Introduction
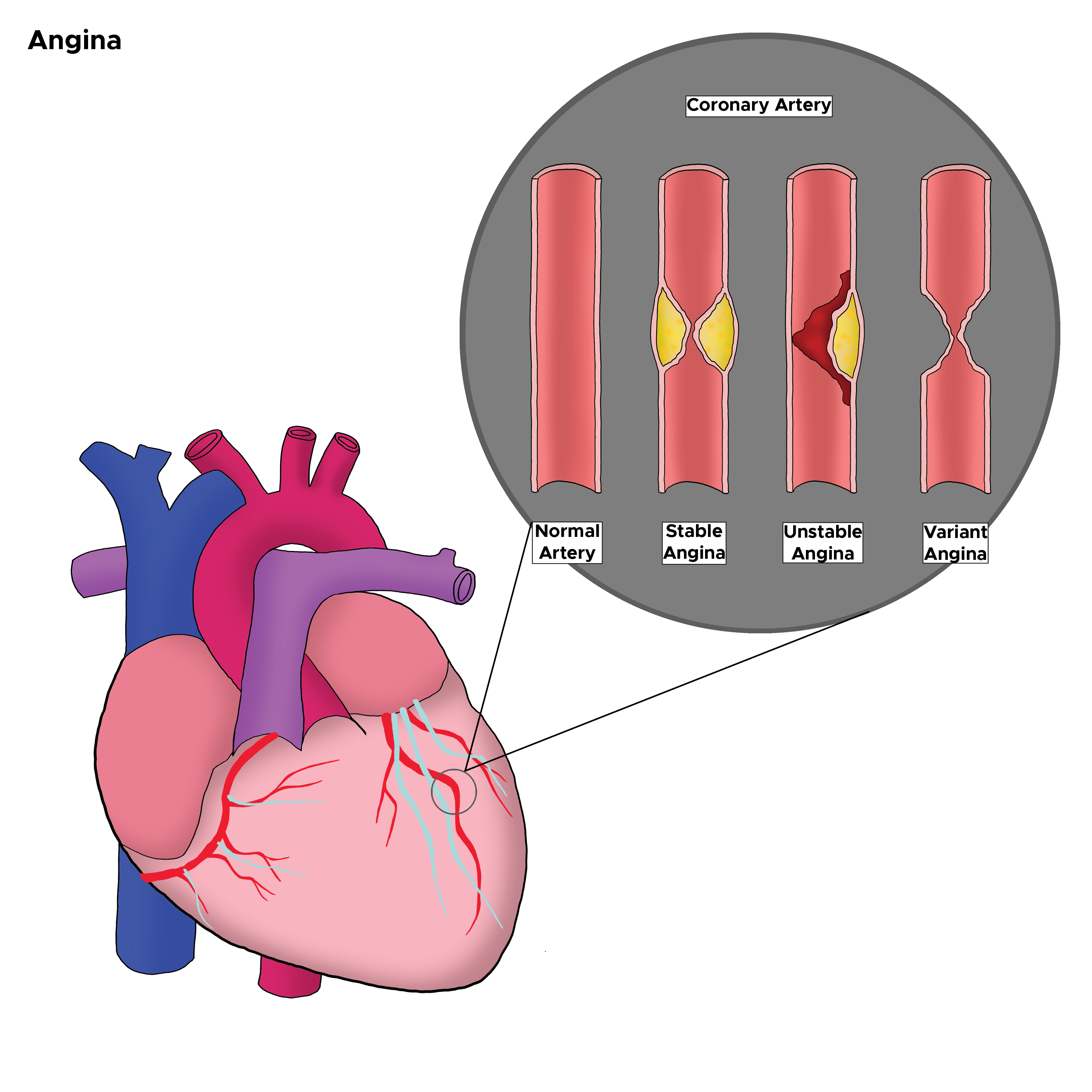
Angina, or chest pain, is the most common symptom of ischemic heart disease, a major cause of morbidity and mortality worldwide. Chest pain can be due to non-cardiac and cardiac causes, and thorough history and physical is critical in differentiating these causes and identifying patients experiencing acute coronary syndrome. Angina is one of the signs of acute coronary syndrome (ACS) and can further subdivide into stable and unstable angina. Stable angina defines as the occurrence of symptoms with exertion only. Unstable angina or symptoms occurring at rest requires more prompt evaluation and management. Approximately 9 million patients in the United States have symptoms of angina, and recognizing these symptoms is imperative in improving patient outcomes.[1]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Chest pain can be due to non-cardiac causes, non-ischemic cardiac disease, and, finally, ischemic cardiac disease. Non-cardiac causes include gastroesophageal reflux disease, lung disease, musculoskeletal causes, and anxiety/panic attacks. Non-ischemic cardiac causes include pericardial disease. The etiology of chest pain caused by cardiac ischemia is largely accepted to be due to atherosclerosis of coronary arteries and coronary vasospasm.[1] This condition leads to myocardial oxygen supply and demand mismatch. In stable angina, the increased demand only occurs with exertion, but in unstable angina, it also happens at rest. Increased myocardial oxygen demand from exercise is most notably due to increased heart rate, increased blood pressure, and increased myocardial contractility, among other factors.[2] Under normal cardiac physiologic conditions, increased oxygen demand occurring with exertion is followed by coronary vasodilation, but in cases of coronary artery atherosclerosis, this function is impeded, and ischemia and chest pain ensue.[1] Vasospastic angina, otherwise known as variant angina or Prinzmetal angina, like stable angina, also occurs at rest but is unrelated to coronary atherosclerosis.[3]
Epidemiology
