Introduction
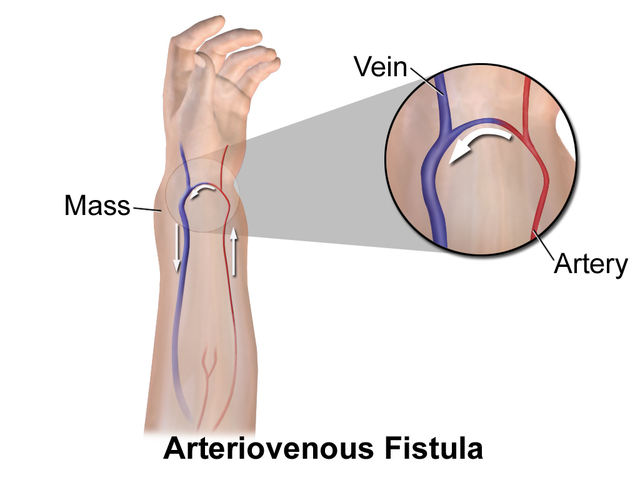
Arteriovenous fistulas (AVFs) are abnormal connections between an artery and a vein (see Image. Diagram of Arteriovenous Fistula).[1] In certain contexts, these may also be referred to as arteriovenous malformations.[2] AVFs can exist almost anywhere in the body, depending on the etiology. These can be divided into 2 groups: acquired or congenital. Acquired fistulas can be further subdivided into surgically created, as in for hemodialysis, or secondary to trauma, whether accidental or procedure-related.
The anatomy of the fistula depends on its location in the body. AVFs for hemodialysis are typically created in the extremities, and vascular surgeons generally prefer the upper extremities over the lower extremities. The cephalic and basilic veins are often used for the surgical creation of an AVF. The radial artery at the volar wrist and the brachial artery at the antecubital fossa and medial upper arm are typical anatomical locations for fistula creation. However, the radio-cephalic AVF is the preferred initial access for hemodialysis.[3]
The literature has described 2 types of lower extremity surgical AVFs for hemodialysis. The superficial femoral or popliteal vein can be mobilized from the knee to anastomose with the superficial femoral artery, called an SFV transposition. The saphenous vein can create a loop AVF on the anterior thigh, anastomosed with the common femoral artery.[4][5]
Although no type of congenital AV fistula is common, reported locations for congenital AVFs include pulmonary, aortocaval, dural, carotid-cavernous, coronary, and hepatic.[6][7][8][9] While the majority of neck fistulas do occur secondary to trauma, congenital vertebrovertebral fistulas and carotid-jugular fistulas have been described in children.[10]
AVFs as a result of iatrogenic injury are typically a result of surgical procedures, invasive line placement, or needle biopsy. The literature demonstrates multiple reports of iatrogenic injury resulting years after surgical procedures.[11][12] Traumatic AVF can essentially occur wherever there is trauma, and these can also have a late presentation.[13] Greater than 50% of traumatic AVFs happen in the lower extremities, and about one-third occur in the femoral vessels, while 15% take place in the popliteal vessels.[14]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Arteriovenous fistulas can be surgically created for hemodialysis access, can occur as a result of a congenital anomaly, or be secondary to iatrogenic injury or trauma. Penetration of any mixed-type vasculature can ultimately heal arteries and veins together, bypassing downstream arteriole and capillary systems.
Iatrogenic Fistulas
These are most commonly reported due to percutaneous access of the femoral vein and femoral artery during cardiac catheterization. However, subclavian and carotid fistulas have been reported to be associated with the placement of central lines.[15] The most common AVFs described as a result of percutaneous biopsy are renal; however, these are typically self-limited, and very few require intervention.[16]
Traumatic Fistulas
These are often associated with direct arterial trauma and long bone fractures, especially where an artery and vein are in close communication. Ninety percent of traumatic AVFs are due to penetrating trauma, the majority of which are gunshot wounds.[17] A small portion of neck AVFs can occur in association with a hyperextension injury or spine surgery. Carotid-cavernous fistulas, typically due to trauma, can be fatal and are most often associated with a basilar skull fracture, penetrating trauma to the area, and ruptured aneurysms.[18] Two-thirds of traumatic AVFs are diagnosed within 1 week of the injury; however, some may present weeks to years after the event.[19][20]
Congenital Fistulas
These are not well-understood. Congenital AVFs of the central nervous system can be dural or carotid cavernous. AVFs of the neck are mostly due to trauma; however, fibromuscular dysplasia, neurofibromatosis, and other types of collagen disorders have been associated. Pulmonary vascular malformations are typically simple and more similar to AVFs than true malformations.[21] Other types of AVFs are very rare.
