Introduction
The urinary bladder is a sac that serves as a reservoir for urine. The urine formed by the kidneys' nephrons is transported to the urinary bladder for storage before it gets expelled through the urethra. The urinary bladder is located in the extraperitoneal space of the pelvis behind the pubic bones and extends into the abdomen when filled with urine. The bladder is divided into two main parts, each with its anatomical, histological, and functional features. Above the ureteric orifices, the upper part is composed of the apex and body, while the lower part consists of the fundus, trigone, and neck. The capacity of the bladder is about 500 mL in healthy individuals.[1] See Image. Urinary Bladder, Vertical Section of Bladder Wall.
As the bladder fills, it stretches, simulating afferent signals. Efferent signals result in the bladder musculature's contraction and the subsequent urethral sphincter's relaxation. In addition to mechanoreceptors, various psychological factors like stress, sense of physical surroundings, and emotional status play a crucial role in the timing and setting of micturition.[2] This section describes the detailed microscopic structure of the urinary bladder wall.
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
Two main functions of the urinary bladder are urine storage and emptying. The specialized histology of the urinary bladder allows coordinated contraction and relaxation to facilitate its physiological function. The highly specific tissue architecture, particularly the lining of the urothelium, is closely linked to pathological conditions in the urinary bladder. Benign and malignant neoplasms of the urinary bladder, including von Brunn’s nests and urothelial carcinoma, are among the frequently diagnosed histological pathologies of the genitourinary tract, imposing a significant diagnostic challenge to clinicians.[3]
Structure
The microscopic structure of the urinary bladder wall organizes into the following layers from the inside out.[4]
- Lining epithelium
- Lamina propria
- Muscularis propria
- Serosa/Adventitia
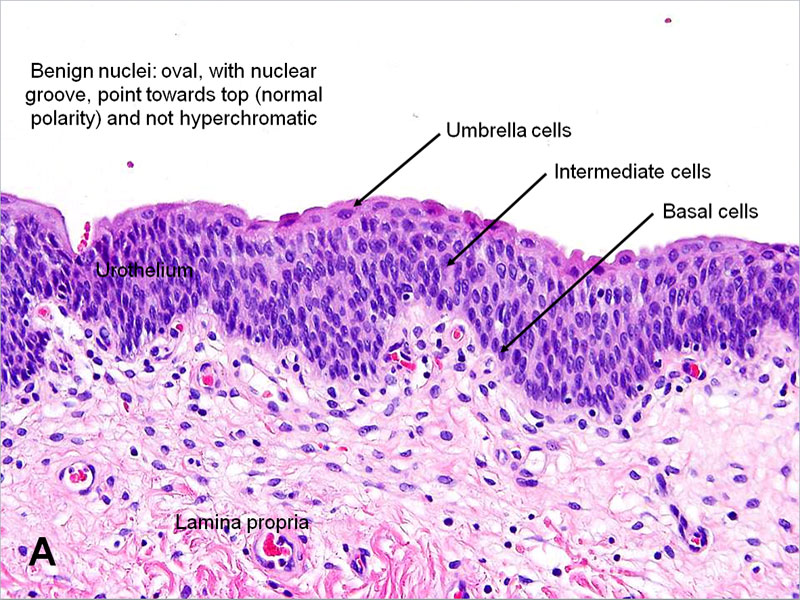
Lining epithelium: The urinary bladder lining is a specialized stratified epithelium, the urothelium. The urothelium is exclusively in urinary structures such as the ureter, urinary bladder, and proximal urethra.[5][6] The urothelium is composed of three different histological layers:
- Apical layer - The innermost layer is a barrier between the bladder lumen and the underlying tissue. It is a single layer of umbrella-shaped cells (i.e., umbrella cells) that are frequently binucleated. These apical umbrella cells of the urothelium form an impermeable barrier. Tight junctions between the cells decrease paracellular flux, while a glycoprotein layer of uroplakin on the surface of umbrella cells forms a superficial plaque that covers the superficial area.
- Intermediate layer - The middle layer is formed from two to three layers of polygonal cells.
- Basal layer - The basal layer is formed from two to three layers of small cuboidal cells.