Chronic stable angina affects approximately 30000 to 40000 people per million people in Western countries.[2] Prevalence increases with age in both men and women. The estimates are prevalence for men and women 45 to 64 years old are 4 to 7% and 5 to 7%, respectively. In men and women 65 to 84 years old, the estimated prevalence is 14 to 15% and 10 to 12%, respectively.[2]
Modifiable risk factors for angina include hyperlipidemia, hypertension, current or past tobacco use, diabetes mellitus, and obesity/metabolic syndrome. Increasing BMI is an independent risk factor for coronary arterial disease (CAD).[4] Non-modifiable risk factors include increasing age, male sex, family history of CAD, and ethnic origin.[5]
Pathophysiology
The heart is dependent on an adequate oxygen supply for energy production to support contractility. At the cellular level, ischemia causes an increase in anaerobic glycolysis. This increases the levels of hydrogen, potassium, and lactate in the venous return of the ischemic or affected area of the myocardium. The hydrogen ions compete with calcium ions causing hypokinesia/akinesia of the affected area. For stable angina, this change in oxygen supply requires a trigger that would cause metabolic mismatch— exercise, stress, and low temperature.[1]
History and Physical
Patients with ACS most commonly present with angina, which patients usually describe as pain, pressure, tightness, or heaviness in the chest, with potential radiation to the jaw or left arm. It may be accompanied by shortness of breath, diaphoresis, nausea, or any combination of the above. The chest pain may be precipitated by exertion and relieved by rest and/or nitroglycerin in the case of stable angina. In cases of unstable angina or myocardial infarction (MI) [non-ST segment elevation MI (NSTEMI)/ST-segment elevation MI (STEMI)], the chest pain will likely not fully resolve with rest or nitroglycerin. In the case of stable angina, the symptoms may last 5 minutes before resolving after rest or the use of nitroglycerin.[5] Although these are classic signs of ACS, classic angina may not occur in some patients, especially diabetics, so one must have a high index of suspicion in patients with significant cardiac risk factors.
A physical exam may be unremarkable; however, the patient may appear uncomfortable or anxious. He or she may be diaphoretic or clutching his or her chest. Vital signs may be normal or reveal tachycardia and tachypnea most commonly.
