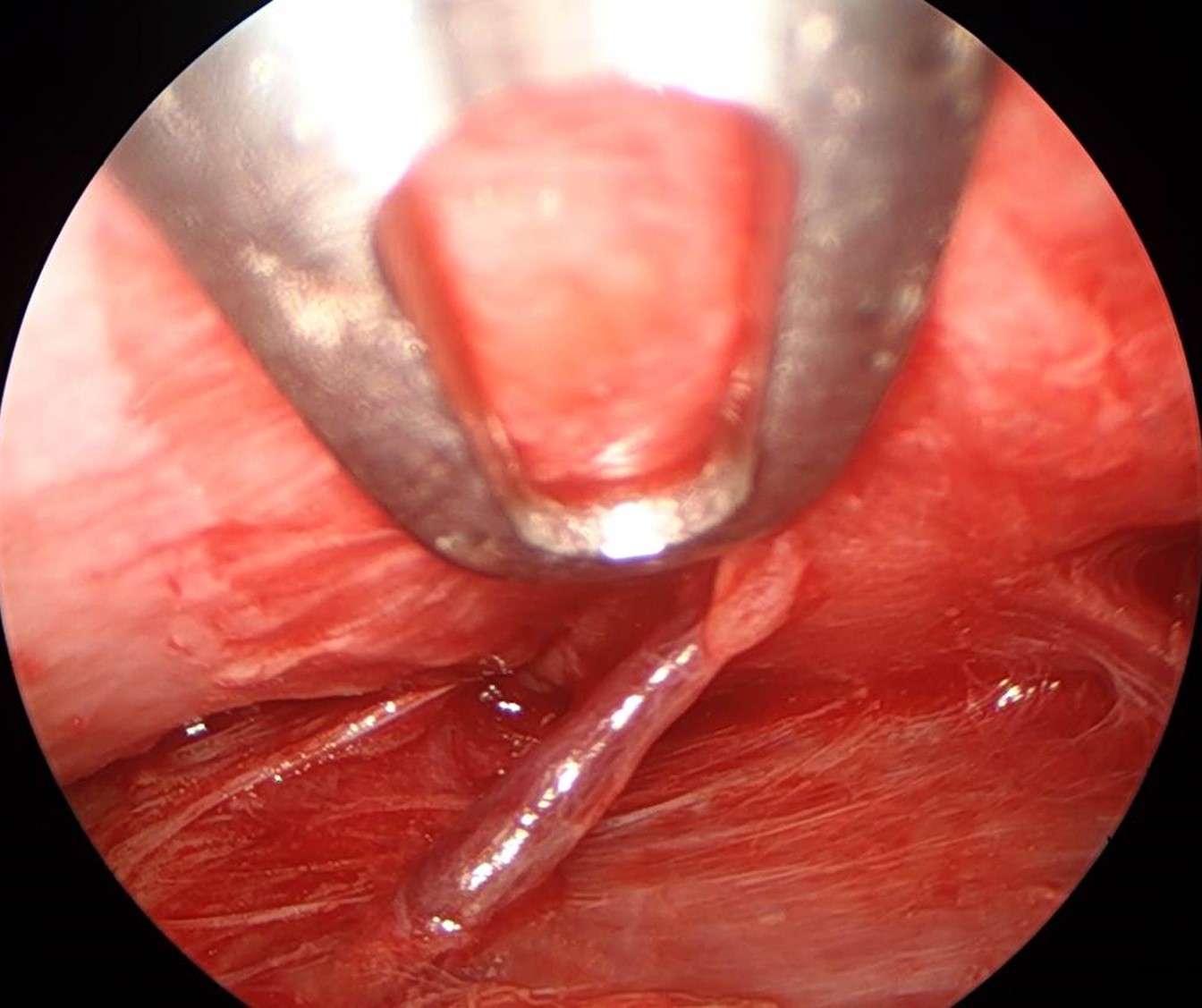
A curved elevator is then introduced via the temporal port to dissect the tissue plane between the temporoparietal fascia (superficial temporal fascia) and the temporalis fascia (deep temporal fascia) that overlies the temporalis muscle. Entering this plane is best performed under direct visualization. The entirety of the superficial temporal space is released anteriorly, posteriorly, and inferiorly to approximately 1 cm above the zygomatic arch to avoid injuring the facial nerve as it crosses the zygoma. The sentinel vein, usually identified 1 cm lateral to the frontozygomatic suture line, should not be cauterized if possible so as to decrease the risk of facial nerve injury. While the vein may appear large on the monitor, the caliber is typically on the order of 1 mm; therefore, if the vein is injured, direct pressure is generally sufficient to stop the bleeding. If cautery is necessary, bipolar forceps on a low setting, such as 10 watts, may be employed, taking care to cauterize only the deep surface and stay away from the temporoparietal fascia.