Epidemiology
Arteriovenous fistulas were originally described by William Hunter as early as 1757.[14] Much of the experience in managing AVFs originated out of traumatic injuries resulting in AVFs from the Second World War, the Korean War, and the Vietnam War. 215 AVFs and aneurysms were reported as a result of the Korean War.[22] In the civilian population, traumatic AVFs of the abdomen and extremities are equally distributed, unlike in the military, where the majority of traumatic AVFs occur in the extremities.[23][17] This difference is likely due to the body armor worn by the military. Demonstrably, traumatic fistulas are much more common than congenital fistulas and are more frequently discussed. Congenital fistulas are generally rare and found in case reports and small studies.[24]
The National Institute of Diabetes and Digestive and Kidney Diseases reported that, as of 2013, over 468,000 patients were on hemodialysis. Twenty percent of those patients receive dialysis via a surgically created AVF. In the HEMO Study published in 2000, AVF prevalence varied between dialysis centers from 4-77%. The authors discovered a decreased prevalence of AVF compared to other means of hemodialysis in females, blacks, obese, elderly, and patients with peripheral arterial disease. Geographically, the rate of AVF creation varies greatly, with the highest rates being in the Northeast and the lowest in the Southwest of the United States.[25]
History and Physical
The presentation of arteriovenous fistulas can vary depending on the location and etiology. Patients with an AVF for hemodialysis present with evidence of a surgical incision on the lateral wrist, volar forearm, or upper arm. A working AVF has a palpable thrill and continuous bruit. A patient with an AVF with an outflow obstruction may present with a pulsatile fistula or prolonged bleeding from a puncture site from hemodialysis. Superficial fistulas have a palpable thrill, a bruit, or even a pulsatile mass. It may be possible to auscultate a machinery-like murmur over the fistula.[26]
Fistulas of the extremities, regardless of etiology, may present with signs of venous hypertension, including varicosities, pain, and swelling. If there has been a long-standing fistula, there may be a significant size discrepancy between the 2 limbs. Suppose the patient reports a history of trauma, anywhere from weeks to years after injury, in particular with long bone fractures or ongoing neurologic deficits. In that case, the index of suspicion for AVF should be raised even in the event of a clinically normal exam.[17]
Patients with congenital AVF may not present until later in life, and a history of trauma should be ruled out. Depending upon location, these fistulas may be low-flow at birth and become high-flow lesions in adulthood. Patients with brain arteriovenous malformations can present with headaches, neurologic deficits, seizures, or a combination. These patients can also be at risk for hemorrhage or ischemia to the parenchyma surrounding the AVM/AVF due to steal syndrome.
In severe, chronic, or high-flow fistulas, patients can present in high output cardiac failure, which results in the shunting of oxygenated blood back to the right heart. Due to the shortcut that the arterial blood takes through the venous system, this results in decreased peripheral resistance. To maintain blood pressure, the total circulating blood volume is increased, leading to heart failure. The Nicoladoni-Israel-Branham sign is a finding of reflex bradycardia with fistula compression due to increased afterload.[10]
Cutaneous AVFs can present with a pink stain, a mass, dilated veins, unequal limb size, or skin ulceration. Patients may feel limb heaviness that aggravates with dependency and relieves with elevation. Almost half of patients experience pain.[27]The pain may be caused by ischemic tissues or by the compression effect on surrounding nerves. Some lesions can be tender, such as glomuvenous malformations.
On examination, there could be an increase in the size of the limb, swelling, discoloration, or prominent vessels with a murmur or palpable thrill. The lesions may also be pulsatile. Over the lesion, there could be hyperhidrosis, hyperthermia, hypertrichosis, or a bruit. Limbs and joints may be functionally impaired from mass effect or necrosis from prolonged tissue ischemia. Visceral AVFs can present with hematemesis, hematuria, hemoptysis, or melena. Occasionally, patients may have an initial presentation of heart failure,e particularly in cases where the fistula is between a very large artery and vein.[27]
Evaluation
Beyond the clinical evaluation from history and physical, a duplex ultrasound (US) is a non-invasive and inexpensive way to confirm the diagnosis of AVF, given that the AVF is superficial. The duplex US demonstrates low resistance flow in the feeding artery. At the anastomosis or fistula, turbulence and high-velocity flow are demonstrated. Thickened walls and high-velocity flow is seen in the dilated draining veins or venous plexus of the AVF. A pseudoaneurysm, venous aneurysm, or dilated feeding artery may also be demonstrated on the ultrasound exam.[15]
Computed tomography angiography (CTA) and magnetic resonance angiography (MRA) show early contrast filling the arterial phase in the involved vein. While MRA may not be an option in trauma or post-trauma patients due to residual metal, CTA is reliable, non-invasive, and accessible as an initial diagnostic test. Disadvantages of CTA include streak artifact from metallic objects (which can be an issue in penetrating trauma), motion artifact, and reliance on contrast timing in the fistula.[28] A retrospective study conducted by Biswas et al observed four-dimensional (4D) CTA to be precise in delineating AVMs and dural AVFs, providing findings relevant to the results of digital subtraction angiography.[29] A study by In 't veld et al compares the diagnostic precision of 4D-CTA and that of DSA. It was found that 4D CTA had much higher sensitivity and specificity and was less invasive than DSA.[30]
Selective angiography is the gold standard and has shown better accuracy than CTA. It is the most invasive evaluation of an AVF but provides the exact point of arteriovenous communication surrounding vascular anatomy, flow dynamics, and mechanism for treatment.[31] Cost, procedural delay, additional arterial or venous access, and the need for a specially trained team are disadvantages of angiography. See image. Arteriovenous Fistula.
