Introduction
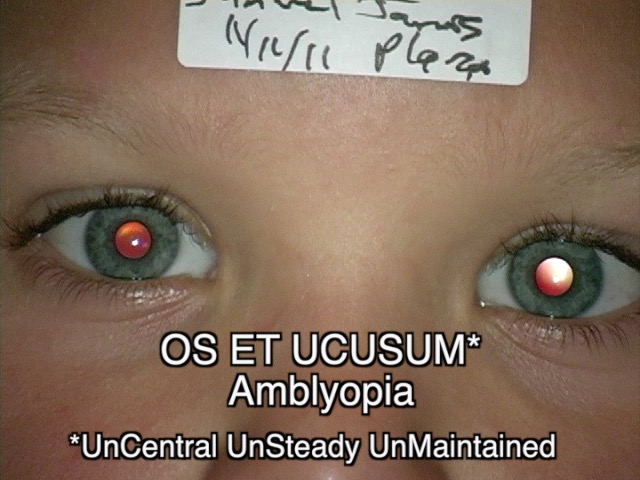
Amblyopia is a developmental disorder that affects vision. Characterized by neurodevelopmental alterations, amblyopia leads to physiological abnormalities in visual pathway development during early childhood, resulting in impaired vision occurring unilaterally or, less commonly, in both eyes.[1] This condition occurs when cortical visual development fails in one or both eyes early in life. Amblyopia is commonly known as a "lazy eye" among the general public. If left untreated, amblyopia can lead to permanent vision loss in the affected eye, even if the underlying ocular pathology is later resolved.
Among children and young adults, amblyopia is the most common cause of decreased vision in a single eye, affecting approximately 2% to 4% of children.[2] The development of this condition is often linked to factors such as visual deprivation, inadequate quality of visual stimulation, or disruptions in binocular ocular interactions during the critical period of pediatric development.[3] Patients with amblyopia typically exhibit reduced best-corrected visual acuity (BCVA), which cannot be attributed to structural alterations in the eye.
Amblyopia presents early in life when the developing visual system fails to transmit a clear and focused image to the visual cortex.[4] Various factors such as media opacities, cataracts, strabismus, or anisometropic refractive errors, which create a developmental disadvantage for one eye over the other, can cause amblyopia. While amblyopia is typically unilateral, there are rare instances where it can occur bilaterally, especially in cases involving cataracts in both eyes or high refractive errors. The visual experiences during infancy and childhood play a pivotal role in shaping adult vision.[5][6]
Amblyopia is diagnosed by identifying diminished visual acuity in one or both eyes that is out of proportion to the structural abnormality of the eye, excluding any other visual disorders as the underlying cause. Diagnosis often involves identifying an interocular difference of 2 lines or more in visual acuity when refractive errors are corrected. In the case of young children, measuring visual acuity can be challenging. Still, it can be estimated by observing their reactions when one eye is covered, including assessing their ability to track objects with a single eye.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Amblyopia can be categorized based on its underlying causes, referred to as refractive, strabismic, visual deprivation, and occlusion (reverse).[7]
Refractive Amblyopia
Refractive amblyopia is caused by untreated refractive errors unilaterally or in both eyes.[8] This condition results from blurred visual input caused by hyperopia, astigmatism, or myopia, typically with a difference of refractive error exceeding 1 diopter (D) between the eyes.[9] Generally, eyes with hyperopia or astigmatism are more prone to developing amblyopia than myopia, as myopic eyes can still maintain a clear focus on nearby objects.
Anisometric amblyopia is a type of vision impairment occurring in 1 eye due to uncorrected and unequal refractive errors between the eyes, which results in a poorly focused image primarily affecting the weaker eye and can manifest with or without strabismus.[10] Research has shown that the risk and severity of amblyopia are correlated with the degree of anisometropia, refractive error magnitude, and astigmatism.[11]
While bilateral refractive amblyopia is less common, it can occur when both eyes consistently receive blurred images on their retinas due to severe uncorrected refractive errors during development. The first-line treatment for individuals with bilateral refractive amblyopia involves a thorough assessment of BCVA and the prescription of corrected lenses to fully correct the underlying refractive errors.
Strabismic Amblyopia
This condition can develop when both eyes fail to align correctly. In pediatric cases, the brain employs a mechanism to prevent diplopia by suppressing the visual input from one eye, leading to impaired visual development in that eye.[12] In these individuals, both retinas receive stimulation in noncorresponding areas, hindering the establishment of proper binocular vision and the fusion of images from both eyes (see Image. Bilateral Extropia). Consequently, the suppression of visual input primarily affects the amblyopic eye.[13]
In cases of amblyopia associated with strabismus, the tropia, or deviation of the eye from its normal position concerning the central line of vision, tends to be unequal and not alternating. Such conditions are usually observed in patients with esodeviations (see Image. Esotropia of Right Eye).
While strabismus can be treated through methods like surgery or the use of prism glasses to realign the eyes, amblyopia can persist despite treating the underlying strabismus. This highlights the necessity of addressing amblyopia directly through appropriate therapies to restore visual function in the affected eye.
Visual Deprivation Amblyopia
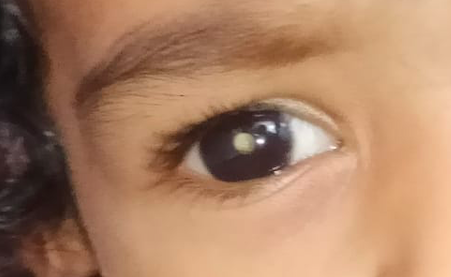
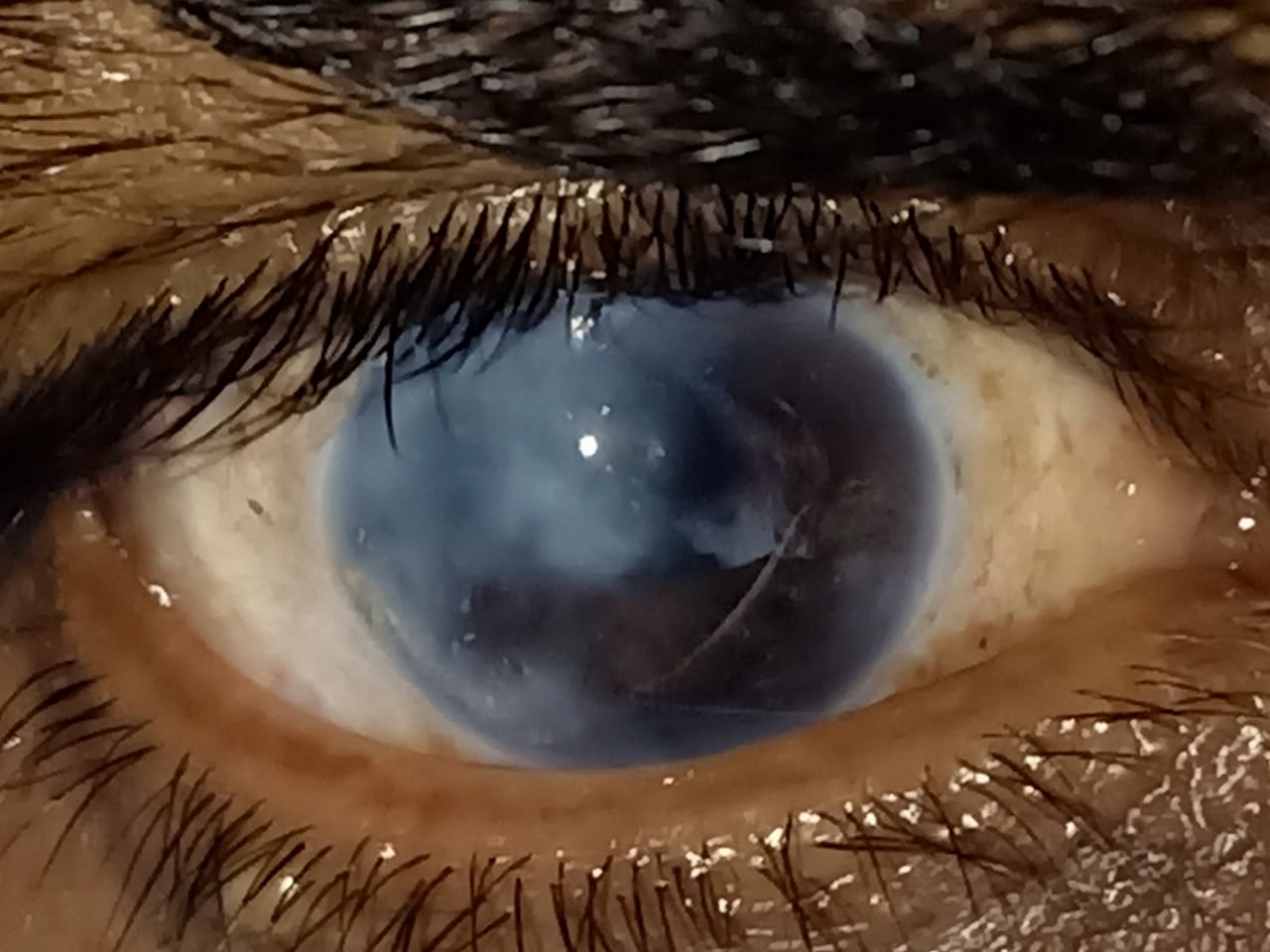
Deprivation amblyopia occurs due to any pathology that obstructs the visual pathway, leading to partial or complete blockage and consequently causing blurred or degraded images to be projected onto the retina.[9] Various factors, including early-onset or congenital cataracts, corneal opacity (see Image. Corneal Opacity in Young Child), intraocular inflammation of either noninfectious or infectious origin, vitreous hemorrhage, retina damage, optic nerve pathologies, or ptosis (see Image. Congenital Ptosis) can contribute to this obstruction.[14] Visual deprivation amblyopia can even result from the absence of visual stimuli, such as covering one eye or living in complete darkness.
