Introduction
The azygos vein forms from the junction of the right subcostal veins and the ascending lumbar veins. The azygos vein is a unilateral vessel that ascends in the right posterior mediastinum along the right border of the inferior eight thoracic vertebrae. In some instances, the azygos vein can travel in the midline along the top of the thoracic vertebrae. This vein carries deoxygenated blood forming a collateral pathway between the superior vena cava (SVC) and the inferior vena cava (IVC).
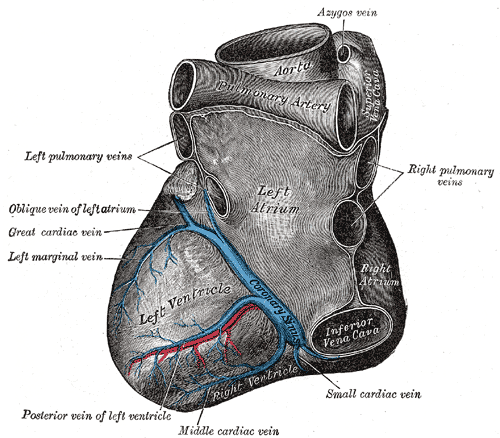
Starting at vertebral levels T12-L2, the azygos vein travels posterior to the right root of the lung (T5-T6) and arches superiorly over the root of the lung, emptying into the SVC. Sometimes, the azygos vein may travel higher to drain into the brachiocephalic or right subclavian vein. There are also instances where the azygos vein can end by draining into the intra-pericardial SVC or even the right atrium.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
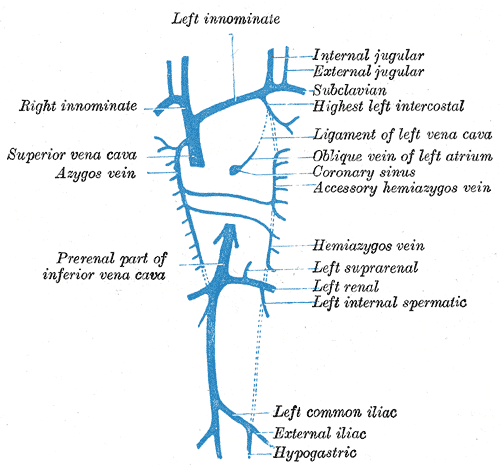
In addition to receiving the right posterior intercostal veins, the azygos vein communicates with the vertebral venous plexus that drains the back, vertebrae, and structures in the vertebral canal. The azygos vein also receives the mediastinal, esophageal, and bronchial veins, the hemi-azygos vein, and the accessory hemi-azygos vein.
The hemi-azygos and accessory hemi-azygos veins cross the midline at T9 and T8, respectively, posterior to the aorta, thoracic duct, and esophagus. In some instances, the hemi-azygos and the accessory hemi-azygos veins combine to form a shared vein crossing the midline at T9 to empty into the azygos vein. The azygos vein enters the thorax through the aortic hiatus in the diaphragm just to the right of the cisterna chyli.
Embryology
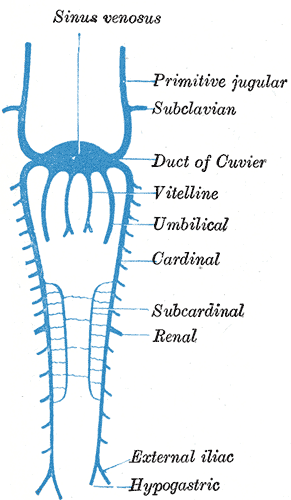
The azygos vein originates from the last portion of the posterior cardinal veins.
The subcardinal, sacrocardinal, and supracardinal veins form between the fifth and seventh weeks of gestation. The supracardinal veins function to drain the body wall through intercostal veins formed from posterior cardinal veins. The anterior cardinal veins, common cardinal veins, and proximal right posterior cardinal veins go through a significant developmental process to become the veins of the heart, the SVC, and its tributaries.
Since the proximal portion of the azygos vein is a tributary to the SVC, it shares a common lineage with the SVC. The proximal portion of the azygos vein also derives from the anterior, common cardinal vein, and the sinus venosus. With the proximal segment of the right posterior cardinal vein, the posterior cardinal derived veins, supracardinal, are further involved in forming the arch of the azygos system. The azygos venous system appears in the image below.[2]
Blood Supply and Lymphatics
The azygos vein is considered a large vein and thus receives vascular supply for its tissues by the vasa vasorum network.
Physiologic Variants
Developmental variations in the azygos system are usually asymptomatic and typically detected during routine examinations. The most documented congenital abnormalities include an azygos lobe of the right lung, agenesis of the azygos vein, azygos continuation of the IVC, and partial venous return.