Patients presenting in need of vascular access for ESRD need to be evaluated for optimal placement of an AVF. Given the preference of the upper extremity, non-dominant over-dominant, and forearm over the upper arm, all patients should be evaluated with a duplex ultrasound scan, including patients presenting for evaluation of an existing AVF. Criteria have been developed for optimal results and primary patency rates. Clinical exams and vein mapping have decreased primary failure rates and negative surgical exploration in the first attempts to create AVFs.[32]
Blood gas analysis in an AVF shows a higher oxygen content in the venous side of the blood distal to the fistula than in normal venous blood. A flow-directed balloon catheter (Swan-Ganz catheter) can assess hemodynamics and reveal increased cardiac output and decreased peripheral vascular resistance. Extremely large AVFs may present with thrombocytopenia due to constant turbulence and platelet trapping.
Treatment / Management
Most cases of arteriovenous fistulas in the past were treated conservatively in wartime and, later on, were surgically managed if needed.[22] Early intervention, however, may deter complications of AVFs that can be avoided, and post-traumatic fistulas should be closed as close to diagnosis as possible.[26] AVF treatment aims to isolate and close the fistula while attempting to maintain essential blood flow. Repair may be completed by direct primary repair, reconstruction (autogenous or prosthetic graft or bypass), or endovascular.[14] (B3)
Indications for Treatment
- Hemodynamic instability, availability of a surgical team, injury to adjacent tissue, and unsuccessful endovascular repair are all indications for open surgical intervention on a fistula.
- In traumatic fistulas, failure of spontaneous regression within 2 weeks indicates repair.
- Congenital fistulas are typically repaired when they present due to sequelae in later life, as many may remain asymptomatic until adulthood.
- Hemodialysis fistulas that are no longer functioning, no longer needed, have endured multiple attempts at salvage, or fail to mature should be considered for ligation.
- Other important indications of surgical repair of AVFs are hemorrhage, pain with ischemia, congestive cardiac failure, Limb-size inequality, nonhealing ulcers, and functional impairment.
Endovascular Management
- It is the preferred method of management for AVFs.
- The first endovascular repair was done in 1992 by Parodi of a traumatic subclavian AVF; a covered stent was used.[33]
- The advantages of endovascular repair include rapid recovery, less post-operative pain, and less disability compared with the open approach.
- Coils, stent-grafts, covered stents, and cyanoacrylate glue are among the options for closing the fistula.[34]
- Stent grafts are used to exclude the fistula while preserving the essential artery and vein; coils can be used when there is a low risk of complication from embolizing essential vessels. Endografts designed for larger vessels, such as the aorta or iliac vessels, can be used similarly. Stent graft patency rates at 1 year range between 88 and 100%.
- Complications associated with the placement of covered stents include arterial dissection or rupture, device migration, or embolization. In a review of patients with traumatic AVFs, the most common reason for the failure of the endovascular intervention was the inability to advance the guidewire.
- The patient may also develop intimal hyperplasia at the stent's placement site or subacute thrombosis, leading to occlusion and distal ischemia. If the patient does develop venous thrombosis, anticoagulation should be initiated and continued for 6 months.
- Embolization can be advantageous for complex AVFs with multiple feeding and draining vessels. Deep-seated or intra-organ and adjacent to critical anatomy, AVFs are more amenable to endovascular management than open surgery.[35][36]
- Contraindications to endovascular management include contrast allergy.
- In the treatment of AVFs, many sclerosing agents, including injectible absolute ethanol, can be administered. They may carry a risk of necrosis of the surrounding tissue. So, they should be used with caution.[37] (B3)
Open Surgery
- It is an option for repair when endovascular management fails.
- In addition to the need for surgical exposure of the fistula and increased risk of bleeding, high morbidity is associated with an open approach, including venous stasis, limb (or distal) ischemia, limb loss, venous thrombosis, and pulmonary embolism.
- Repairs can be made via autogenous (usually saphenous vein) grafts, synthetic grafts, venous ligation (diameter dependent), bypass, or complex reconstruction involving 1 or more of the above.
- Limitations for using the saphenous vein autologous graft include needing a 3-8 mm vein, no lower extremity venous insufficiency, and no thrombophlebitis of the vein.[14]
- Conservative management is an option if no symptoms or complications exist or the AVF is expected to be self-limited.
Differential Diagnosis
Differential diagnoses of AVF include other conditions that result in hyperdynamic circulation, such as tachycardia, increased cardiac output, and decreased peripheral resistance.
- Arteriovenous malformation: These are congenital lesions from the failure of fetal vascular differentiation. High flow or complex AVMs are more likely to have high resistance, similar to a capillary bed, and, therefore, are more likely to be asymptomatic.[38] AVMs can be differentiated from AVFs with high resonance imaging (CTA or MRA).