Although deprivation is the least common form of amblyopia, it tends to be the most severe and challenging form to treat. The prognosis for patients with this condition is usually more favorable when early intervention (within the first 2 months of age) is undertaken, particularly in cases involving the removal of cataracts or the cause of the optical opacity.[15]
Occlusion or Reverse Amblyopia
Occlusion amblyopia is uncommon, resulting from prolonged visual deprivation in the healthy eye, often induced by pharmaceutical cycloplegia or therapeutic patching.[16] Research has indicated that BCVA may decline by more than 2 lines following 6 months of daily patching for 6 hours daily or topical atropine in the nonamblyopic eye.[17] This form of iatrogenic-induced amblyopia is quite rare.
Visual acuity typically returns to normal once atropine or patching is discontinued, and optimal refractive correction spectacles are used for the healthy eye. This underscores the importance of promptly monitoring and managing occlusion amblyopia to ensure the best visual outcomes.
The severity of resulting amblyopia tends to be more pronounced when the degree of visual deprivation is greater. The critical period for visual development is primarily concentrated within the first 7 years of life, with the initial few years and even months being particularly critical.[18] Delaying the start of amblyopia treatment makes it increasingly challenging to achieve clinical reversal of the condition. Early-onset visual deprivation can lead to permanent anatomic alterations in the magnocellular (M) and parvocellular (P) visual pathways.
For this reason, surgical intervention may be necessary very early, often within a week of discovery, when dealing with dense congenital monocular cataracts. Even a few months of having a congenital cataract could potentially cause irreversible amblyopia. There is typically a bit more flexibility in cases of binocular cataracts with equal density, allowing for intervention within a few weeks.[19][20]
Epidemiology
Amblyopia presents a significant global health concern owing to its prevalence and the potential for permanent visual impairment if it is not promptly diagnosed and treated.[21][22] Historically, various forms of amblyopia have been reported to affect up to 3% of the population, with a 1.2% lifetime risk of vision loss attributed to this condition.[23] More recent data suggest that the global prevalence of amblyopia falls within the range of 1.1% to 1.8%.[24][25][26]
Population-based studies have reported varying prevalence rates, with estimates ranging from 0.7% to 2.6% among children aged 30 to 70 months and 1.0% to 5.5% in older children.[27] The reported prevalence of amblyopia can fluctuate based on factors such as age, ethnicity, race, the specific definition used for amblyopia, the methodology of the study, and other contributing variables.[28][29]
A comprehensive meta-analysis from global prevalence data encompassing more than 1.8 million patients across 60 studies revealed a pooled prevalence rate of 1.44%, with a range of 1.17% to 1.78%. The prevalence rates varied across different continents, with Europe, North America, Asia, and Africa reporting rates of 2.90%, 2.41%, 1.09%, and 0.72%, respectively.[30] The study estimated that in 2019, approximately 99.2 million people worldwide were affected by amblyopia, with a projected increase to 175 million by the year 2030 and 220 million by 2040.[30]
Amblyopia typically manifests as a unilateral condition. However, there are instances where patients can develop the bilateral form if both eyes experience visual alterations during early development.[31] Anisometropia is the most common cause of amblyopia, followed by mixed anisometropia and strabismus, strabismus, and visual deprivation. Studies have indicated that the relative prevalence rates, categorized by the type of amblyopia, are approximately 50% due to anisometropia, 19% linked to strabismus, 27% arising from a combination of both factors, and 4% attributed to deprivation-related causes.[32]
The likelihood of developing amblyopia increases significantly with specific factors. When the difference in refraction error between the eyes falls within the range of 1D to 2D of spherical equivalence, the odds of developing amblyopia are 4.5 times higher. This risk can escalate to a 40-fold increase when the difference in refraction error exceeds 2D.[33]
Regarding strabismus, amblyopia risk has been reported to be between 3 and 18 times greater compared to individuals without strabismus.[34] Mixed and strabismic amblyopia is typically diagnosed at an earlier age, with an average age of 7.4 years, compared to anisometropic amblyopia, which is usually diagnosed at an average age of 12.7.[35] The prevalence of amblyopia appears to be similar between right and left eyes, and there is no observed gender preference.
Several risk factors contribute to the development of amblyopia.[10] These include:[36]
- Ptosis
- Strabismus
- Childhood glaucoma
- Early-onset cataracts (see Image. Pediatric Right Eye Cataract)
- Uveitis
- Systemic conditions with ocular manifestation
- Children born small for gestational age
- Low birth weight (less than 1500 g)
- Premature birth (gestational age less than 30 weeks)
- Developmental delay
- First-degree relatives with the condition
- Maternal use of smoking
- Alcohol or drug use during pregnancy
Pathophysiology
Amblyopia is a neurodevelopmental condition that results in impaired best-corrected vision in one or both eyes.[21] The development of visual acuity in the postnatal period relies on continuous exposure to high-quality visual stimuli by both eyes and the proper functioning of the visual pathways. Research has pinpointed a sensitive or critical period during which amblyopia can develop due to incomplete visual pathway development, with a susceptibility window extending to approximately 7 to 10 years of age.[37] Any deviations from normal vision during the first decade of life caused by unilateral or bilateral blurred retinal images can lead to permanent vision loss if not promptly diagnosed and treated.[38]
Disruptions along the normal visual pathways can arise from various factors, including anisometropia, uncorrected refractive errors, strabismus, and ocular media opacities.[39] Early recognition and intervention are crucial in addressing these underlying causes to prevent the potentially irreversible consequences of amblyopia.
In cases of monocular visual deprivation during the critical period of visual development, a competitive process unfolds between the neural networks of both eyes that are vying for influence over cortical neurons in the primary visual cortex. Various aspects of neuronal selectivity, such as synaptic plasticity, activity dependence, and neuronal network learning, exhibit distinct sensitive periods and are consequently affected in diverse ways by the types of vision deprivation experienced.
