Introduction
Eosinophilic pustular folliculitis (EPF), first reported in 1965 and previously known as Ofuji disease, is a rare dermatological condition found across diverse patient populations.[1] EPF comprises three distinct subtypes: EPF of infancy (EPFI), classic EPF of adulthood (EPF), and immunosuppression-associated EPF (IS-EPF). All three subtypes are characterized by a pruritic pustular skin eruption with a noninfectious origin and histological eosinophilic infiltrates. However, despite these similarities, treatment approaches and prognoses vary with each subtype.
This activity will review the epidemiology, proposed etiologies, presumptive pathophysiological processes, typical clinical presentation, evaluation, and management of EPF and highlight the role of the interprofessional team in caring for patients with this dermatological condition.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology of EPF is unknown, although multiple theories have been proposed.
Genetic predisposition may increase the risk of developing EPF, and studies have identified immunohistochemical markers that may be indicative of increased risk.[2] Further studies are needed to elucidate contributing genetic factors.
An immunological etiology of EPF has been proposed based on the high prevalence of EPF cases in patients living with the human immunodeficiency virus (HIV).[3] Additionally, studies of solid organ or hematopoietic transplant recipients receiving immunosuppressive therapy demonstrate an increased incidence of EPF.[4][5] The eosinophilic infiltrates characteristic of all forms of EPF typically indicate allergic and inflammatory responses, and it is hypothesized that an aberrant immune response triggers this eosinophilic inflammation. There are also reports of EPF developing in a typical medication-related adverse event scenario.[6][4]
The fact that EPF responds to such a diverse array of treatment modalities, including immunosuppressive medications, antimicrobials, and phototherapy, suggests the underlying etiologies of EPF may vary or be multifactorial. The intricate interplay between immune dysregulation, microbial factors, and genetic susceptibility necessitates further investigation to unravel the complex etiologic mechanisms and facilitate treatment regimens.
Epidemiology
EPF is a rare disorder with a wide geographic distribution, although it is most frequently reported in Japan. The prevalence in Asia, Europe, and the Americas varies widely. Adult EPF tends to present in the third and fourth decades.[7] EPF-I most commonly presents before 12 months of age and usually resolves by 36 months.[8] IS-EPF is most frequently identified in patients with advanced HIV disease or acquired immunodeficiency syndrome (AIDS). Approximately 5% of patients living with HIV will develop EPF at some time following their diagnosis.
All forms of EPF demonstrate a male-dominated gender predilection; the ratio of affected males to females is 5:1.[9]
Establishing precise epidemiological data is hindered by the rarity of EPF and the lack of large-scale studies.
Pathophysiology
The pathophysiology of EPF is not entirely understood. Immune dysregulation appears to play a role in the pathophysiologic processes associated with IS-EPF. Studies employing reverse transcriptase polymerase chain reaction (PCR) to measure mRNA expression have found elevated levels of interleukin-4, interleukin-5, RANTES (regulated on activation, normal T cell expressed and secreted), and eotaxins in patients with IS-EPF. These cytokines and chemokines increase the expression of T cells, especially type 2 helper T cells (TH2 cells).[10] Eotaxins also contribute to the migration and activation of eosinophils in allergic and inflammatory conditions.[11]
Furthermore, there are likely interactions between the skin microbiome and the immune system, judging by the variety of treatment options that have efficacy in specific patients, such as itraconazole or metronidazole.[7]
Histopathology
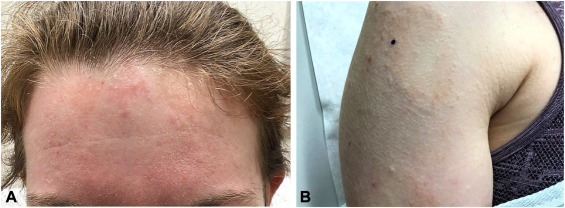
The 3 subtypes of EPF share the same histological features characterized by a brisk eosinophilic dermal infiltrate in a nonspecific perifollicular or perivascular distribution. (see Image. Eosinophilic pustular folliculitis) Additional findings include interstitial flame figures indicative of abundant eosinophil degranulation with subsequent coating of dermal collagen fibers and eosinophilic pustules at various levels, including hair follicles.[12]
History and Physical
The 3 subtypes of EPF commonly present in a similar fashion. Patients with EPF usually present with recurrent crops of intensely pruritic papules and sterile pustules in a seborrheic and hair-bearing distribution.[13] (see Image. Eosinophilic pustular folliculitis) A koebnerized distribution may also be observed during disease relapse.[14]
Flares of EPF last approximately 1 week and remain asymptomatic following treatment for approximately 4 weeks prior to relapse.[15] Atypical presentations of EPF may include extrafollicular plaques resembling pemphigus foliaceous.[16]
The course of the disease will vary according to subtype. The timeline of EPF-I, presenting within the first 14 months and resolving within the first 36 months, aids in differentiating EPF-I from the commonly seen erythema toxicum neonatorum and transient neonatal pustular melanosis, both of which occur in the neonatal period.[17] EPF-I is frequently localized to the scalp and rarely demonstrates an annular or serpiginous configuration.