- Hemangioma: Hemangiomas, also known as vascular tumors, may have similar symptoms to AVFs. However, these tend to present with overt bleeding. Hemangiomas have been found to have mitotic activity and can rapidly involute.[38] Similar to AVMs, these can be ruled out with CTA or MRA.
- Pseudoaneurysm: These may present as a pulsatile mass associated with a vascular access procedure. Pseudoaneurysms and true aneurysms may have a thrill due to significant turbulence in the area. Doppler US can differentiate these from a fistula.
- Malignancy: Malignant masses can require significant blood flow and present as a previously unnoticed pulsatile mass if they are closer to a larger vessel. Doppler US and/or multiphasic imaging can help differentiate these.
- Cyst/Abscess/Hematoma: These are typically identified as simple hypodense lesions on the duplex US and do not demonstrate flow.
Prognosis
While some congenital arteriovenous fistulas can be fatal, leading to failure to survive, the overall prognosis is good. Peripheral arteriovenous fistula does not typically incur systemic hemodynamic effects, and around 15% of all AVFs do.[39]
The Schobinger Classification is a clinical staging system that serves to predict the success of treatment. Stage 1 is of quiescence and is described as a cutaneous blush and skin warmth at the site of the fistula. The second stage demonstrates darkened skin, a pulsatile lesion with a bruit on auscultation, or palpable thrill. This stage is called expansion. Stage 3, the destruction phase, is essentially steal syndrome and is characterized by skin changes, ulceration, and distal ischemia. Stage 4 is the decompensated phase, characterized by high-output heart failure. While it has been shown that decompensated heart failure can be completely reversed after a high-flow AVF is closed, the prognosis is much better in patients who present earlier.[38]
Prompt recognition is crucial for favorable outcomes. Brinjikji et al observed spinal dural AVFs, which are either easily missed on imaging or misdiagnosed. These cases were diagnosed at their institution. They stated that delays in establishing a diagnosis in these cases led to an increased incidence of additional irreversible disability that frequently could not be corrected surgically or otherwise.[40]
Complications
Chronic venous insufficiency/venous hypertension: Venous hypertension can present as swelling of the affected extremity, which can be progressive and limit mobility. Insufficiency is demonstrated in developing stasis pigmentation of the skin, varicosities, and ulcerations. This complication directly results from arterial pressure against the thinner venous walls and failure of 1-way valves in the veins.
High cardiac output failure: In a study of 120 patients who suffered from high-output heart failure, 23% were found to have an AV shunt, which includes congenital, traumatic, and HD fistulas. In all patients with high-output cardiac failure, their increased stroke volume was secondary to decreased vascular resistance, which is a mechanism found in patients with AVFs, particularly when these become high-flow.[41]
Arterial insufficiency: Steal syndrome can occur in up to 6% of patients with an AVF or arteriovenous graft for hemodialysis. It is a result of a high-flow fistula causing distal ischemia.[38] These patients can present with severe pain associated with the use or during hemodialysis. They may also have swelling or signs of ischemia distal to the fistula, such as cool skin, discolored fingers or toes, diminished distal pulses, hair loss, or atrophy. A normal compensatory mechanism to the fistula is to increase overall flow to the affected extremist, which provides adequate blood flow to the higher resistance distal capillary beds; when this mechanism fails, steal syndrome results, which blood through the lower resistance fistula, instead of supplying distal tissue. Inflow stenosis of the arterial supply can cause or worsen steal. In the evaluation for steal syndrome, fistula compression increases inflow to the symptomatic distal extremity.[42]
Hemorrhage: Hemorrhage is a much rarer complication than those above. Due to the high flow through the venous system, dilatations can occur throughout the venous drainage system. These can become thin-walled and be at risk for rupture. This can be especially problematic with hemodialysis fistulas, which are repetitively accessed through the venous side, causing ulcerations to the vein and overlying skin. High flow through the fistula and outflow stenosis can make obtaining hemostasis challenging after dialysis.[43]
Consultations
The consultation needed to manage the arteriovenous fistula depends on its location and nature. Specialties required to be involved can include:
- Vascular surgery
- Interventional radiology
- Interventional cardiology
- Neurosurgery
- Interventional neurology
Deterrence and Patient Education
While AVFs may be unavoidable for patients with end-stage renal disease, the best way to prevent the development of an AVF is to avoid unnecessary trauma or procedures that may lead to their development. Congenital AVF etiology is poorly understood; thus, there is little to do regarding prevention.
Patients who are diagnosed with an AVF or who think they may have an AVF should see their primary care provider first. After a thorough work-up, these patients may be referred to 1 of the specialists mentioned above for management and potential fistula repair. Important things to write down before any appointment include any symptoms experienced, changes in the extremity or area of concern, and any significant history, such as trauma or procedures in the same area. A fistula can arise from a prior injury at any point in your lifetime.
Expectations from your provider can include further labs and imaging, including an ultrasound, CT, or MRI. To start the evaluation, your provider looks at, listens to, and feels the area. In addition to your questions and the provision of symptoms, your provider will likely ask you further questions to help diagnose this problem.