Research conducted using functional magnetic resonance imaging (fMRI) and optical coherence tomography (OCT) in individuals with amblyopia have revealed neuroanatomical structural and functional alterations in the gray matter volume of the corresponding visual cortex hemispheres,[40] alteration in cortical thickness within several white matter volumes,[41] variations in ciliary muscle thickness,[42] changes in choroidal thickness,[43] differences in retinal nerve fiber thickness,[44] variations in central macular thickness,[45] and modifications in other structures along the visual pathway.[46] These findings highlight the extensive impact of amblyopia on both the structural and functional aspects of the visual system.
Amblyopia is influenced by the anatomical relationships between photoreceptors and ganglion cell receptor fields, the relationships between ganglion cell receptor fields and the layers within the lateral geniculate, and the connections between the lateral geniculate and the layers of the visual cortex. These intricate neural connections play a pivotal role in developing and manifesting amblyopia.
The depth and severity of amblyopia are closely tied to the age at which it begins and its untreated duration. In general, the earlier the onset of amblyopia and the longer it persists without intervention, the more challenging it becomes to correct and mitigate its effects.[47]
History and Physical
A comprehensive medical history of the patient should be diligently explored, tracing back to their childhood. Whenever feasible, it is valuable to obtain relevant medical records. Some patients may not have a complete recollection of their medical history. In such cases, gathering information from their parents or other family members who may know the patient's eye-related history can be beneficial. It is essential to inquire about specific details, which may include:[7]
- Age and demographics
- Ethnicity and race
- Birth history (birth weight, gestational age, pre and perinatal history, maternal alcohol or drug use during pregnancy)
- Onset of decreased vision
- Refractive correction history
- Ocular trauma
- Ocular pathology
- Amblyopia treatment
- Ocular surgeries
- Systemic conditions
- Medications
- Family history of ocular disease
Any patient with suspected amblyopia should undergo a comprehensive eye examination. The visual acuity of each eye should be assessed individually while considering the patient's refractive correction. Visual acuity in amblyopic eyes may be overestimated when using individual visual targets. It can be advantageous to employ bracketing of visual targets to ensure accuracy.[48] Steroacuity testing should be conducted, as amblyopic eyes frequently exhibit impaired or absent stereopsis.[49]
All patients experiencing decreased vision should undergo a refraction assessment. In the case of children, this evaluation is often best performed after administering cycloplegia to obtain a cycloplegic refraction, which can uncover underlying hyperopia.[50]
Additionally, it is crucial to test the pupillary reflex using light and closely assess the eye in question for any signs of relative afferent pupillary defect, which can be accomplished through the swinging flashlight test.[51] The intraocular pressure (IOP) should be measured in all cooperating patients. However, in situations where patients, especially children, may have difficulty undergoing this testing, it may be deferred.[52]
Extraocular motility and confrontational visual fields should be assessed in all patients capable of undergoing this testing. To identify any underlying strabismus, a frequent cause of amblyopia, it is essential to evaluate for tropias and phorias using the cover-uncover and alternate-cover tests (see Image. Partially Accomodative Estopia).[53]
All patients with suspected amblyopia should undergo a dilated eye examination. During the examination of the eyes, it is crucial to focus on the ocular structures that play a key role in vision, including the cornea, lens, retina, and optic nerve (see Image. Cataractous Changes Seen with Slit Lamp).
In summary, a comprehensive ocular eye examination should encompass the following:[10]
Evaluation
When evaluating for amblyopia, additional testing may be necessary, including formal visual field testing, OCT, fundus photography, and an electroretinogram (ERG).[62] Brain and orbit imaging can be considered if there is suspicion of a compressive lesion along the visual pathway.[63]
Amblyopia is a clinical diagnosis. Thus, additional patient testing should be done only to evaluate for other ocular pathologies causing decreased vision. While research has shown reduced visual cortex size in patients with amblyopia using brain MRI,[64][65] routine brain MRI is not recommended as a standard diagnostic test for amblyopia.
Screening for Amblyopia
Amblyopia holds significant global prevalence and is the leading cause of unilateral visual loss in children.[66] Early detection and timely treatment of this condition can prevent or decrease the severity of permanent visual impairments. Consequently, screening programs for amblyopia are frequently integrated into the public healthcare systems of many nations worldwide.
Guidelines and methods of screening children for amblyopia vary worldwide and even within countries due to social, political, and economic influences.[67] Multiple national guidelines for amblyopia screening have been established, including the following:
- In Canada, certain provinces have implemented amblyopia screening programs for children aged 3 to 5 years, while others, like Ontario and Quebec, do not endorse these national programs.[68]
- In the United States, most states do not have official screening programs for children, despite recommendations by various American Medical Associations.[69] However, in some states, vision screening tests are mandatory for school-age children, typically from kindergarten to grade 12.[70]
- Recent guidelines in France recommend ophthalmologic assessments in the first year of life for children with risk factors for amblyopia. A systematic orthoptic examination, which includes nonmydriatic refraction, BCVA, and oculomotor testing, is recommended at 3 years of age with referral to an ophthalmologist in cases of suspected amblyopia.[71]
- The National Screening Committee in the United Kingdom recommends orthoptist screening assessments for children aged 4 to 5 years.[72]
- In Singapore, children aged 4 to 5 years attending kindergarten undergo their initial vision screening, which continues annually until age 14.[73] Children with suspected amblyopia or those requiring spectacle correction are referred to ophthalmologists.
- South Korea has integrated nationwide toddler and infant screening programs into its national healthcare programs since 2008.[74]
Treatment / Management
The initial treatment approach for amblyopia depends upon the underlying cause. The primary treatment considerations are as follows:
- Deprivation amblyopia: In cases of deprivation amblyopia, the first step involves addressing and rectifying the obstructive pathology responsible for the deprivation. This may encompass surgical interventions such as cataract surgery, retinal detachment repair, corneal surgery, or treatment for various other ocular pathologies.
- Refractive amblyopia: Refractive amblyopia often responds well to treatment. An essential intervention involves addressing the patient's complete refractive error through corrective lenses. In many instances, this may be sufficient to reverse the amblyopia.
- Strabismic amblyopia: For strabismic amblyopia, repairing the strabismus through interventions to realign the eyes is a consideration. However, strabismus repair alone rarely leads to a complete reversal of amblyopia.
The rationale for treating amblyopia is limiting the risk of permanent visual loss during early development.[5] Treatment is generally more effective and sometimes complete when the diagnosis and therapeutic measures start as early as possible during childhood.[75] Timely treatment can have numerous benefits during early development and adulthood, including improvements in BCVA, binocular vision, oculomotor deficits, stereopsis, fixation, contrast sensitivity, and quality of life.[21]
In treating various forms of amblyopia, visual penalization of the eye without amblyopia is often necessary to stimulate visual development in the amblyopic eye. The most common visual penalization method is patching the nonamblyopic eye (see Image. Patching Right Eye). The duration of patching can vary depending on the severity of the amblyopia, with practitioners recommending patching for 2 hours, 6 hours, or even full-time in some cases.[76] Encouraging visual activities such as reading, watching television, or playing video games during patching can be beneficial, as it compels the patient to use the amblyopic eye and may enhance the patient's cooperation with the patching regimen, significantly if it is associated with enjoyable activities.(B3)
Patching the eye without amblyopia as a treatment has a long history dating back to the 16th century. It continues to be a central component of therapy to this day.[77][78]
In cases where patients cannot reliably adhere to patching therapy, pharmacologic treatment for amblyopia is an option. A cycloplegic drug, typically atropine, can inhibit accommodation in the eye without amblyopia. The treatment offers the advantage of being administered as a single daily drop, which can be more convenient than an eye patch's extended use. Research has indicated that pharmacologic therapy can be similarly effective to patching in suitable patients.[79] However, patients who are myopic or emmetropic in the nonamblyopic eye may not benefit from pharmacologic therapy, as their eyes can already maintain focus on objects at specific distances without the need for accommodation. (A1)
As a patient ages, the likelihood of successfully reversing amblyopia through brain plasticity diminishes. The precise age at which amblyopia treatment becomes ineffective is not uniformly established. Nevertheless, The Pediatric Eye Disease Investigator Group has indicated that patients aged 7 to 12 showed some degree of benefit from amblyopia treatment. In contrast, patients 13 and older typically exhibit minimal improvement with treatment.[80](B3)
Treatment Options for Amblyopia
Treatment options for amblyopia, which can be used individually or in combination, encompass:
- Optical correction [7]
- Patching [81]
- Pharmacological treatment (eg, Atropine 1%) [82]
- Optical treatment for refractive blur (not typically used) [83]
- Bangerter filters [84]
- Binocular Dichoptic Therapy [85][86]
- Surgery (for conditions like media opacities, strabismus, refractive errors) [87][88]
- Alternative therapies (such as oculomotor exercises and polarized glasses) [89][90]
- Emerging treatment (including perceptual training,[91] video games,[92] brain stimulation [93]) (A1)
Follow-up evaluations are crucial to gauge the effectiveness of therapy and to make any modifications and adjustments to the treatment plan. The primary objective is to enhance BCVA in the amblyopic eye. Additionally, the fellow healthy eye should be evaluated to prevent the development of reverse amblyopia in the occluded eye and to ensure that refractive correction is updated for spectacle use.