The lateral and the central dissection cavities are then connected by sharply dividing the zone of adhesion at the superior temporal line, typically accomplished most easily by passing an elevator from lateral to medial. Similarly, the conjoint tendon is then opened above the supraorbital rim and posteriorly until there is a complete connection between the lateral and central dissection pockets.
Fixation is usually accomplished first at the temporal ports and then at the paramedian ports. A large permanent or semi-permanent suture (e.g., 0-0 nylon or polydioxanone) is utilized to affix the temporoparietal fascia to the deep temporalis fascia in a vector that follows a line running from the ala to the lateral canthus. Fixation at the paramedian incision is then performed, which can be accomplished via numerous techniques. Absorbable tissue fixation devices are commonly employed. Holes are drilled in the skull through the paramedian incisions to place the devices bilaterally. The frontal scalp flap is then lifted off the bone and suspended superiorly onto the device prongs with the help of an assistant. This maneuver holds the periosteum in place and sets the height and arch of the brows. Note: In general, approximately 5 mm of vertical relapse should be anticipated depending on the thickness and redundancy of the preoperative forehead. Tunnels may be drilled into the frontal bone, and sutures passed through them to anchor the scalp in a more superior position as well. Some surgeons prefer to place screws at the superior extent of the paramedian incisions and then staple the incisions closed such that the staples pull the scalp back and are held in place against the screws. The screws can then be removed in the clinic six weeks post-operatively.
Scalp incision closure is performed with either skin staples or sutures, and petrolatum or antibiotic ointment is applied. Drains are usually not necessary, and one may use a light forehead wrap placed as a pressure dressing, taking care to avoid placing downward traction on the forehead, which may reduce the amount of lift achieved.
Lastly, if planning a concurrent upper blepharoplasty, the blepharoplasty should only be performed after completing the brow lift because the brow lift decreases upper eyelid skin redundancy and reduces the amount of skin that needs to be excised during blepharoplasty.
Complications
The most common complications of the endoscopic brow lift are paresthesia/dysesthesia, asymmetry, alopecia, lagophthalmos, and the need for revision. Motor nerve injury to the frontal branch of the facial nerve, the most feared complication, is less common. Fortunately, temporary paresis is far more common than permanent paralysis. Other complications include edema, wound dehiscence, eye problems, glabellar irregularity, granuloma, hematoma, infection, pain, palpability of implanted materials (e.g., screws or tines), pruritus, screw exposure, seroma, skin burn, and scar.[13][2]
Nonetheless, patient satisfaction with endoscopic brow lift is high (greater than 98%), and reports of significant complications are rare.[4]
Lastly, while the endoscopic brow lift may possess a lower complication profile compared to the traditional open approaches, open approaches still may provide a more effective or durable lift. There is very little available data on the subject.[14]
Clinical Significance
The endoscopic brow lift aims to restore a more youthful and rested appearance. When performing an endoscopic brow lift, meticulous surgical technique, strict adherence to anatomic dissection planes, and direct visualization at crucial points in the procedure are required to produce a safer, more complete dissection, and ultimately a better outcome and a satisfied patient.