The urothelium is thick with five to seven structural layers when the urinary bladder is relaxed. However, the bladder wall stretches to accommodate the increased volume when the urinary bladder fills with urine. The urothelium reorganizes into two or three layers in the distended bladder without structural damage. Due to this transitional ability of the urothelium, it is also known as the transitional epithelium.
Lamina Propria is the suburothelial layer separating the urothelium and underlying muscularis propria (detrusor muscle). A layer of basement membrane separates the overlying urothelium from the lamina propria. This layer is a heterogenous network of structural proteins and cells, composed of an extracellular matrix with elastic fibers, capillaries, lymphatics, immune cells, afferent and efferent nerve endings, fibroblasts, myofibroblasts, adipocytes, interstitial cells of Cajal or telocytes, an indistinct smooth muscle cells, and the muscularis mucosae. [7]
The interstitial cells of Cajal are within the lamina propria; they form a syncytium with smooth muscle cells and nerve endings. The interstitial cells of Cajal are multifunctional in different tissues. They are known to function as pacemaker cells in the gut, urethra, and prostate. However, in the bladder, they appear to act as nerve signal transducers to the bladder's smooth muscle cells.[8]
Muscularis propria, also known as the detrusor muscle, consists of three sublayers: inner longitudinal, middle circular, and outer longitudinal. These sublayers are well-defined around the neck of the urinary bladder but are randomly aligned with the rest of the bladder wall. The bladder's body has a higher smooth muscle content than the trigone, reflecting a well-developed network of myofibroblasts of lamina propria and muscularis mucosae in the body.
Serosa is a thin connective tissue layer that covers the bladder dome and is continuous with the peritoneal layer of the abdominal wall. It also contains blood vessels of various sizes.
Adventitia is a loose connective tissue layer that serves as the bladder's outer layer in areas of the bladder where there is no serosa.[9]
Function
The urothelium transforms from five to seven layers thick in a relaxed state to two or three layers thick in a distended bladder. This functional modification of the epithelium does not cause any damage - resulting in the name "transitional epithelium" – and allows for urine storage. In its superficial layer, umbrella-shaped cells are connected by tight junctions and covered by uroplakin, thus making it a barrier preventing injury to the tissue below.[10] The lamina propria and the urothelium are sensory regions regulating the afferent limb of the micturition reflex.[11] See Image. Benign Urothelial Cells, Histology.
The lamina propria acts as the bladder's "functional center" because of the presence of many specialized cells. It serves as a capacitance layer of the bladder that determines its compliance. The detrusor muscle of the muscularis propria is under autonomic nervous control. Sympathetic stimulation relaxes the detrusor muscle and contracts the urethral sphincter to allow urine filling, while parasympathetic stimulation contracts the detrusor and relaxes the urethral sphincter to allow micturition.[7]
Tissue Preparation
Tissue samples for histopathological examination of the bladder are collected via cystoscopy biopsy or radical cystectomy resections. Diagnosticians can use image-guided percutaneous bladder biopsy if there are contraindications to cystoscopy or surgery. Formalin-fixed tissue embedded in paraffin wax or frozen sections is helpful for routine hematoxylin and eosin histopathology examination of the urinary bladder.[12]
Histochemistry and Cytochemistry
Immunohistochemical staining of the urinary bladder is used to identify different cell types and malignant lesions. For instance, the umbrella-shaped cells in the apical layer of urothelium express CK20, and the cuboidal cells of basal cells are CD44+. However, in carcinoma in situ, all cell types express CK20 and p53 and show a greater Ki-67 proliferation index.[13]
Microscopy, Light
The urothelium, lamina propria, muscularis propria, and serosa may be seen under the light microscope in a histological section of the bladder wall. The urothelium's most superficial layer comprises dome-shaped umbrella cells whose shape becomes flat in a distended bladder. The cells of this layer are often multinucleated. Below the umbrella cells, the urothelium contains the multi-cell-layered intermediate and a single-cell layer of basal cells contacting its basement membrane. The cells of the intermediate layer are uninucleated; the number of layers in the intermediate layer depends on the stage of distension of the urinary bladder. The basal layer contains mononucleated, cuboidal cells with mitotic capability. Even though the turnover rate is gradual, this layer demonstrates a great regenerative capacity.[10] The lamina propria is a suburothelial layer, the contents of which are described in the "Structure" section above.