During follow-up assessments, the healthcare professional should also assess the patient's adherence to the treatment regimen, monitor for side effects of treatments, watch for any signs of amblyopia recurrence upon discontinuation of therapy, and consider modifications to the treatment plan if it is found to be ineffective or unsuitable for the individual patient.[39][94] These ongoing evaluations are crucial for optimizing the outcomes of amblyopia treatment.
Differential Diagnosis
Amblyopia is a diagnosis of exclusion, meaning that amblyopia can be diagnosed only after all other potential ocular or cerebral pathologies have been eliminated as the causes of decreased visual acuity. Common factors contributing to decreased visual acuity include refractive errors, cataracts, corneal abnormalities, retinal pathologies, and optic nerve disorders. Most of these pathologies can be ruled out by a comprehensive eye examination. It is also essential to consider the possibility of cerebral visual impairment and functional (non-organic) vision loss.[95]
While routine diagnostic tests such as OCT, visual field testing, and MRI are not typically conducted in clinical settings, they may be considered in uncertain situations or when there is a need to exclude potential underlying causes of impaired vision.
Prognosis
The prognosis of amblyopia depends on the age at which treatment is initiated and the severity of the condition. Amblyopia carries significant morbidity and is a common cause of monocular vision impairment. At least 75% of children who undergo occlusion therapy exhibit a favorable improvement in vision. However, visual acuity may slightly decline over time in approximately 50% of children with amblyopia. The most promising outcomes are observed in children referred for treatment early in life. Nonetheless, as children grow, the actual real-life images they encounter may undergo slight alterations.[96][97]
When treated, over 70% of patients experience significant vision improvement within 12 months. Even after successful treatment, there may be some gradual decline in vision in subsequent years. Factors associated with a heightened risk of not achieving complete vision restoration include the age at which treatment commenced (with later treatment typically yielding a less favorable outcome), deprivation amblyopia, and poor initial visual acuity.
Complications
The primary complication of amblyopia is an irreversible, lifelong reduction in vision. These visual functional abnormalities include diminished BCVA, reduced contrast sensitivity, impaired vernier acuity, spatial distortion, abnormal spatial interactions, and compromised contour detection. Individuals with amblyopia typically exhibit binocular abnormalities, including poor stereoscopic acuity and abnormal binocular summation. While the monocular vision deficits are usually specific to the amblyopic eye, there have been instances of subclinical deficits observed in the nonamblyopic eye.
Individuals with amblyopia often encounter challenges when perceiving 3-dimensional images hidden in stereoscopic displays such as autostereograms. However, their perception of depth derived from monocular cues, such as variations in size, perspective, and motion parallax in the nonamblyopic eye, typically remains normal.
Children with amblyopia may experience impaired learning abilities and are found to read and respond to multiple-choice questions at a slower pace than children without amblyopia.[98][99] Another potential complication associated with amblyopia is the worsening of strabismus, which can occur due to impaired binocular fusion.
Deterrence and Patient Education
Parents should receive comprehensive education regarding the importance of early vision examinations for their children. School vision screenings may serve as the first time amblyopia is suspected. If a child is diagnosed with amblyopia, parents must comprehend that, without treatment, the vision loss associated with amblyopia is typically irreversible. The importance of therapy should be emphasized to the child and parents.
Children may initially resist wearing glasses or patches, but parents must ensure that their child adheres to the treatment plan. Healthcare professionals should consistently encourage and support parents during every visit to ensure the continuation of treatment, as amblyopia treatment may need to be sustained over an extended period.
Enhancing Healthcare Team Outcomes
Pediatric ophthalmologists primarily treat amblyopia, although optometrists also possess the expertise in its management. It is critically important that patients are referred to a healthcare professional who has training in amblyopia treatment, as mismanagement of this condition can lead to irreversible vision loss.
The initial healthcare professional to suspect amblyopia often will not be an ophthalmologist or optometrist. Pediatricians, family doctors, nurses, or medical assistants usually have concerns about amblyopia and will refer the patient to an appropriate specialist.
Family members who spend significant time with the patient may be the first to notice preferential fixation of the nonamblyopic eye. Vision screenings often play a fundamental role in the early diagnosis of amblyopia.[100] Without a proper referral, the child is at risk for permanent vision loss. As the duration of the condition's undiagnosed and untreated state lengthens, the prognosis becomes increasingly unfavorable. Effective communication between healthcare providers and, importantly, with parents is essential to prevent irreversible vision loss stemming from this condition.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)

Bilateral Exotropia. (a) Image of the child depicting a 30° exotropia in the left eye while fixating with the right eye in primary gaze. (b) Image of the child showing a 30° exotropia with minimal 5° hypertropia of the right eye while fixating with the left eye in primary gaze suggestive of an alternate exotropia with right eye dissociated vertical deviation
Contributed by Dr. Kirandeep Kaur, MBBS, DNB, FPOS, FICO, MRCS Ed, MNAMS
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)

Congenital Ptosis. Right congenital ptosis with moderate levator function. A right anterior approach levator advancement procedure was done to correct the ptosis and create a new skin crease. Examining all children with unilateral ptosis for amblyopia in the affected eye is essential and institute eye-patching as indicated.