Evaluation
In patients presenting with angina, the value of cardiac testing is determined by the patient’s pretest, probability of ACS. Pretest probability is evaluated by considering the patient’s presentation, along with their cardiac risk factors. In patients with very high or very low pretest probability, diagnostic tests are less valuable as they are less likely to change management.[5]
Initial testing includes a 12-lead electrocardiogram (ECG), chest X-ray, and basic lab testing, including complete blood count (CBC), and basic metabolic profile (BMP), along with serial troponin levels if ACS is suspected. ECG may not show any abnormalities in the cases of stable angina, unstable angina, or NSTEMI. ECG findings of myocardial ischemia include T-wave flattening or inversions, or ST-segment depressions. Further testing may include exercise or pharmacologic stress testing with or without nuclear perfusion imaging and diagnostic heart catheterization. ECG changes will appear in STEMIs and prompt an immediate need for coronary revascularization.
Treatment / Management
Treatment of chronic stable angina is aimed at managing symptoms as well as slowing the progression to cardiac events. Management is multifactorial and involves lifestyle modifications, risk factor modification, and medical therapy as essential components of treatment.[6] In cases in which symptoms are refractory to medical therapy, revascularization may be attempted; however, although it may be successful in controlling symptoms, it is not shown to reduce major cardiovascular events compared with medical therapy.[7](A1)
Lifestyle modifications include regular exercise, weight control, and smoking cessation, which should be encouraged. Risk factor modification includes controlling blood pressure, cholesterol, and blood sugar. Medications for risk factor modification and to prevent disease progression include aspirin, statins, angiotensin-converting enzyme inhibitors, or angiotensin receptor blockers.[6]
Medical therapy can be used to control symptoms as well as help mitigate the risk of the progression of atherosclerosis and cardiac events.[6] Antianginal agents can be separated based on the mechanism of symptom relief in angina. In general, symptomatic control is achieved by way of decreasing myocardial oxygen consumption.
As heart rate is the main influencer of oxygen consumption, most anginal events are initiated by an increase in heart rate.[1] Three classes of drugs used for angina reduce symptoms by way of heart rate reduction— beta-blockers, ivabradine, and non-dihydropyridine calcium channel blockers. Calcium channel blockers should be avoided in patients with left ventricular dysfunction and decreased ejection fraction.
Another mechanism by which anginal symptoms can be treated is vascular smooth muscle relaxation. This leads to coronary artery dilatation, thereby increasing perfusion ability. The drugs that work on this mechanism are dihydropyridine calcium channel blockers, nitrates, and nicorandil.[1]
Another drug used for chronic stable angina is ranolazine, which inhibits the late sodium current in ventricular myocardial cells. This reduces diastolic contractile dysfunction.[8]
Treatment for unstable angina is aimed at pain reduction, limiting damage to the myocardium, and decreasing morbidity and mortality.
Nitrates - no mortality benefit, but used for chest pain relief. They cause vasodilation, which decreases preload and left ventricular end-diastolic volume. This reduces myocardial oxygen consumption. They are contraindicated in cases of hypotension and previous use of phosphodiesterase inhibitors within the past 48 hours.[9]
Morphine - no mortality benefit, used for pain relief when pain relief is not fully achieved by nitrates. It causes some vasodilation aside from analgesia.