Classic EPF presents in middle-aged men, with most cases demonstrating serpiginous and annular groups of papules and pustules on the face, back, and trunk. However, there are case reports of EPF appearing on the palms and soles.[18] EPF may also present as an isotopic response of Wolf by appearing in the area of a previously healed dermatosis.[19]
IS-EPF predominantly presents with excoriated and eczematous follicular papules, although it may arise in koebnerized or atypical areas.[15][20][21]
Evaluation
There are many etiologies of pustular eruptions, including conditions as common as acne vulgaris and as rare as graft-versus-host disease. Routine history-taking of patients with relapsing and remitting skin eruptions should pursue the identification of any underlying chronic immunosuppression. If the pruritic erythematous papulopustular condition fails to respond to a trial of topical steroids, Nomura et al propose potassium hydroxide microscopy of skin scrapings, a mineral oil preparation for microscopic evaluation, a complete blood count, HIV testing, and biopsy of a lesion that includes a pustule and hair follicle.[22]
Treatment / Management
The initial symptomatic treatment of all three subtypes of EPF is topical steroids. However, first-line therapy for classic EPF should also include indomethacin, which has shown favorable outcomes in typical and atypical presentations.[22][13](B3)
In patients with IS-EPF, the primary goal of therapy is a return to normal T-cell levels. If the underlying immunosuppression is due to HIV infection, highly active antiretroviral therapy (HAART) should be initiated, and other medications may be used to alleviate pruritus in the interim. Symptomatic IS-EPF and recalcitrant EPF may benefit from UVB phototherapy, low-dose isotretinoin, tumor necrosis factor-alpha (TNF-α) inhibitors, tetracyclines, systemic corticosteroids, metronidazole, itraconazole, or topical calcineurin inhibitors.[23][24][25][7](B3)
The goal of treatment for patients with EPF-I is alleviation of symptoms until the disease process spontaneously resolves; topical steroids or erythromycin may benefit.[22]
Scabicides such as permethrin may be helpful in some HIV-associated EPF cases. Permethrin acts on the nerve cell's membrane, disrupting sodium channel current, leading to dysregulation of the membrane's polarization.[7]
Antihistamines may help relieve itching in some instances of HIV-associated EPF. Sedating antihistamines may prove more helpful when patients experience nocturnal pruritus. Cyproheptadine can provide symptomatic relief of symptoms caused by histamine release from allergens leading to skin manifestations. Hydroxyzine antagonizes H1 receptors in the periphery, suppressing histamine action in the CNS. Cetirizine has also been used in cases of infantile EPF.[26]
Differential Diagnosis
The diagnostic protocol outlined by Nomura et al allows the astute clinician to rule in or out other common and uncommon pruritic pustular conditions such as bacterial and fungal folliculitis, seborrheic dermatitis, scabies, other arthropod assaults, pustular rosacea, and cutaneous T-cell lymphoma (mycosis fungoides). Other conditions to consider with similar signs or symptoms include photodermatitis, papular urticaria, and graft-versus-host-disease in organ transplant recipients.
EPF-I may present similarly to transient neonatal pustular melanosis, erythema toxicum neonatorum, acropustulosis of infancy, kerion, Langerhans cell histiocytosis, or acne neonatorum.[27]
Prognosis
The prognosis of EPF is dictated by the subtype. While classic EPF can be a chronic relapsing and remitting disease, EPF-I and IS-EPF have reliable endpoints of age and correction of underlying immunosuppression, respectively.
Complications
Complications of all subtypes of EPF tend to be mild and rare. However, in cases where the pustules are severe and persistent, scarring can occur and distort local free margins; if EPF occurs near the eyelid margin, ectropion may result.[25]
Deterrence and Patient Education
The existing literature on EPF is devoid of specific deterrence measures or distinctive patient education strategies. There is no evidence supporting dietary modifications or alterations in environmental exposures to alleviate the condition. Nevertheless, it is advised that patients refrain from excessive scratching of the lesions to mitigate the risk of secondary bacterial infection of the sterile pustules. Adherence may be challenging due to the pruritic nature of the disease process.