Contributed by Prof. Bhupendra C. K. Patel MD, FRCS
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Levi DM. Amblyopia. Handbook of clinical neurology. 2021:178():13-30. doi: 10.1016/B978-0-12-821377-3.00002-7. Epub [PubMed PMID: 33832673]
Birch EE, Subramanian V, Weakley DR. Fixation instability in anisometropic children with reduced stereopsis. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2013 Jun:17(3):287-90. doi: 10.1016/j.jaapos.2013.03.011. Epub [PubMed PMID: 23791411]
Level 2 (mid-level) evidenceWebber AL. The functional impact of amblyopia. Clinical & experimental optometry. 2018 Jul:101(4):443-450. doi: 10.1111/cxo.12663. Epub 2018 Feb 26 [PubMed PMID: 29484704]
Seignette K, Levelt CN. Amblyopia: The Thalamus Is a No-Go Area for Visual Acuity. Current biology : CB. 2018 Jun 18:28(12):R709-R712. doi: 10.1016/j.cub.2018.04.081. Epub [PubMed PMID: 29920266]
Hunter D, Cotter S. Early diagnosis of amblyopia. Visual neuroscience. 2018 Jan:35():E013. doi: 10.1017/S0952523817000207. Epub [PubMed PMID: 29905128]
Bangerter A. Treatment of amblyopia: Part 3 Apparatus, exercise equipment and games (continued). Strabismus. 2018 Jun:26(2):106-109. doi: 10.1080/09273972.2018.1463676. Epub [PubMed PMID: 29952715]
Cruz OA, Repka MX, Hercinovic A, Cotter SA, Lambert SR, Hutchinson AK, Sprunger DT, Morse CL, Wallace DK, American Academy of Ophthalmology Preferred Practice Pattern Pediatric Ophthalmology/Strabismus Panel. Amblyopia Preferred Practice Pattern. Ophthalmology. 2023 Mar:130(3):P136-P178. doi: 10.1016/j.ophtha.2022.11.003. Epub 2022 Dec 14 [PubMed PMID: 36526450]
Repka MX. Amblyopia Outcomes Through Clinical Trials and Practice Measurement: Room for Improvement: The LXXVII Edward Jackson Memorial Lecture. American journal of ophthalmology. 2020 Nov:219():A1-A26. doi: 10.1016/j.ajo.2020.07.053. Epub 2020 Aug 7 [PubMed PMID: 32777377]
Hamm L, Chen Z, Li J, Black J, Dai S, Yuan J, Yu M, Thompson B. Interocular suppression in children with deprivation amblyopia. Vision research. 2017 Apr:133():112-120. doi: 10.1016/j.visres.2017.01.004. Epub 2017 Mar 30 [PubMed PMID: 28214552]
Sen S, Singh P, Saxena R. Management of amblyopia in pediatric patients: Current insights. Eye (London, England). 2022 Jan:36(1):44-56. doi: 10.1038/s41433-021-01669-w. Epub 2021 Jul 7 [PubMed PMID: 34234293]
Pascual M, Huang J, Maguire MG, Kulp MT, Quinn GE, Ciner E, Cyert LA, Orel-Bixler D, Moore B, Ying GS, Vision In Preschoolers (VIP) Study Group. Risk factors for amblyopia in the vision in preschoolers study. Ophthalmology. 2014 Mar:121(3):622-9.e1. doi: 10.1016/j.ophtha.2013.08.040. Epub 2013 Oct 18 [PubMed PMID: 24140117]
Level 2 (mid-level) evidenceNajem K, Margolin E. Diplopia. StatPearls. 2024 Jan:(): [PubMed PMID: 28722934]
Şahin Karamert S, Atalay HT, Özdek Ş. Strabismus in Retinopathy of Prematurity: Risk Factors and the Effect of Macular Ectopia. Turkish journal of ophthalmology. 2023 Aug 19:53(4):241-246. doi: 10.4274/tjo.galenos.2023.48310. Epub [PubMed PMID: 37602650]
Hamm LM, Chen Z, Li J, Dai S, Black J, Yuan J, Yu M, Thompson B. Contrast-balanced binocular treatment in children with deprivation amblyopia. Clinical & experimental optometry. 2018 Jul:101(4):541-552. doi: 10.1111/cxo.12630. Epub 2017 Nov 28 [PubMed PMID: 29193320]
Cheng KP, Hiles DA, Biglan AW, Pettapiece MC. Visual results after early surgical treatment of unilateral congenital cataracts. Ophthalmology. 1991 Jun:98(6):903-10 [PubMed PMID: 1866144]
Elhusseiny AM, Wu C, MacKinnon S, Hunter DG. Severe reverse amblyopia with atropine penalization. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2020 Apr:24(2):106-108. doi: 10.1016/j.jaapos.2019.12.001. Epub 2020 Jan 15 [PubMed PMID: 31953022]
Pediatric Eye Disease Investigator Group.. A randomized trial of atropine vs. patching for treatment of moderate amblyopia in children. Archives of ophthalmology (Chicago, Ill. : 1960). 2002 Mar:120(3):268-78 [PubMed PMID: 11879129]
Level 1 (high-level) evidencede Zárate BR, Tejedor J. Current concepts in the management of amblyopia. Clinical ophthalmology (Auckland, N.Z.). 2007 Dec:1(4):403-14 [PubMed PMID: 19668517]
Holmes JM, Levi DM. Treatment of amblyopia as a function of age. Visual neuroscience. 2018 Jan:35():E015. doi: 10.1017/S0952523817000220. Epub [PubMed PMID: 29905125]
Kiorpes L, Daw N. Cortical correlates of amblyopia. Visual neuroscience. 2018 Jan:35():E016. doi: 10.1017/S0952523817000232. Epub [PubMed PMID: 29905122]
Levi DM. Rethinking amblyopia 2020. Vision research. 2020 Nov:176():118-129. doi: 10.1016/j.visres.2020.07.014. Epub 2020 Aug 28 [PubMed PMID: 32866759]
Davidson S, Quinn GE. The impact of pediatric vision disorders in adulthood. Pediatrics. 2011 Feb:127(2):334-9. doi: 10.1542/peds.2010-1911. Epub 2011 Jan 3 [PubMed PMID: 21199855]
Webber AL, Wood J. Amblyopia: prevalence, natural history, functional effects and treatment. Clinical & experimental optometry. 2005 Nov:88(6):365-75 [PubMed PMID: 16329744]
Hu B, Liu Z, Zhao J, Zeng L, Hao G, Shui D, Mao K. The Global Prevalence of Amblyopia in Children: A Systematic Review and Meta-Analysis. Frontiers in pediatrics. 2022:10():819998. doi: 10.3389/fped.2022.819998. Epub 2022 May 4 [PubMed PMID: 35601430]
Level 1 (high-level) evidenceHashemi H, Pakzad R MSc, Yekta A, Bostamzad P, Aghamirsalim M, Sardari S MSc, Valadkhan M MSc, Pakbin M MSc, Heydarian S, Khabazkhoob M. Global and regional estimates of prevalence of amblyopia: A systematic review and meta-analysis. Strabismus. 2018 Dec:26(4):168-183. doi: 10.1080/09273972.2018.1500618. Epub 2018 Jul 30 [PubMed PMID: 30059649]
Level 1 (high-level) evidenceNitzan I, Bez M, Megreli J, Bez D, Barak A, Yahalom C, Levine H. Socio-demographic disparities in amblyopia prevalence among 1.5 million adolescents. European journal of public health. 2021 Dec 1:31(6):1211-1217. doi: 10.1093/eurpub/ckab111. Epub [PubMed PMID: 34518882]
Xiao O, Morgan IG, Ellwein LB, He M, Refractive Error Study in Children Study Group. Prevalence of Amblyopia in School-Aged Children and Variations by Age, Gender, and Ethnicity in a Multi-Country Refractive Error Study. Ophthalmology. 2015 Sep:122(9):1924-31. doi: 10.1016/j.ophtha.2015.05.034. Epub 2015 Aug 13 [PubMed PMID: 26278861]
Aldebasi YH. Prevalence of amblyopia in primary school children in Qassim province, Kingdom of Saudi Arabia. Middle East African journal of ophthalmology. 2015 Jan-Mar:22(1):86-91. doi: 10.4103/0974-9233.148355. Epub [PubMed PMID: 25624680]