Enhancing Healthcare Team Outcomes
It is imperative to identify the risk factors and perform a thorough assessment of the patient before an endoscopic brow lift. A team approach is an ideal way to limit the complications of this procedure. Prior to surgery, the patient should have the following done:
- Evaluation by a surgeon experienced in selecting the appropriate patient for the surgery
- Evaluation by the primary care physician and anesthesiologist or nurse anesthetist to ensure that the patient is fit for general anesthesia
- Evaluation by the optometrist or ophthalmologist if the patient suffers from dry eyes, blepharoptosis, or lagophthalmos
- Evaluation and monitoring by the pre-, intra-, and postoperative specialty nurses to assist with coordination of care and patient and family education
An interprofessional team of a surgeon, anesthesiologist, surgical assistants, and operative nurses should perform the endoscopic brow lift to ensure the best outcomes. A nurse dedicated to the monitoring of the patient during anesthesia is highly recommended. Pharmacist involvement comes in the form of prophylactic antibiotic verification pre-operatively (e.g., dose, appropriateness of agent selected). Post-operatively, pharmacist recommendations for pain control and corticosteroid dosing are helpful, along with a complete medication reconciliation to ensure no drug-drug interactions. Close follow-up during the initial postoperative period by a wound care nurse and/or clinician experienced in the postoperative care of endoscopic brow lift patients should identify any complications that arise, including hematoma formation. The patient will also require education on avoiding strenuous activity, heavy lifting, or bending over during the first several days post-operatively in order to prevent complications. Only through this type of interprofessional healthcare team approach can outcomes for this procedure be consistently optimized. [Level 5]
Nursing, Allied Health, and Interprofessional Team Interventions
Adequate pain medication is critical, as patients often report severe tension headache-like discomfort for the first day or two postoperatively. Ice packs should be placed intermittently around the eyes for the initial 24 hours after surgery. The head dressing is removed on postoperative day 1, at which time showering may resume. Sleeping with the head elevated for one week, avoiding vigorous activity for two weeks after surgery, and a low-dose corticosteroid taper may help lessen bruising and swelling. Patients are asked to return at one week for wound assessment and staple/suture removal. Hair coloring is safe to perform at one month. It is not uncommon that the tine-fixation devices remain palpable out to 5 months or longer. Photographic documentation should occur at the 3-month and 12-month visits.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
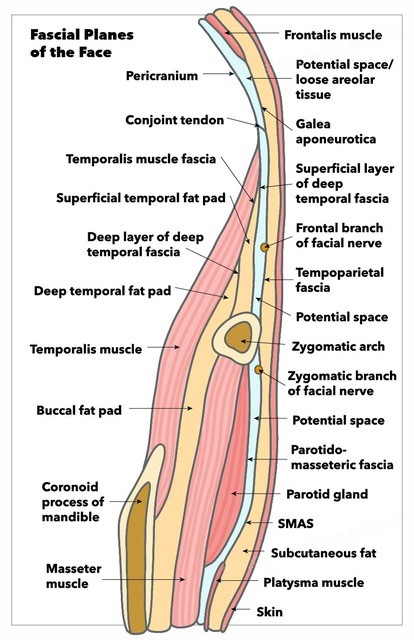
Fascial Planes of the Face and Musculature. This illustration depicts the fascial planes of the face, highlighting the continuity of the frontalis muscle, galea aponeurotica, temporoparietal fascia, superficial musculoaponeurotic system, platysma, and the location of the facial nerve.