Enhancing Healthcare Team Outcomes
Patients presenting with signs and symptoms of arteriovenous fistulas require an interprofessional approach to the workup. As with any condition, this starts with a thorough history and physical exam. Involving the appropriate surgical team early in the process can help direct the evaluation so that the imaging obtained can be used in surgical planning. Early warnings to trauma patients with injuries to the extremities, particularly involving an arterial or venous injury, should help to prevent late presentations of high-flow AVFs. Surgeons, interventionalists, and intensivists should be aware of arteriovenous fistulas as a potential complication of bedside procedures for venous access and biopsies.
Media
(Click Image to Enlarge)
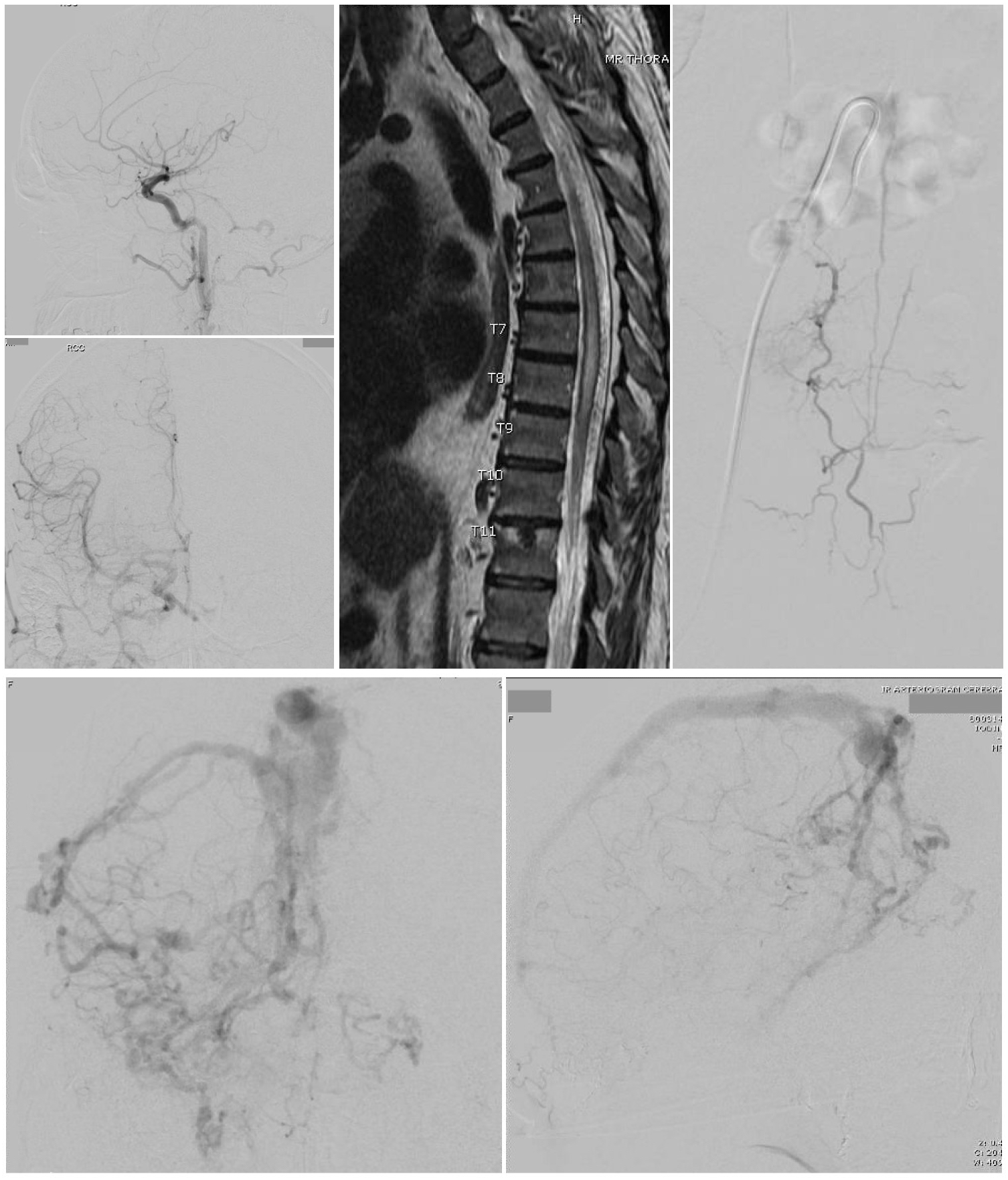
Arteriovenous Fistula. A Cognard type 3 dural arteriovenous fistula (top left 2 images) is seen on cerebral catheter angiography with arterial phase right common carotid injections, lateral view (top) and anteroposterior view (bottom). Bottom 2 Images - A cerebral catheter angiogram with anteroposterior (left) and lateral (right) views, late arterial phase, shows a Cognard type 4 dural arteriovenous fistula with multiple feeding arteries, cerebral and cerebellar draining veins, and venous ectasia of the superior sagittal sinus. A thoracic MRI (Left top 2 images) was obtained in a 60-year-old man presenting with symptoms of thoracic myelopathy, which showed cord signal change extending from the T5 level to the conus as well as a serpiginous appearing flow void posterior to the spinal cord concerning for a spinal dural arteriovenous fistula. A catheter angiogram was then performed (right).