Level 2 (mid-level) evidenceFu J, Li SM, Liu LR, Li JL, Li SY, Zhu BD, Li H, Yang Z, Li L, Wang NL, Anyang Childhood Eye Study Group. Prevalence of amblyopia and strabismus in a population of 7th-grade junior high school students in Central China: the Anyang Childhood Eye Study (ACES). Ophthalmic epidemiology. 2014 Jun:21(3):197-203. doi: 10.3109/09286586.2014.904371. Epub 2014 Apr 17 [PubMed PMID: 24742059]
Level 2 (mid-level) evidenceFu Z, Hong H, Su Z, Lou B, Pan CW, Liu H. Global prevalence of amblyopia and disease burden projections through 2040: a systematic review and meta-analysis. The British journal of ophthalmology. 2020 Aug:104(8):1164-1170. doi: 10.1136/bjophthalmol-2019-314759. Epub 2019 Nov 8 [PubMed PMID: 31704700]
Level 1 (high-level) evidenceChia A, Lin X, Dirani M, Gazzard G, Ramamurthy D, Quah BL, Chang B, Ling Y, Leo SW, Wong TY, Saw SM. Risk factors for strabismus and amblyopia in young Singapore Chinese children. Ophthalmic epidemiology. 2013 Jun:20(3):138-47. doi: 10.3109/09286586.2013.767354. Epub [PubMed PMID: 23713916]
Level 2 (mid-level) evidenceXu Z, Wu Z, Wen Y, Ding M, Sun W, Wang Y, Shao Z, Liu Y, Yu M, Liu G, Hu Y, Bi H. Prevalence of anisometropia and associated factors in Shandong school-aged children. Frontiers in public health. 2022:10():1072574. doi: 10.3389/fpubh.2022.1072574. Epub 2022 Dec 22 [PubMed PMID: 36620276]
Tarczy-Hornoch K, Varma R, Cotter SA, McKean-Cowdin R, Lin JH, Borchert MS, Torres M, Wen G, Azen SP, Tielsch JM, Friedman DS, Repka MX, Katz J, Ibironke J, Giordano L, Joint Writing Committee for the Multi-Ethnic Pediatric Eye Disease Study and the Baltimore Pediatric Eye Disease Study Groups. Risk factors for decreased visual acuity in preschool children: the multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology. 2011 Nov:118(11):2262-73. doi: 10.1016/j.ophtha.2011.06.033. Epub 2011 Aug 19 [PubMed PMID: 21856014]
Level 2 (mid-level) evidenceAfsari S, Rose KA, Gole GA, Philip K, Leone JF, French A, Mitchell P. Prevalence of anisometropia and its association with refractive error and amblyopia in preschool children. The British journal of ophthalmology. 2013 Sep:97(9):1095-9. doi: 10.1136/bjophthalmol-2012-302637. Epub 2013 Apr 23 [PubMed PMID: 23613508]
Attebo K, Mitchell P, Cumming R, Smith W, Jolly N, Sparkes R. Prevalence and causes of amblyopia in an adult population. Ophthalmology. 1998 Jan:105(1):154-9 [PubMed PMID: 9442792]
Pathai S, Cumberland PM, Rahi JS. Prevalence of and early-life influences on childhood strabismus: findings from the Millennium Cohort Study. Archives of pediatrics & adolescent medicine. 2010 Mar:164(3):250-7. doi: 10.1001/archpediatrics.2009.297. Epub [PubMed PMID: 20194258]
Level 2 (mid-level) evidenceDuan Y, Norcia AM, Yeatman JD, Mezer A. The Structural Properties of Major White Matter Tracts in Strabismic Amblyopia. Investigative ophthalmology & visual science. 2015 Aug:56(9):5152-60. doi: 10.1167/iovs.15-17097. Epub [PubMed PMID: 26241402]
Varma R, Tarczy-Hornoch K, Jiang X. Visual Impairment in Preschool Children in the United States: Demographic and Geographic Variations From 2015 to 2060. JAMA ophthalmology. 2017 Jun 1:135(6):610-616. doi: 10.1001/jamaophthalmol.2017.1021. Epub [PubMed PMID: 28472231]
Lin HW, Young ML, Pu C, Huang CY, Lin KK, Lee JS, Hou CH. Changes in anisometropia by age in children with hyperopia, myopia, and antimetropia. Scientific reports. 2023 Aug 22:13(1):13643. doi: 10.1038/s41598-023-40831-0. Epub 2023 Aug 22 [PubMed PMID: 37608064]
Mendola JD, Lam J, Rosenstein M, Lewis LB, Shmuel A. Partial correlation analysis reveals abnormal retinotopically organized functional connectivity of visual areas in amblyopia. NeuroImage. Clinical. 2018:18():192-201. doi: 10.1016/j.nicl.2018.01.022. Epub 2018 Jan 31 [PubMed PMID: 29868445]
Kantarci FA, Tatar MG, Uslu H, Colak HN, Yildirim A, Goker H, Gurler B. Choroidal and peripapillary retinal nerve fiber layer thickness in adults with anisometropic amblyopia. European journal of ophthalmology. 2015 Sep-Oct:25(5):437-42. doi: 10.5301/ejo.5000594. Epub 2015 Mar 21 [PubMed PMID: 25837640]
Cevher S, Şahin T. Does anisometropia affect the ciliary muscle thickness? An ultrasound biomicroscopy study. International ophthalmology. 2020 Dec:40(12):3393-3402. doi: 10.1007/s10792-020-01625-9. Epub 2020 Oct 20 [PubMed PMID: 33083933]
Nishi T, Ueda T, Hasegawa T, Miyata K, Ogata N. Choroidal thickness in children with hyperopic anisometropic amblyopia. The British journal of ophthalmology. 2014 Feb:98(2):228-32. doi: 10.1136/bjophthalmol-2013-303938. Epub 2013 Nov 1 [PubMed PMID: 24187049]
Level 2 (mid-level) evidenceTekin K, Cankurtaran V, Inanc M, Sekeroglu MA, Yilmazbas P. Effect of myopic anisometropia on anterior and posterior ocular segment parameters. International ophthalmology. 2017 Apr:37(2):377-384. doi: 10.1007/s10792-016-0272-x. Epub 2016 Jun 4 [PubMed PMID: 27262559]
Bruce A, Pacey IE, Bradbury JA, Scally AJ, Barrett BT. Bilateral changes in foveal structure in individuals with amblyopia. Ophthalmology. 2013 Feb:120(2):395-403. doi: 10.1016/j.ophtha.2012.07.088. Epub 2012 Sep 29 [PubMed PMID: 23031668]
Level 2 (mid-level) evidenceMeng C, Zhang Y, Wang S. Anisometropic amblyopia: A review of functional and structural changes and treatment. European journal of ophthalmology. 2023 Jul:33(4):1529-1535. doi: 10.1177/11206721221143164. Epub 2022 Nov 29 [PubMed PMID: 36448184]
Jang J, Kyung SE. Assessing amblyopia treatment using multifocal visual evoked potentials. BMC ophthalmology. 2018 Aug 13:18(1):196. doi: 10.1186/s12886-018-0877-0. Epub 2018 Aug 13 [PubMed PMID: 30103718]
Caltrider D, Gupta A, Tripathy K. Evaluation of Visual Acuity. StatPearls. 2025 Jan:(): [PubMed PMID: 33231977]
Adams WE, Leske DA, Hatt SR, Holmes JM. Defining real change in measures of stereoacuity. Ophthalmology. 2009 Feb:116(2):281-5. doi: 10.1016/j.ophtha.2008.09.012. Epub 2008 Dec 16 [PubMed PMID: 19091410]
Level 2 (mid-level) evidenceMajumdar S, Tripathy K. Hyperopia. StatPearls. 2023 Jan:(): [PubMed PMID: 32809551]
Simakurthy S, Tripathy K. Marcus Gunn Pupil. StatPearls. 2025 Jan:(): [PubMed PMID: 32491607]
Bader J, Zeppieri M, Havens SJ. Tonometry. StatPearls. 2024 Jan:(): [PubMed PMID: 29630277]
Kanukollu VM, Sood G. Strabismus. StatPearls. 2024 Jan:(): [PubMed PMID: 32809617]
Lança CC, Rowe FJ. Measurement of fusional vergence: a systematic review. Strabismus. 2019 Jun:27(2):88-113. doi: 10.1080/09273972.2019.1583675. Epub 2019 Mar 1 [PubMed PMID: 30821611]