Enhancing Healthcare Team Outcomes
All subtypes of EPF have the potential to cause physical discomfort and negatively affect quality of life despite the benign nature of the disease process. Patients with classic EPF or EPF-I will most likely present to a primary care practitioner. Dermatology consultation will benefit patients with any subtype of EPF. Patients with chronic immunosuppression may present to the provider managing that disease process. In cases of secondary infection, infectious disease consultation may prove helpful.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
ISE S, OFUJI S. SUBCORNEAL PUSTULAR DERMATOSIS; A FOLLICULAR VARIANT? Archives of dermatology. 1965 Aug:92():169-71 [PubMed PMID: 14314743]
Teraki Y, Konohana I, Shiohara T, Nagashima M, Nishikawa T. Eosinophilic pustular folliculitis (Ofuji's disease). Immunohistochemical analysis. Archives of dermatology. 1993 Aug:129(8):1015-9 [PubMed PMID: 7688946]
Hayes BB, Hille RC, Goldberg LJ. Eosinophilic folliculitis in 2 HIV-positive women. Archives of dermatology. 2004 Apr:140(4):463-5 [PubMed PMID: 15096375]
Level 3 (low-level) evidenceChen J, Beatty CJ, Falcone LM, English JC 3rd, Kazlouskaya V. Eosinophilic Pustular Folliculitis in the Setting of Solid Organ Transplant Immunosuppression. Dermatology practical & conceptual. 2023 Apr 1:13(2):. doi: 10.5826/dpc.1302a78. Epub 2023 Apr 1 [PubMed PMID: 37196266]
Sasaki Y, Kishi A, Takagi S, Uchida N, Hayashi N. Eosinophilic pustular folliculitis after hematopoietic stem cell transplantation: A study of 11 cases. The Journal of dermatology. 2021 May:48(5):e231-e233. doi: 10.1111/1346-8138.15846. Epub 2021 Mar 14 [PubMed PMID: 33715192]
Level 3 (low-level) evidenceSmith SS, Cernaro N, Tonti E. Eosinophilic pustular folliculitis due to naltrexone: A case report. Journal of the American Pharmacists Association : JAPhA. 2022 Nov-Dec:62(6):1925-1928. doi: 10.1016/j.japh.2022.07.007. Epub 2022 Aug 3 [PubMed PMID: 35987727]
Level 3 (low-level) evidenceEllis E, Scheinfeld N. Eosinophilic pustular folliculitis: a comprehensive review of treatment options. American journal of clinical dermatology. 2004:5(3):189-97 [PubMed PMID: 15186198]
Ziemer M, Böer A. Eosinophilic pustular folliculitis in infancy: not a distinctive inflammatory disease of the skin. The American Journal of dermatopathology. 2005 Oct:27(5):443-55 [PubMed PMID: 16148418]
Takematsu H, Nakamura K, Igarashi M, Tagami H. Eosinophilic pustular folliculitis. Report of two cases with a review of the Japanese literature. Archives of dermatology. 1985 Jul:121(7):917-20 [PubMed PMID: 4015140]
Level 3 (low-level) evidenceAmerio P, Verdolini R, Proietto G, Feliciani C, Toto P, Shivji G, Loconsole F, Cassano N, Amerio P, Vena G, Sauder DN. Role of Th2 cytokines, RANTES and eotaxin in AIDS-associated eosinophilic folliculitis. Acta dermato-venereologica. 2001 May:81(2):92-5 [PubMed PMID: 11501668]
Amerio P, Frezzolini A, Feliciani C, Verdolini R, Teofoli P, De Pità O, Puddu P. Eotaxins and CCR3 receptor in inflammatory and allergic skin diseases: therapeutical implications. Current drug targets. Inflammation and allergy. 2003 Mar:2(1):81-94 [PubMed PMID: 14561178]
Level 3 (low-level) evidenceFertitta L, Bodemer C, Molina T, Frassati-Biaggi A, Fraitag S, Leclerc-Mercier S. Eosinophilic Pustular Folliculitis of Infancy: A Histologic Assessment of 43 Cases. The American Journal of dermatopathology. 2022 Jun 1:44(6):395-403. doi: 10.1097/DAD.0000000000002006. Epub 2021 Aug 5 [PubMed PMID: 35583404]
Level 3 (low-level) evidenceGrant GJ, Sahni DR, Florell AJ, Hull CM, Florell SR, Miles RR, Wada DA, Bowen AR. An atypical case of eosinophilic pustular folliculitis with associated secondary follicular mucinosis treated with indomethacin. JAAD case reports. 2023 Apr:34():86-89. doi: 10.1016/j.jdcr.2022.12.022. Epub 2023 Jan 27 [PubMed PMID: 37025561]