Microscopy, Electron
Umbrella cells demonstrate a characteristic ultrastructural feature; plaques or asymmetrical unit membranes. These are thick, focal areas of the cell membrane associated with actin filaments. Actin filaments extend from the plaques' inner surface to the umbrella cells' cytoplasm. In the non-distended bladder, the superficial cells appear to fold inwards; these folded plaques seemingly form membrane-bound, cytoplasmic fusiform vesicles. When the bladder distends during filling, these vesicles become part of a smooth surface as the cells flatten out.[14]
Pathophysiology
Urge incontinence, a form of urinary incontinence, is characterized by urinary urgency. Etiologies for urge incontinence include neurogenic, myogenic, or idiopathic causes. Disruption or damage of autonomic nerves or nerve signaling to the bladder cells may result in conditions including overactive bladder or bladder pain syndrome.[2]
Clinical Significance
Clinicians use cystoscopy to examine the urinary bladder mucosa for pathologic lesions, which may be diagnosed via biopsy sampling. Benign lesions include von Brunn’s nests. These islands or nests of the urothelium are separated from the luminal surface and consequently found within the lamina propria. Von Brunn’s nests of benign urothelium may undergo degeneration to form cysts (cystitis cystica).[15]
After prostate cancer, the second most common type of malignancy in the genitourinary tract is bladder cancer. Urothelial carcinomas are the most frequently diagnosed type of bladder cancer and are graded based on their depth of invasion into the bladder wall. Clinically 75%-85% of urothelial carcinomas are superficial, and 15%-25% of the cases are invasive and metastatic at the time of initial diagnosis.[16] Depending on the risk classification, non-muscle invasive neoplasms are treated with endoscopic reactions. However, more aggressive treatment options, including radical cystectomy, are preferred for patients with muscle-invasive histology.[17]
Media
(Click Image to Enlarge)
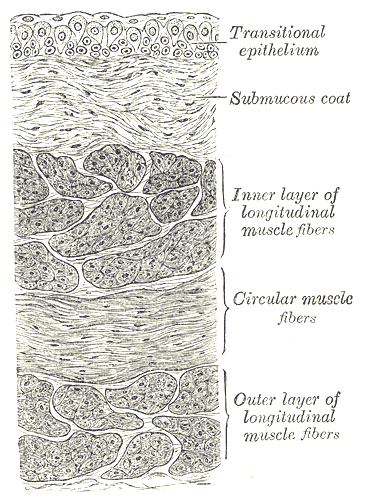
Vertical Section of the Urinary Bladder Wall. Anatomical features of the urinary bladder wall, including the transitional epithelium, submucous coat, inner layer of longitudinal muscle fibers, circular muscle fibers, and outer layer of longitudinal muscle fibers.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Sellers D, Chess-Williams R, Michel MC. Modulation of lower urinary tract smooth muscle contraction and relaxation by the urothelium. Naunyn-Schmiedeberg's archives of pharmacology. 2018 Jul:391(7):675-694. doi: 10.1007/s00210-018-1510-8. Epub 2018 May 28 [PubMed PMID: 29808232]
Chai TC, Russo A, Yu S, Lu M. Mucosal signaling in the bladder. Autonomic neuroscience : basic & clinical. 2016 Oct:200():49-56. doi: 10.1016/j.autneu.2015.08.009. Epub 2015 Sep 24 [PubMed PMID: 26422993]
Andersson KE, Arner A. Urinary bladder contraction and relaxation: physiology and pathophysiology. Physiological reviews. 2004 Jul:84(3):935-86 [PubMed PMID: 15269341]
Level 3 (low-level) evidenceCaione P, Capozza N, Zavaglia D, Palombaro G, Boldrini R. In vivo bladder regeneration using small intestinal submucosa: experimental study. Pediatric surgery international. 2006 Jul:22(7):593-9 [PubMed PMID: 16773371]