Level 1 (high-level) evidenceHutchinson AK, Morse CL, Hercinovic A, Cruz OA, Sprunger DT, Repka MX, Lambert SR, Wallace DK, American Academy of Ophthalmology Preferred Practice Pattern Pediatric Ophthalmology/Strabismus Panel. Pediatric Eye Evaluations Preferred Practice Pattern. Ophthalmology. 2023 Mar:130(3):P222-P270. doi: 10.1016/j.ophtha.2022.10.030. Epub 2022 Dec 19 [PubMed PMID: 36543602]
Cotter SA, Tarczy-Hornoch K, Song E, Lin J, Borchert M, Azen SP, Varma R, Multi-Ethnic Pediatric Eye Disease Study Group. Fixation preference and visual acuity testing in a population-based cohort of preschool children with amblyopia risk factors. Ophthalmology. 2009 Jan:116(1):145-53. doi: 10.1016/j.ophtha.2008.08.031. Epub 2008 Oct 29 [PubMed PMID: 18962921]
Donahue SP, Baker CN, Committee on Practice and Ambulatory Medicine, American Academy of Pediatrics, Section on Ophthalmology, American Academy of Pediatrics, American Association of Certified Orthoptists, American Association for Pediatric Ophthalmology and Strabismus, American Academy of Ophthalmology. Procedures for the Evaluation of the Visual System by Pediatricians. Pediatrics. 2016 Jan:137(1):. doi: 10.1542/peds.2015-3597. Epub 2015 Dec 7 [PubMed PMID: 26644488]
Aljohani S, Aldakhil S, Alrasheed SH, Tan QQ, Alshammeri S. The Clinical Characteristics of Amblyopia in Children Under 17 Years of Age in Qassim Region, Saudi Arabia. Clinical ophthalmology (Auckland, N.Z.). 2022:16():2677-2684. doi: 10.2147/OPTH.S379550. Epub 2022 Aug 18 [PubMed PMID: 36003073]
Tam EK, Elhusseiny AM, Shah AS, Mantagos IS, VanderVeen DK. Etiology and outcomes of childhood glaucoma at a tertiary referral center. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2022 Jun:26(3):117.e1-117.e6. doi: 10.1016/j.jaapos.2021.12.009. Epub 2022 Apr 8 [PubMed PMID: 35398512]
Fan DS, Rao SK, Ng JS, Yu CB, Lam DS. Comparative study on the safety and efficacy of different cycloplegic agents in children with darkly pigmented irides. Clinical & experimental ophthalmology. 2004 Oct:32(5):462-7 [PubMed PMID: 15498055]
Level 1 (high-level) evidenceWang C, Yu J, Pan M, Ye X, Song E. Macular pigment optical density of hyperopic anisometropic amblyopic patients measured by fundus reflectometry. Frontiers in medicine. 2022:9():991423. doi: 10.3389/fmed.2022.991423. Epub 2022 Oct 11 [PubMed PMID: 36304187]
Asanad S, Karanjia R. Full-Field Electroretinogram. StatPearls. 2024 Jan:(): [PubMed PMID: 32491415]
Musa MJ, Zeppieri M. Foster Kennedy Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 35881754]
Xiao JX, Xie S, Ye JT, Liu HH, Gan XL, Gong GL, Jiang XX. Detection of abnormal visual cortex in children with amblyopia by voxel-based morphometry. American journal of ophthalmology. 2007 Mar:143(3):489-93 [PubMed PMID: 17224120]
Choi MY, Lee KM, Hwang JM, Choi DG, Lee DS, Park KH, Yu YS. Comparison between anisometropic and strabismic amblyopia using functional magnetic resonance imaging. The British journal of ophthalmology. 2001 Sep:85(9):1052-6 [PubMed PMID: 11520755]
Bui Quoc E, Kulp MT, Burns JG, Thompson B. Amblyopia: A review of unmet needs, current treatment options, and emerging therapies. Survey of ophthalmology. 2023 May-Jun:68(3):507-525. doi: 10.1016/j.survophthal.2023.01.001. Epub 2023 Jan 18 [PubMed PMID: 36681277]
Level 3 (low-level) evidencePowell C, Hatt SR. Vision screening for amblyopia in childhood. The Cochrane database of systematic reviews. 2009 Jul 8:(3):CD005020. doi: 10.1002/14651858.CD005020.pub3. Epub 2009 Jul 8 [PubMed PMID: 19588363]
Level 1 (high-level) evidenceMema SC, McIntyre L, Musto R. Childhood vision screening in Canada: public health evidence and practice. Canadian journal of public health = Revue canadienne de sante publique. 2012 Jan-Feb:103(1):40-5 [PubMed PMID: 22338327]
Hambidge SJ, Emsermann CB, Federico S, Steiner JF. Disparities in pediatric preventive care in the United States, 1993-2002. Archives of pediatrics & adolescent medicine. 2007 Jan:161(1):30-6 [PubMed PMID: 17199064]
Level 2 (mid-level) evidenceWahl MD, Fishman D, Block SS, Baldonado KN, Friedman DS, Repka MX, Collins ME. A Comprehensive Review of State Vision Screening Mandates for Schoolchildren in the United States. Optometry and vision science : official publication of the American Academy of Optometry. 2021 May 1:98(5):490-499. doi: 10.1097/OPX.0000000000001686. Epub [PubMed PMID: 33973910]
Lequeux L, Thouvenin D, Couret C, Audren F, Costet C, Dureau P, Leruez S, Defoordt-Dhellemmes S, Daien V, Espinasse Berrod MA, Arsene S, Lebranchu P, Denis D, Bui-Quoc E, Speeg-Schatz C. [Vision screening for children: Recommended practices from AFSOP]. Journal francais d'ophtalmologie. 2021 Feb:44(2):244-251. doi: 10.1016/j.jfo.2020.07.005. Epub 2020 Dec 30 [PubMed PMID: 33388188]
Tailor V, Bossi M, Greenwood JA, Dahlmann-Noor A. Childhood amblyopia: current management and new trends. British medical bulletin. 2016 Sep:119(1):75-86. doi: 10.1093/bmb/ldw030. Epub 2016 Aug 19 [PubMed PMID: 27543498]
Handa S, Chia A. Amblyopia therapy in Asian children: factors affecting visual outcome and parents' perception of children's attitudes towards amblyopia treatment. Singapore medical journal. 2019 Jun:60(6):291-297. doi: 10.11622/smedj.2018151. Epub 2018 Nov 29 [PubMed PMID: 30488078]
Jeong SH, Kim US. Ten-Year Results of Home Vision-Screening Test in Children Aged 3-6 Years in Seoul, Korea. Seminars in ophthalmology. 2015:30(5-6):383-8. doi: 10.3109/08820538.2014.912335. Epub 2014 May 8 [PubMed PMID: 24809740]
Hunter D. Amblyopia: The clinician's view. Visual neuroscience. 2018 Jan:35():E011. doi: 10.1017/S0952523817000189. Epub [PubMed PMID: 29905115]
Chen AM, Cotter SA. The Amblyopia Treatment Studies: Implications for Clinical Practice. Advances in ophthalmology and optometry. 2016 Aug:1(1):287-305. doi: 10.1016/j.yaoo.2016.03.007. Epub [PubMed PMID: 28435934]
Level 3 (low-level) evidencePeterseim MMW, Rhodes RS, Patel RN, Wilson ME, Edmondson LE, Logan SA, Cheeseman EW, Shortridge E, Trivedi RH. Effectiveness of the GoCheck Kids Vision Screener in Detecting Amblyopia Risk Factors. American journal of ophthalmology. 2018 Mar:187():87-91. doi: 10.1016/j.ajo.2017.12.020. Epub 2018 Jan 2 [PubMed PMID: 29305313]
US Preventive Services Task Force, Grossman DC, Curry SJ, Owens DK, Barry MJ, Davidson KW, Doubeni CA, Epling JW Jr, Kemper AR, Krist AH, Kurth AE, Landefeld CS, Mangione CM, Phipps MG, Silverstein M, Simon MA, Tseng CW. Vision Screening in Children Aged 6 Months to 5 Years: US Preventive Services Task Force Recommendation Statement. JAMA. 2017 Sep 5:318(9):836-844. doi: 10.1001/jama.2017.11260. Epub [PubMed PMID: 28873168]