Beta-blockers - reduce mortality. They cause a decrease in heart rate, contractility, and blood pressure, thereby reducing myocardial oxygen demand.[9]
Antiplatelet agents - dual therapy with aspirin and either clopidogrel, ticagrelor, or prasugrel decrease the risk of cardiovascular events in patients with acute coronary syndromes— acute myocardial infarction, cardiovascular death, and stroke.[9][10](A1)
Anticoagulants - reduce mortality by decreasing re-infarction rates in combination with antiplatelet agents. Used intravenously for acute treatment.[9]
Anatomic assessment of coronary arteries/consideration of revascularization - high-risk patients should be identified with risk stratification methods and considered for urgent revascularization.[9]
Differential Diagnosis
The differential diagnosis of angina can divide into body systems:
- Gastrointestinal: gastroesophageal reflux, hiatal hernia, peptic ulcer disease
- Pulmonary: pneumothorax, pneumonia, pulmonary embolism
- Musculoskeletal: costochondritis, rib injury, muscle spasm, chest wall injury
- Psychiatric: panic attack, generalized anxiety
- Cardiac non-ischemic: pericarditis, myocarditis
- Vascular: aortic dissection
Prognosis
The prognosis of chronic stable angina progression to cardiac events varies among patients. Factors affecting prognosis include cardiovascular comorbidities as well as compliance with lifestyle modifications and medical treatment plans. Long-term prognosis is also affected by left ventricular systolic function, the degree of exercise the patient can tolerate, and the extent of CAD present.[1]
Risk factors for poorer prognosis are diabetes mellitus, previous MI, hypertension, increasing age, and male sex.[11] The use of nitrates has also been demonstrated to be a negative prognostic indicator of mortality, likely because their use indicates more advanced disease.
Complications
As the initial symptom of CAD in many cases, the main complication of angina is a future cardiac event, such as myocardial infarction. In one study, estimates are that the 10-year risk of MI exceeded 10 percent in women with chronic stable angina starting from when they initially began to use nitrates to treat symptoms.[12]
Aside from this potentially fatal complication, chronic stable angina has implications for society as well as patients. These include lower quality of life due to decreased ability to perform daily activities, as well as an increased burden to society from indirect costs, such as early retirement or disability.[1] Angina treatment should be aimed not only at improving mortality but also at treating symptoms so patients can be more active.[13]
Deterrence and Patient Education
Patients with cardiac risk factors should be monitored for symptoms of angina and receive education about alarming signs, such as symptoms occurring at rest and symptoms no longer relieved by nitrates. It is imperative to stress risk factor modification as an essential component of treatment to slow progression. So, dietary and exercise education, along with smoking cessation counseling, if applicable, is beneficial. It is important to stress compliance with medications, as well.
Enhancing Healthcare Team Outcomes
Recognizing the symptoms of angina is critical to making a diagnosis of CAD, but similar symptoms can present in many other conditions. The interprofessional team must recognize signs of cardiac vs. non-cardiac chest pain and understand that the etiology may not be clear based solely on the quality of pain. In specific patient populations, such as patients with diabetes, the presentation may be more inconspicuous. Understanding the patient's medical history and family history is critical to making the diagnosis. In the presence of cardiac risk factors, the clinician must have a high index of suspicion for a cardiac etiology and conduct further workup, versus when risk factors are absent.
While the cardiologist is the team leader in the treatment and management of these patients, it is the primary care physician who usually completes the initial workup and makes the diagnosis in many cases. It is vital to obtain an accurate history and physical and have an open line of communication between physicians, or else the clinician may miss the diagnosis. A missed diagnosis increases morbidity and mortality for these patients as it may delay their treatment.