Contributed by G Gould, MD, and S Zyck, MD
(Click Image to Enlarge)
References
Gonzalez-Araiza G, Haddad L, Patel S, Karageorgiou J. Percutaneous Embolization of a Postsurgical Prostatic Artery Pseudoaneurysm and Arteriovenous Fistula. Journal of vascular and interventional radiology : JVIR. 2019 Feb:30(2):269-271. doi: 10.1016/j.jvir.2018.11.011. Epub [PubMed PMID: 30717965]
Faughnan ME, Lui YW, Wirth JA, Pugash RA, Redelmeier DA, Hyland RH, White RI Jr. Diffuse pulmonary arteriovenous malformations: characteristics and prognosis. Chest. 2000 Jan:117(1):31-8 [PubMed PMID: 10631195]
Level 2 (mid-level) evidenceAntoniou GA, Lazarides MK, Georgiadis GS, Sfyroeras GS, Nikolopoulos ES, Giannoukas AD. Lower-extremity arteriovenous access for haemodialysis: a systematic review. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2009 Sep:38(3):365-72. doi: 10.1016/j.ejvs.2009.06.003. Epub 2009 Jul 10 [PubMed PMID: 19596598]
Level 1 (high-level) evidenceNepal S,Annamaraju P, Coronary Arteriovenous Fistula 2020 Jan; [PubMed PMID: 32119505]
Demirci O, Celayir A. Prenatal diagnosis and treatment of intrahepatic arteriovenous fistulas: case reports and the literature review. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians. 2022 Mar:35(5):837-845. doi: 10.1080/14767058.2020.1731466. Epub 2020 Apr 2 [PubMed PMID: 32241194]
Level 3 (low-level) evidenceJha AK, Sunder A. An unusual case of pulmonary arterio-venous fistula (PAVF). Journal of family medicine and primary care. 2019 Oct:8(10):3408-3411. doi: 10.4103/jfmpc.jfmpc_580_19. Epub 2019 Oct 31 [PubMed PMID: 31742178]
Level 3 (low-level) evidenceKandemirli SG, Kizilkaya MH, Erdemli Gursel B, Akca T, Bostan OM. Congenital arteriovenous fistula between descending aorta and the left innominate vein. Surgical and radiologic anatomy : SRA. 2020 Apr:42(4):401-404. doi: 10.1007/s00276-019-02282-z. Epub 2019 Jul 10 [PubMed PMID: 31292677]
Reynolds MR,Lanzino G,Zipfel GJ, Intracranial Dural Arteriovenous Fistulae. Stroke. 2017 May; [PubMed PMID: 28432263]
Kléber AG. Consequences of acute ischemia for the electrical and mechanical function of the ventricular myocardium. A brief review. Experientia. 1990 Dec 1:46(11-12):1162-7 [PubMed PMID: 2253715]
Guneyli S, Cinar C, Bozkaya H, Korkmaz M, Oran I. Endovascular management of congenital arteriovenous fistulae in the neck. Diagnostic and interventional imaging. 2016 Sep:97(9):871-5. doi: 10.1016/j.diii.2015.08.006. Epub 2016 Mar 11 [PubMed PMID: 26972281]
Ying A, Al-Asady R, Vicaretti M. Endovascular treatment of a large iatrogenic popliteal arteriovenous fistula. Journal of vascular surgery cases and innovative techniques. 2020 Mar:6(1):129-132. doi: 10.1016/j.jvscit.2019.10.010. Epub 2020 Feb 21 [PubMed PMID: 32123780]
Level 3 (low-level) evidencePetrov I,Tasheva I,Stankov Z,Polomski P,Georgieva G,Marinov K, Uneventful Follow-Up 2 Years after Endovascular Treatment of a High-Flow Iatrogenic Aortocaval Fistula Causing Pulmonary Hypertension and Right Heart Failure. Methodist DeBakey cardiovascular journal. 2019 Apr-Jun; [PubMed PMID: 31384380]
Farshidmehr P, Zafarghandi MR, Sadat A, Sayarifard A. Coil Embolization of an Iatrogenic Arteriovenous Fistula between the Superior Mesenteric Artery and Vein: A Case Report. The journal of Tehran Heart Center. 2019 Jan:14(1):37-39 [PubMed PMID: 31210769]
Level 3 (low-level) evidenceŞahin M, Yücel C, Kanber EM, İlal Mert FT, Bıçakhan B. Management of traumatic arteriovenous fistulas: A tertiary academic center experience. Ulusal travma ve acil cerrahi dergisi = Turkish journal of trauma & emergency surgery : TJTES. 2018 May:24(3):234-238. doi: 10.5505/tjtes.2017.49060. Epub [PubMed PMID: 29786818]
Davison BD, Polak JF. Arterial injuries: a sonographic approach. Radiologic clinics of North America. 2004 Mar:42(2):383-96 [PubMed PMID: 15136023]