Azygos Lobe of the Right Lung
Incomplete medial migration of the right posterior cardinal vein gives rise to an azygos lobe of the right lung. This anomaly is easily identifiable on CT scans. Such scans would show the azygos vein more lateral than the usual anterior arching before entering the SVC or right brachiocephalic vein. This lateral positioning of the azygos arch leads to the intrusion of the lung farther into the pretracheal and retro-tracheal mediastinum.[3]
Agenesis of the Azygos Vein
Agenesis of the azygos vein results from the failed development of the superior segment of the right supracardinal vein. This variant is typically asymptomatic because the hemiazygos and accessory hemiazygos veins ensure the draining of the right and left posterior intercostal veins.[1]
Azygos Vein Continuation With the IVC
The azygos vein's continuation with the IVC results from the congenital interruption of the IVC. This occurs due to the failure of the union between the right subcardinal veins and the hepatic veins. The failure of the development of the right subcardinal vein, which is the precursor of the prerenal segment of the IVC, prevents the IVC from developing. Identification of this vascular anomaly is necessary before undertaking surgical procedures involving the azygos vein.
Azygos continuation can be suspected on a chest x-ray if the radiograph shows a focal enlargement of the right paratracheal stripe above the right mainstem bronchus. A CT scan can be useful to confirm the enlargement of the azygos vein and the azygos arch. A CT scan would discover an absence of the intrahepatic portion of the IVC. Azygos continuation is typically identified in otherwise asymptomatic patients but can also be associated with severe congenital heart disease, asplenia, or polysplenia syndromes.[3]
Clinical Significance
Acquired anomalies affecting the azygos vein include enlargement due to hemodynamic changes or the presence of lesions. These anomalies may induce pulmonary edema due to the physiological imbalance of fluid. On chest X-ray, the size and contour of the azygos vein can provide useful insight into any hemodynamic changes. Studies have shown that the main reason for enlargement of the azygos vein is the increased mean right atrial pressure, which is usually a result of constrictive pericarditis, cardiac tamponade, pulmonary hypertension, and portal hypertension.[1]
Fibrosing Mediastinitis
A rare, typically benign condition, fibrosing mediastinitis, results from the proliferation of acellular collagen and fibrous tissue inside the mediastinum. There are instances where tissue proliferation can extend to the soft tissues of the posterior mediastinum and pleural space. Evidence for this would be demonstrated by chest x-rays, which may show signs of pulmonary venous obstruction manifesting as localized pulmonary venous hypertension. A CT scans with contrast can demonstrate the involvement of the azygos vein with fibrosing mediastinitis. The scan would depict the level and extent of the stenosis. This condition would result in the engorgement of the azygos pathway.[1]
Superior Vena Cava Syndrome
Superior vena cava syndrome results from the absence of blood flow through the SVC. An intraluminal blockage or external compression can cause the obstruction. The azygos venous system is the most important pathway for the decompression of SVC obstruction. SVC syndrome develops as a result of collateral blood vessels being unable to compensate for the obstructed SVC. If the obstruction of the SVC is above the azygos vein, the venous flow of the azygos vein is retrograde. If the lesion of the SVC is below the azygos vein, the venous flow direction will be anterograde.[1]
Inferior Vena Cava Obstruction
Several factors can cause IVC obstruction, but the most important are membranous obstruction, Budd-Chiari syndrome (BCS), and neoplastic lesions. The presence of an IVC obstruction requires decompression of the liver. Intrahepatic venous, portocaval, and spider web vessels (forming the caput medusae) develop as a result of the obstruction to decompress the liver parenchyma. Ascending lumbar veins and extrahepatic collateral vessels are also influential in the decompression of the liver in IVC obstruction and will drain into the azygos system. Lung cancer adenopathy, sarcoidosis, and lymphoma are typical examples of nonvascular lesions found in the right inferior paratracheal region, often mimicking azygos vein enlargement.[1]