As the management of the condition progresses, cardiology nurses play an essential role in monitoring, assessing patient compliance with treatment regimens, and encouraging lifestyle changes. The pharmacist will weigh in on the patient's medication regimen by evaluating the effectiveness of chosen agents, checking for drug-drug interactions, and verifying dosing. With this type of interprofessional collaboration, patients with angina can experience increased quality of life and avoid future morbidity. [Level 5]
Media
(Click Image to Enlarge)
References
Balla C, Pavasini R, Ferrari R. Treatment of Angina: Where Are We? Cardiology. 2018:140(1):52-67. doi: 10.1159/000487936. Epub 2018 Jun 6 [PubMed PMID: 29874661]
Ferrari R, Camici PG, Crea F, Danchin N, Fox K, Maggioni AP, Manolis AJ, Marzilli M, Rosano GMC, Lopez-Sendon JL. Expert consensus document: A 'diamond' approach to personalized treatment of angina. Nature reviews. Cardiology. 2018 Feb:15(2):120-132. doi: 10.1038/nrcardio.2017.131. Epub 2017 Sep 7 [PubMed PMID: 28880025]
Level 3 (low-level) evidencePicard F, Sayah N, Spagnoli V, Adjedj J, Varenne O. Vasospastic angina: A literature review of current evidence. Archives of cardiovascular diseases. 2019 Jan:112(1):44-55. doi: 10.1016/j.acvd.2018.08.002. Epub 2018 Sep 7 [PubMed PMID: 30197243]
Wolk R, Berger P, Lennon RJ, Brilakis ES, Somers VK. Body mass index: a risk factor for unstable angina and myocardial infarction in patients with angiographically confirmed coronary artery disease. Circulation. 2003 Nov 4:108(18):2206-11 [PubMed PMID: 14557360]
Level 2 (mid-level) evidenceMancini GB, Gosselin G, Chow B, Kostuk W, Stone J, Yvorchuk KJ, Abramson BL, Cartier R, Huckell V, Tardif JC, Connelly K, Ducas J, Farkouh ME, Gupta M, Juneau M, O'Neill B, Raggi P, Teo K, Verma S, Zimmermann R, Canadian Cardiovascular Society. Canadian Cardiovascular Society guidelines for the diagnosis and management of stable ischemic heart disease. The Canadian journal of cardiology. 2014 Aug:30(8):837-49. doi: 10.1016/j.cjca.2014.05.013. Epub 2014 May 28 [PubMed PMID: 25064578]
Wee Y, Burns K, Bett N. Medical management of chronic stable angina. Australian prescriber. 2015 Aug:38(4):131-6 [PubMed PMID: 26648642]
Boden WE, O'Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, Knudtson M, Dada M, Casperson P, Harris CL, Chaitman BR, Shaw L, Gosselin G, Nawaz S, Title LM, Gau G, Blaustein AS, Booth DC, Bates ER, Spertus JA, Berman DS, Mancini GB, Weintraub WS, COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. The New England journal of medicine. 2007 Apr 12:356(15):1503-16 [PubMed PMID: 17387127]
Level 1 (high-level) evidenceRayner-Hartley E, Sedlak T. Ranolazine: A Contemporary Review. Journal of the American Heart Association. 2016 Mar 15:5(3):e003196. doi: 10.1161/JAHA.116.003196. Epub 2016 Mar 15 [PubMed PMID: 26979079]
Silva FM, Pesaro AE, Franken M, Wajngarten M. Acute management of unstable angina and non-ST segment elevation myocardial infarction. Einstein (Sao Paulo, Brazil). 2015 Jul-Sep:13(3):454-61. doi: 10.1590/S1679-45082015RW3172. Epub [PubMed PMID: 26466065]
Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK, Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. The New England journal of medicine. 2001 Aug 16:345(7):494-502 [PubMed PMID: 11519503]
Level 1 (high-level) evidenceHjemdahl P, Eriksson SV, Held C, Forslund L, Näsman P, Rehnqvist N. Favourable long term prognosis in stable angina pectoris: an extended follow up of the angina prognosis study in Stockholm (APSIS). Heart (British Cardiac Society). 2006 Feb:92(2):177-82 [PubMed PMID: 15951393]
Level 2 (mid-level) evidenceHemingway H, McCallum A, Shipley M, Manderbacka K, Martikainen P, Keskimäki I. Incidence and prognostic implications of stable angina pectoris among women and men. JAMA. 2006 Mar 22:295(12):1404-11 [PubMed PMID: 16551712]
Level 2 (mid-level) evidenceKloner RA, Chaitman B. Angina and Its Management. Journal of cardiovascular pharmacology and therapeutics. 2017 May:22(3):199-209. doi: 10.1177/1074248416679733. Epub 2016 Dec 14 [PubMed PMID: 28196437]