Van den Broecke M, Vereecke E, De Visschere P. Renal Arteriovenous Fistula. Journal of the Belgian Society of Radiology. 2020 Jan 31:104(1):10. doi: 10.5334/jbsr.2032. Epub 2020 Jan 31 [PubMed PMID: 32025626]
Fox CJ, Gillespie DL, O'Donnell SD, Rasmussen TE, Goff JM, Johnson CA, Galgon RE, Sarac TP, Rich NM. Contemporary management of wartime vascular trauma. Journal of vascular surgery. 2005 Apr:41(4):638-44 [PubMed PMID: 15874928]
Level 2 (mid-level) evidenceKim JW, Kim SJ, Kim MR. Traumatic carotid-cavernous sinus fistula accompanying abducens nerve (VI) palsy in blowout fractures: missed diagnosis of 'white-eyed shunt'. International journal of oral and maxillofacial surgery. 2013 Apr:42(4):470-3. doi: 10.1016/j.ijom.2013.01.007. Epub 2013 Feb 14 [PubMed PMID: 23415244]
Level 3 (low-level) evidenceStathis A, Gan J. Traumatic arteriovenous fistula: a 25-year delay in presentation. Journal of surgical case reports. 2020 Mar:2020(3):rjaa042. doi: 10.1093/jscr/rjaa042. Epub 2020 Mar 24 [PubMed PMID: 32226601]
Level 3 (low-level) evidenceCuoco JA, Guilliams EL, Klein BJ, Malaty GR, Witcher MR, Entwistle JJ. N-butyl cyanoacrylate embolization of a traumatic pseudoaneurysm and arteriovenous fistula of the middle meningeal artery. Radiology case reports. 2020 Apr:15(4):321-325. doi: 10.1016/j.radcr.2019.12.009. Epub 2020 Jan 20 [PubMed PMID: 31993092]
Level 3 (low-level) evidenceDickey KW, Pollak JS, Meier GH 3rd, Denny DF, White RI Jr. Management of large high-flow arteriovenous malformations of the shoulder and upper extremity with transcatheter embolotherapy. Journal of vascular and interventional radiology : JVIR. 1995 Sep-Oct:6(5):765-73 [PubMed PMID: 8541682]
HUGHES CW. Arterial repair during the Korean war. Annals of surgery. 1958 Apr:147(4):555-61 [PubMed PMID: 13521671]
Baldini M, Catania A, Orsatti A, Manfredi MG, Motta P, Cantalamessa L. Inhibitory effect of somatostatin on abnormal GH response to TRH in primary hypothyroidism. Experimental and clinical endocrinology. 1992:99(2):80-3 [PubMed PMID: 1353454]
Zamani H, Meragi M, Arabi Moghadam MY, Alizadeh B, Babazadeh K, Mokhtari-Esbuie F. Clinical presentation of coronary arteriovenous fistula according to age and anatomic orientation. Caspian journal of internal medicine. 2015 Spring:6(2):108-12 [PubMed PMID: 26221510]
Allon M, Ornt DB, Schwab SJ, Rasmussen C, Delmez JA, Greene T, Kusek JW, Martin AA, Minda S. Factors associated with the prevalence of arteriovenous fistulas in hemodialysis patients in the HEMO study. Hemodialysis (HEMO) Study Group. Kidney international. 2000 Nov:58(5):2178-85 [PubMed PMID: 11044239]
Level 1 (high-level) evidenceNagpal K, Ahmed K, Cuschieri R. Diagnosis and management of acute traumatic arteriovenous fistula. The International journal of angiology : official publication of the International College of Angiology, Inc. 2008 Winter:17(4):214-6 [PubMed PMID: 22477453]
Level 3 (low-level) evidenceHashimoto O, Miyazaki T, Hosokawa J, Shimura Y, Okuyama H, Endo M. A case of high-output heart failure caused by a femoral arteriovenous fistula after endovenous laser ablation treatment of the saphenous vein. Phlebology. 2015 May:30(4):290-2. doi: 10.1177/0268355514525149. Epub 2014 Feb 19 [PubMed PMID: 24553135]
Level 3 (low-level) evidenceMiller-Thomas MM, West OC, Cohen AM. Diagnosing traumatic arterial injury in the extremities with CT angiography: pearls and pitfalls. Radiographics : a review publication of the Radiological Society of North America, Inc. 2005 Oct:25 Suppl 1():S133-42 [PubMed PMID: 16227487]
Biswas S, Chandran A, Radon M, Puthuran M, Bhojak M, Nahser HC, Das K. Accuracy of four-dimensional CT angiography in detection and characterisation of arteriovenous malformations and dural arteriovenous fistulas. The neuroradiology journal. 2015 Aug:28(4):376-84. doi: 10.1177/1971400915604526. Epub 2015 Oct 1 [PubMed PMID: 26427892]