Insertion of Devices Into the Azygos Vein
Central devices may be placed in the SVC between the azygos vein arch and the atriocaval junction. Examples of central devices include central venous catheters and peripherally inserted central catheters (PICCs). Misplacement of the catheter tip can occur with it being placed in the azygos vein. This result can be confirmed using chest X-rays. The film would show the catheter loop in the right superior mediastinum. Fistulas and thrombosis are typical complications of implantable devices. Fistulas between the azygos vein and airways may occur. Pacemaker implantation in the azygos vein can also induce SVC syndrome because of thrombosis of the tip.[1]
Demonstration of the Enlargement of Azygos Vein With Specific Etiologies: Congenital Azygos Continuation and Absence of IVC
A marked enlarged IVC on the CT is diagnostic for this entity, as demonstrated in two patients. About 50% of such cases may be associated with polysplenia syndrome and congenital heart anomalies such as dextrocardia, cor biloculare, and pulmonary atresia.[4]
Inferior Vena Cava Thrombosis
During obstruction of the IVC by thrombosis, the azygos and hemizygous veins, as well as the vertebral veins, form important collateral circulation by which venous blood can return to the heart. Enlargement of the azygos vein can occur under such a condition.[4]
Right Atrial Mural Thrombosis and Pulmonary Embolism
These two conditions can lead to elevation of the right atrial pressure that, in turn, impedes the venous return from both the SVC and IVC, leading to enlargement of the azygos vein. A combination of IVC thrombosis, right atrial mural thrombosis, and pulmonary embolism is not uncommon.[4]
Congestive Heart Failure
Congestive heart failure, particularly right-side heart failure, impedes the venous return to the right atrium. This condition is the most common cause of azygos vein enlargement.[4]
Portal Vein Thrombosis
Anastomosis between the portal and systemic circulations in portal vein obstruction offers effective collateral circulation. The portal blood can empty into the left gastric vein that connects with the esophageal tributaries of the azygos and accessory hemizygous veins. Azygos vein enlargement in cirrhotic patients with portal hypertension is also quite common.[4]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
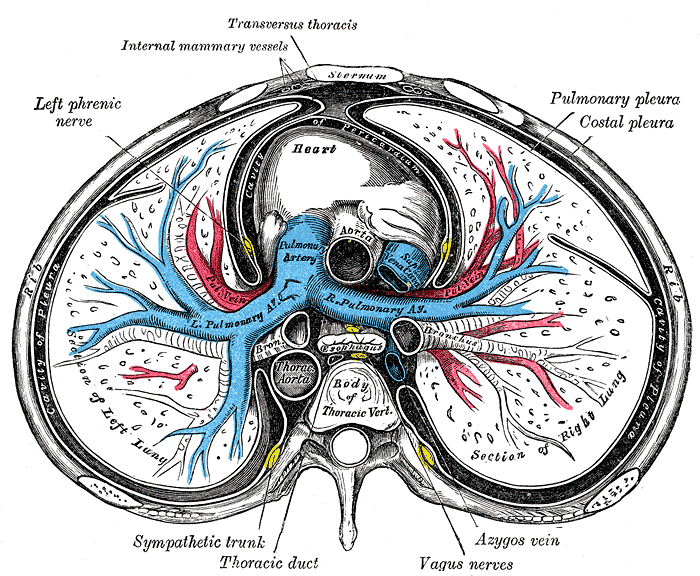
Sternum Transverse Section. This illustration shows the anatomic relationships between the right and left lungs, heart, pulmonary pleura, costal pleura, pleural cavity, ascending and thoracic aorta, pulmonary artery and its right and left branches, superior vena cava, esophagus, main bronchi, azygos vein, vagus nerves, thoracic duct, sympathetic trunk, left phrenic nerve, internal mammary vessel, transversus thoracis muscle, rib, sternum, and thoracic vertebral body.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
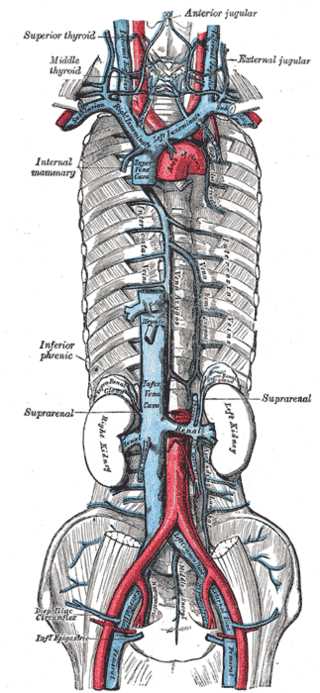
Azygos Venous System. The azygos venous system includes the internal mammary vein, inferior phrenic vein, suprarenal vein, and the left and right kidneys.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Piciucchi S, Barone D, Sanna S, Dubini A, Goodman LR, Oboldi D, Bertocco M, Ciccotosto C, Gavelli G, Carloni A, Poletti V. The azygos vein pathway: an overview from anatomical variations to pathological changes. Insights into imaging. 2014 Oct:5(5):619-28. doi: 10.1007/s13244-014-0351-3. Epub 2014 Aug 30 [PubMed PMID: 25171956]
Level 3 (low-level) evidencePetrenko VM. [Development of the ascending lumbar and azygos veins in human embryogenesis]. Arkhiv anatomii, gistologii i embriologii. 1990 Jun:98(6):65-70 [PubMed PMID: 2400331]
Dudiak CM, Olson MC, Posniak HV. CT evaluation of congenital and acquired abnormalities of the azygos system. Radiographics : a review publication of the Radiological Society of North America, Inc. 1991 Mar:11(2):233-46 [PubMed PMID: 2028062]
Shin MS, Ho KJ. Clinical significance of azygos vein enlargement: radiographic recognition and etiologic analysis. Clinical imaging. 1999 Jul-Aug:23(4):236-40 [PubMed PMID: 10631900]
Level 3 (low-level) evidence