Level 3 (low-level) evidenceAbelson B, Sun D, Que L, Nebel RA, Baker D, Popiel P, Amundsen CL, Chai T, Close C, DiSanto M, Fraser MO, Kielb SJ, Kuchel G, Mueller ER, Palmer MH, Parker-Autry C, Wolfe AJ, Damaser MS. Sex differences in lower urinary tract biology and physiology. Biology of sex differences. 2018 Oct 22:9(1):45. doi: 10.1186/s13293-018-0204-8. Epub 2018 Oct 22 [PubMed PMID: 30343668]
Walz T, Häner M, Wu XR, Henn C, Engel A, Sun TT, Aebi U. Towards the molecular architecture of the asymmetric unit membrane of the mammalian urinary bladder epithelium: a closed "twisted ribbon" structure. Journal of molecular biology. 1995 May 19:248(5):887-900 [PubMed PMID: 7760330]
Level 3 (low-level) evidenceAndersson KE, McCloskey KD. Lamina propria: the functional center of the bladder? Neurourology and urodynamics. 2014 Jan:33(1):9-16. doi: 10.1002/nau.22465. Epub 2013 Jul 11 [PubMed PMID: 23847015]
Level 3 (low-level) evidenceDrumm BT, Koh SD, Andersson KE, Ward SM. Calcium signalling in Cajal-like interstitial cells of the lower urinary tract. Nature reviews. Urology. 2014 Oct:11(10):555-64. doi: 10.1038/nrurol.2014.241. Epub 2014 Sep 16 [PubMed PMID: 25224445]
Sánchez Freire V, Burkhard FC, Schmitz A, Kessler TM, Monastyrskaya K. Structural differences between the bladder dome and trigone revealed by mRNA expression analysis of cold-cut biopsies. BJU international. 2011 Jul:108(2 Pt 2):E126-35. doi: 10.1111/j.1464-410X.2010.09934.x. Epub 2011 Jan 18 [PubMed PMID: 21244608]
Khandelwal P, Abraham SN, Apodaca G. Cell biology and physiology of the uroepithelium. American journal of physiology. Renal physiology. 2009 Dec:297(6):F1477-501. doi: 10.1152/ajprenal.00327.2009. Epub 2009 Jul 8 [PubMed PMID: 19587142]
Level 3 (low-level) evidenceVannucchi MG, Traini C, Guasti D, Del Popolo G, Faussone-Pellegrini MS. Telocytes subtypes in human urinary bladder. Journal of cellular and molecular medicine. 2014 Oct:18(10):2000-8. doi: 10.1111/jcmm.12375. Epub 2014 Aug 19 [PubMed PMID: 25139461]
Butros SR, McCarthy CJ, Karaosmanoğlu AD, Shenoy-Bhangle AS, Arellano RS. Feasibility and effectiveness of image-guided percutaneous biopsy of the urinary bladder. Abdominal imaging. 2015 Aug:40(6):1838-42. doi: 10.1007/s00261-015-0356-5. Epub [PubMed PMID: 25875861]
Level 2 (mid-level) evidenceWang G, McKenney JK. Urinary Bladder Pathology: World Health Organization Classification and American Joint Committee on Cancer Staging Update. Archives of pathology & laboratory medicine. 2019 May:143(5):571-577. doi: 10.5858/arpa.2017-0539-RA. Epub 2018 Jul 25 [PubMed PMID: 30044124]
Jhang JF, Ho HC, Jiang YH, Lee CL, Hsu YH, Kuo HC. Electron microscopic characteristics of interstitial cystitis/bladder pain syndrome and their association with clinical condition. PloS one. 2018:13(6):e0198816. doi: 10.1371/journal.pone.0198816. Epub 2018 Jun 7 [PubMed PMID: 29879217]
Hodges KB, Lopez-Beltran A, Maclennan GT, Montironi R, Cheng L. Urothelial lesions with inverted growth patterns: histogenesis, molecular genetic findings, differential diagnosis and clinical management. BJU international. 2011 Feb:107(4):532-7. doi: 10.1111/j.1464-410X.2010.09853.x. Epub 2010 Nov 23 [PubMed PMID: 21091975]
Castillo-Martin M, Domingo-Domenech J, Karni-Schmidt O, Matos T, Cordon-Cardo C. Molecular pathways of urothelial development and bladder tumorigenesis. Urologic oncology. 2010 Jul-Aug:28(4):401-8. doi: 10.1016/j.urolonc.2009.04.019. Epub [PubMed PMID: 20610278]
Level 3 (low-level) evidenceLenis AT, Lec PM, Chamie K, Mshs MD. Bladder Cancer: A Review. JAMA. 2020 Nov 17:324(19):1980-1991. doi: 10.1001/jama.2020.17598. Epub [PubMed PMID: 33201207]