Scheiman MM, Hertle RW, Kraker RT, Beck RW, Birch EE, Felius J, Holmes JM, Kundart J, Morrison DG, Repka MX, Tamkins SM, Pediatric Eye Disease Investigator Group. Patching vs atropine to treat amblyopia in children aged 7 to 12 years: a randomized trial. Archives of ophthalmology (Chicago, Ill. : 1960). 2008 Dec:126(12):1634-42. doi: 10.1001/archophthalmol.2008.107. Epub [PubMed PMID: 19064841]
Level 1 (high-level) evidenceScheiman MM, Hertle RW, Beck RW, Edwards AR, Birch E, Cotter SA, Crouch ER Jr, Cruz OA, Davitt BV, Donahue S, Holmes JM, Lyon DW, Repka MX, Sala NA, Silbert DI, Suh DW, Tamkins SM, Pediatric Eye Disease Investigator Group. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Archives of ophthalmology (Chicago, Ill. : 1960). 2005 Apr:123(4):437-47 [PubMed PMID: 15824215]
Level 3 (low-level) evidenceRepka MX, Kraker RT, Holmes JM, Summers AI, Glaser SR, Barnhardt CN, Tien DR, Pediatric Eye Disease Investigator Group. Atropine vs patching for treatment of moderate amblyopia: follow-up at 15 years of age of a randomized clinical trial. JAMA ophthalmology. 2014 Jul:132(7):799-805. doi: 10.1001/jamaophthalmol.2014.392. Epub [PubMed PMID: 24789375]
Level 1 (high-level) evidenceLi Y, Sun H, Zhu X, Su Y, Yu T, Wu X, Zhou X, Jing L. Efficacy of interventions for amblyopia: a systematic review and network meta-analysis. BMC ophthalmology. 2020 May 25:20(1):203. doi: 10.1186/s12886-020-01442-9. Epub 2020 May 25 [PubMed PMID: 32450849]
Level 1 (high-level) evidenceRepka MX, Gallin PF, Scholz RT, Guyton DL. Determination of optical penalization by vectographic fixation reversal. Ophthalmology. 1985 Nov:92(11):1584-6 [PubMed PMID: 4080330]
Pediatric Eye Disease Investigator Group Writing Committee, Rutstein RP, Quinn GE, Lazar EL, Beck RW, Bonsall DJ, Cotter SA, Crouch ER, Holmes JM, Hoover DL, Leske DA, Lorenzana IJ, Repka MX, Suh DW. A randomized trial comparing Bangerter filters and patching for the treatment of moderate amblyopia in children. Ophthalmology. 2010 May:117(5):998-1004.e6. doi: 10.1016/j.ophtha.2009.10.014. Epub 2010 Feb 16 [PubMed PMID: 20163869]
Level 1 (high-level) evidenceLi SL, Reynaud A, Hess RF, Wang YZ, Jost RM, Morale SE, De La Cruz A, Dao L, Stager D Jr, Birch EE. Dichoptic movie viewing treats childhood amblyopia. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2015 Oct:19(5):401-5. doi: 10.1016/j.jaapos.2015.08.003. Epub [PubMed PMID: 26486019]
Xiao S, Angjeli E, Wu HC, Gaier ED, Gomez S, Travers DA, Binenbaum G, Langer R, Hunter DG, Repka MX, Luminopia Pivotal Trial Group. Randomized Controlled Trial of a Dichoptic Digital Therapeutic for Amblyopia. Ophthalmology. 2022 Jan:129(1):77-85. doi: 10.1016/j.ophtha.2021.09.001. Epub 2021 Sep 14 [PubMed PMID: 34534556]
Level 1 (high-level) evidenceLam GC, Repka MX, Guyton DL. Timing of amblyopia therapy relative to strabismus surgery. Ophthalmology. 1993 Dec:100(12):1751-6 [PubMed PMID: 8259271]
Ehlers M, Mauschitz MM, Wabbels B. Implementing strabismus-specific psychosocial questionnaires in everyday clinical practice: mental health and quality of life in the context of strabismus surgery. BMJ open ophthalmology. 2023 Aug:8(1):. doi: 10.1136/bmjophth-2023-001334. Epub [PubMed PMID: 37558407]
Level 2 (mid-level) evidenceSuttle CM. Active treatments for amblyopia: a review of the methods and evidence base. Clinical & experimental optometry. 2010 Sep:93(5):287-99. doi: 10.1111/j.1444-0938.2010.00486.x. Epub 2010 Jun 28 [PubMed PMID: 20533925]
Level 3 (low-level) evidenceWang J, Neely DE, Galli J, Schliesser J, Graves A, Damarjian TG, Kovarik J, Bowsher J, Smith HA, Donaldson D, Haider KM, Roberts GJ, Sprunger DT, Plager DA. A pilot randomized clinical trial of intermittent occlusion therapy liquid crystal glasses versus traditional patching for treatment of moderate unilateral amblyopia. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2016 Aug:20(4):326-31. doi: 10.1016/j.jaapos.2016.05.014. Epub 2016 Jul 12 [PubMed PMID: 27418249]
Level 1 (high-level) evidenceChen Z, Li J, Liu J, Cai X, Yuan J, Deng D, Yu M. Monocular perceptual learning of contrast detection facilitates binocular combination in adults with anisometropic amblyopia. Scientific reports. 2016 Feb 1:6():20187. doi: 10.1038/srep20187. Epub 2016 Feb 1 [PubMed PMID: 26829898]
Kelly KR, Jost RM, Dao L, Beauchamp CL, Leffler JN, Birch EE. Binocular iPad Game vs Patching for Treatment of Amblyopia in Children: A Randomized Clinical Trial. JAMA ophthalmology. 2016 Dec 1:134(12):1402-1408. doi: 10.1001/jamaophthalmol.2016.4224. Epub [PubMed PMID: 27832248]
Level 1 (high-level) evidenceDing Z, Li J, Spiegel DP, Chen Z, Chan L, Luo G, Yuan J, Deng D, Yu M, Thompson B. The effect of transcranial direct current stimulation on contrast sensitivity and visual evoked potential amplitude in adults with amblyopia. Scientific reports. 2016 Jan 14:6():19280. doi: 10.1038/srep19280. Epub 2016 Jan 14 [PubMed PMID: 26763954]
Zhang H, Yang P, Li Y, Zhang W, Li S. Effect of Low-Concentration Atropine Eye Drops in Controlling the Progression of Myopia in Children: A One- and Two-Year Follow-Up Study. Ophthalmic epidemiology. 2023 Aug 1:():1-9. doi: 10.1080/09286586.2023.2232462. Epub 2023 Aug 1 [PubMed PMID: 37528608]
Sarkar S, Tripathy K. Cortical Blindness. StatPearls. 2023 Jan:(): [PubMed PMID: 32809461]
Kraus CL, Culican SM. New advances in amblyopia therapy II: refractive therapies. The British journal of ophthalmology. 2018 Dec:102(12):1611-1614. doi: 10.1136/bjophthalmol-2018-312173. Epub 2018 Jun 5 [PubMed PMID: 29871968]
Level 3 (low-level) evidenceKelly KR, Jost RM, Wang YZ, Dao L, Beauchamp CL, Leffler JN, Birch EE. Improved Binocular Outcomes Following Binocular Treatment for Childhood Amblyopia. Investigative ophthalmology & visual science. 2018 Mar 1:59(3):1221-1228. doi: 10.1167/iovs.17-23235. Epub [PubMed PMID: 29625442]
Kelly KR, Jost RM, De La Cruz A, Dao L, Beauchamp CL, Stager D Jr, Birch EE. Slow reading in children with anisometropic amblyopia is associated with fixation instability and increased saccades. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2017 Dec:21(6):447-451.e1. doi: 10.1016/j.jaapos.2017.10.001. Epub 2017 Oct 9 [PubMed PMID: 29024763]
Kelly KR, Jost RM, De La Cruz A, Birch EE. Multiple-Choice Answer Form Completion Time in Children With Amblyopia and Strabismus. JAMA ophthalmology. 2018 Aug 1:136(8):938-941. doi: 10.1001/jamaophthalmol.2018.2295. Epub [PubMed PMID: 29902312]
Level 2 (mid-level) evidenceOstendorf GM. [Vision screening of children: rational and cost effective]. Versicherungsmedizin. 2013 Dec 1:65(4):207 [PubMed PMID: 24404617]
Level 2 (mid-level) evidence