In 't Veld M, Fronczek R, Dos Santos MP, van Walderveen MAA, Meijer FJA, Willems PWA. High sensitivity and specificity of 4D-CTA in the detection of cranial arteriovenous shunts. European radiology. 2019 Nov:29(11):5961-5970. doi: 10.1007/s00330-019-06234-4. Epub 2019 May 14 [PubMed PMID: 31089848]
Ares WJ, Jankowitz BT, Tonetti DA, Gross BA, Grandhi R. A comparison of digital subtraction angiography and computed tomography angiography for the diagnosis of penetrating cerebrovascular injury. Neurosurgical focus. 2019 Nov 1:47(5):E16. doi: 10.3171/2019.8.FOCUS19495. Epub [PubMed PMID: 31675711]
Georgiadis GS, Charalampidis DG, Argyriou C, Georgakarakos EI, Lazarides MK. The Necessity for Routine Pre-operative Ultrasound Mapping Before Arteriovenous Fistula Creation: A Meta-analysis. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2015 May:49(5):600-5. doi: 10.1016/j.ejvs.2015.01.012. Epub 2015 Feb 27 [PubMed PMID: 25736517]
Level 1 (high-level) evidenceMarin ML, Veith FJ, Panetta TF, Cynamon J, Barone H, Schonholz C, Parodi JC. Percutaneous transfemoral insertion of a stented graft to repair a traumatic femoral arteriovenous fistula. Journal of vascular surgery. 1993 Aug:18(2):299-302 [PubMed PMID: 8350439]
Level 3 (low-level) evidenceNuman F, Omeroglu A, Kara B, Cantaşdemir M, Adaletli I, Kantarci F. Embolization of peripheral vascular malformations with ethylene vinyl alcohol copolymer (Onyx). Journal of vascular and interventional radiology : JVIR. 2004 Sep:15(9):939-46 [PubMed PMID: 15361561]
Zaki Ghali G, Zaki Ghali MG, Zaki Ghali E. Transvenous embolization of arteriovenous malformations. Clinical neurology and neurosurgery. 2019 Mar:178():70-76. doi: 10.1016/j.clineuro.2018.08.024. Epub 2018 Sep 11 [PubMed PMID: 30731326]
Guo H, Wang C, Yang M, Tong X, Wang J, Guan H, Song L, Zou Y. Management of iatrogenic renal arteriovenous fistula and renal arterial pseudoaneurysm by transarterial embolization: A single center analysis and outcomes. Medicine. 2017 Oct:96(40):e8187. doi: 10.1097/MD.0000000000008187. Epub [PubMed PMID: 28984770]
Lee BB, Kim DI, Huh S, Kim HH, Choo IW, Byun HS, Do YS. New experiences with absolute ethanol sclerotherapy in the management of a complex form of congenital venous malformation. Journal of vascular surgery. 2001 Apr:33(4):764-72 [PubMed PMID: 11296330]
Nosher JL, Murillo PG, Liszewski M, Gendel V, Gribbin CE. Vascular anomalies: A pictorial review of nomenclature, diagnosis and treatment. World journal of radiology. 2014 Sep 28:6(9):677-92. doi: 10.4329/wjr.v6.i9.677. Epub [PubMed PMID: 25276311]
CREECH O Jr, GANTT J, WREN H. TRAUMATIC ARTERIOVENOUS FISTULA AT UNUSUAL SITES. Annals of surgery. 1965 Jun:161(6):908-20 [PubMed PMID: 14295942]
Brinjikji W, Nasr DM, Morris JM, Rabinstein AA, Lanzino G. Clinical Outcomes of Patients with Delayed Diagnosis of Spinal Dural Arteriovenous Fistulas. AJNR. American journal of neuroradiology. 2016 Feb:37(2):380-6. doi: 10.3174/ajnr.A4504. Epub 2015 Sep 3 [PubMed PMID: 26338916]
Level 2 (mid-level) evidenceReddy YNV, Melenovsky V, Redfield MM, Nishimura RA, Borlaug BA. High-Output Heart Failure: A 15-Year Experience. Journal of the American College of Cardiology. 2016 Aug 2:68(5):473-482. doi: 10.1016/j.jacc.2016.05.043. Epub [PubMed PMID: 27470455]
Reddy SN, Boros MC, Horrow MM. Approach to the Swollen Arm With Chronic Dialysis Access: It's Not Just Deep Vein Thrombosis. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2015 Oct:34(10):1901-10. doi: 10.7863/ultra.15.14.11063. Epub 2015 Aug 25 [PubMed PMID: 26307123]
Handlos P, Marecová K, Smatanová M, Dvořáček I, Dobiáš M. Fatal Hemorrhage from an Arteriovenous Fistula. Journal of forensic sciences. 2018 Sep:63(5):1577-1581. doi: 10.1111/1556-4029.13730. Epub 2018 Jan 16 [PubMed PMID: 29341134]