Contributed by K Humphreys and MH Hohman, MD, FACS
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Terella AM, Wang TD. Technical considerations in endoscopic brow lift. Clinics in plastic surgery. 2013 Jan:40(1):105-15. doi: 10.1016/j.cps.2012.06.004. Epub 2012 Aug 27 [PubMed PMID: 23186760]
Graham DW, Heller J, Kirkjian TJ, Schaub TS, Rohrich RJ. Brow lift in facial rejuvenation: a systematic literature review of open versus endoscopic techniques. Plastic and reconstructive surgery. 2011 Oct:128(4):335e-341e. doi: 10.1097/PRS.0b013e3182268d41. Epub [PubMed PMID: 21921747]
Level 1 (high-level) evidenceIsse NG. Endoscopic facial rejuvenation: endoforehead, the functional lift. Case reports. Aesthetic plastic surgery. 1994 Winter:18(1):21-9 [PubMed PMID: 8122572]
Level 3 (low-level) evidenceElkwood A, Matarasso A, Rankin M, Elkowitz M, Godek CP. National plastic surgery survey: brow lifting techniques and complications. Plastic and reconstructive surgery. 2001 Dec:108(7):2143-50; discussion 2151-2 [PubMed PMID: 11743421]
Level 3 (low-level) evidencePerez PB, Gunter AE, Moody MP, Vincent AG, Perez CR, Serra RM, Hohman MH. Investigating Long-Term Brow Stabilization by Endotine-Assisted Endoscopic Brow Lift with Concomitant Upper Lid Blepharoplasty. The Annals of otology, rhinology, and laryngology. 2021 Oct:130(10):1139-1147. doi: 10.1177/0003489421997653. Epub 2021 Feb 25 [PubMed PMID: 33631951]
Knize DM. Anatomic concepts for brow lift procedures. Plastic and reconstructive surgery. 2009 Dec:124(6):2118-2126. doi: 10.1097/PRS.0b013e3181bd0726. Epub [PubMed PMID: 19952669]
Pitanguy I, Ramos AS. The frontal branch of the facial nerve: the importance of its variations in face lifting. Plastic and reconstructive surgery. 1966 Oct:38(4):352-6 [PubMed PMID: 5926990]
Sabini P, Wayne I, Quatela VC. Anatomical guides to precisely localize the frontal branch of the facial nerve. Archives of facial plastic surgery. 2003 Mar-Apr:5(2):150-2 [PubMed PMID: 12633201]
Park J, Yun S, Son D. Changes in Eyebrow Position and Movement with Aging. Archives of plastic surgery. 2017 Jan:44(1):65-71. doi: 10.5999/aps.2017.44.1.65. Epub 2017 Jan 20 [PubMed PMID: 28194350]
Core GB, Vasconez LO, Graham HD 3rd. Endoscopic browlift. Clinics in plastic surgery. 1995 Oct:22(4):619-31 [PubMed PMID: 8846631]
Level 3 (low-level) evidencePunthakee X, Mashkevich G, Keller GS. Endoscopic forehead and brow-lift. Facial plastic surgery : FPS. 2010 Aug:26(3):239-51. doi: 10.1055/s-0030-1254335. Epub 2010 Jun 3 [PubMed PMID: 20524172]
Starkman SJ, Sherris DA. Association of Corrugator Supercilii and Procerus Myectomy With Endoscopic Browlift Outcomes. JAMA facial plastic surgery. 2019 Sep 1:21(5):375-380. doi: 10.1001/jamafacial.2018.2084. Epub [PubMed PMID: 31046060]
Byun S, Mukovozov I, Farrokhyar F, Thoma A. Complications of browlift techniques: a systematic review. Aesthetic surgery journal. 2013 Feb:33(2):189-200. doi: 10.1177/1090820X12471829. Epub [PubMed PMID: 23388642]
Level 1 (high-level) evidenceCho MJ, Carboy JA, Rohrich RJ. Complications in Brow Lifts: A Systemic Review of Surgical and Nonsurgical Brow Rejuvenations. Plastic and reconstructive surgery. Global open. 2018 Oct:6(10):e1943. doi: 10.1097/GOX.0000000000001943. Epub 2018 Oct 15 [PubMed PMID: 30534495]