Level 3 (low-level) evidenceSialiti S, Khallaayoune M, Meziane M, Senouci K. Uncommon localisation of Ofuji disease in a Moroccan patient. BMJ case reports. 2021 Apr 13:14(4):. doi: 10.1136/bcr-2021-241606. Epub 2021 Apr 13 [PubMed PMID: 33849877]
Level 3 (low-level) evidenceNervi SJ, Schwartz RA, Dmochowski M. Eosinophilic pustular folliculitis: a 40 year retrospect. Journal of the American Academy of Dermatology. 2006 Aug:55(2):285-9 [PubMed PMID: 16844513]
Kakurai M, Oya K, Furuta J, Iijima S, Nomura T. A Case of Eosinophilic Pustular Folliculitis with Vegetating Lesions on the Lower Legs and Feet Resembling Pemphigus Vegetans. Acta dermato-venereologica. 2023 Apr 21:103():adv11622. doi: 10.2340/actadv.v103.11622. Epub 2023 Apr 21 [PubMed PMID: 37083096]
Level 3 (low-level) evidenceChadha A, Jahnke M. Common Neonatal Rashes. Pediatric annals. 2019 Jan 1:48(1):e16-e22. doi: 10.3928/19382359-20181206-01. Epub [PubMed PMID: 30653638]
Tsuboi H, Niiyama S, Katsuoka K. Eosinophilic pustular folliculitis (Ofuji disease) manifested as pustules on the palms and soles. Cutis. 2004 Aug:74(2):107-10 [PubMed PMID: 15379363]
Level 3 (low-level) evidenceXv L, Wang B, Zhu Q, Zhang G. A Case of Isotopic Response Presented with Eosinophilic Pustular Folliculitis. Clinical, cosmetic and investigational dermatology. 2023:16():1749-1752. doi: 10.2147/CCID.S415322. Epub 2023 Jul 7 [PubMed PMID: 37441695]
Level 3 (low-level) evidenceRikitake S, Kokubu H, Yamamoto B, Manabe T, Fujimoto N. Eosinophilic pustular folliculitis developing at the site of COVID-19 vaccination. Clinical and experimental dermatology. 2022 Nov:47(11):2022-2024. doi: 10.1111/ced.15293. Epub 2022 Jul 28 [PubMed PMID: 35699624]
Bronte Anaut M, Arredondo Montero J, Arpa Nadal E, Guarch Troyas R. A vulvar pseudotumor: A rare clinical presentation of eosinophilic folliculitis. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2022 May:157(2):484-485. doi: 10.1002/ijgo.14038. Epub 2021 Nov 23 [PubMed PMID: 34796483]
Nomura T, Katoh M, Yamamoto Y, Miyachi Y, Kabashima K. Eosinophilic pustular folliculitis: A proposal of diagnostic and therapeutic algorithms. The Journal of dermatology. 2016 Nov:43(11):1301-1306. doi: 10.1111/1346-8138.13359. Epub 2016 Mar 30 [PubMed PMID: 27028427]
Buchness MR, Lim HW, Hatcher VA, Sanchez M, Soter NA. Eosinophilic pustular folliculitis in the acquired immunodeficiency syndrome. Treatment with ultraviolet B phototherapy. The New England journal of medicine. 1988 May 5:318(18):1183-6 [PubMed PMID: 3362166]
Gallo G, Conti L, Quaglino P, Ribero S. Treatment of eosinophilic pustular folliculitis with low-dose isotretinoin. International journal of dermatology. 2022 Jul:61(7):e262-e264. doi: 10.1111/ijd.15929. Epub 2021 Sep 30 [PubMed PMID: 34591315]
Ramondetta A, Giuffrida G, Di Vincenzo S, De Pasquale R. A case of eosinophilic pustular folliculitis successfully treated with adalimumab. Dermatologic therapy. 2022 Jul:35(7):e15550. doi: 10.1111/dth.15550. Epub 2022 May 13 [PubMed PMID: 35508711]
Level 3 (low-level) evidenceOdyakmaz Demirsoy E, Demirsoy U, Ozod U, Kiran R. Eosinophilic pustular folliculitis of infancy suppressed with cetirizine. Pediatric dermatology. 2019 May:36(3):395-396. doi: 10.1111/pde.13764. Epub 2019 Feb 21 [PubMed PMID: 30791150]
Frølunde AS, Olesen AB, Riber-Hansen R, Pallesen KAU. Eosinophilic pustular folliculitis of infancy: A rare diagnosis in children. Clinical case reports. 2021 May:9(5):e04167. doi: 10.1002/ccr3.4167. Epub 2021 May 11 [PubMed PMID: 34026179]
Level 3 (low-level) evidence