Introduction
Cogan syndrome is an autoimmune disease characterized by inflammation of the inner ears and the eyes, presenting with vestibulo-auditory dysfunction and interstitial keratitis.[1] The disease progresses over 3 to 90 days and usually shows a response to steroid treatment.[2]
Humoral and cellular immune responses are the suggested mechanisms. There is expression and upregulation of cytokines like intercellular cell adhesion molecule-1 (ICAM-1) and (IL-)1β.[3] Originally, Baumgartner and Morgan described the disease in 1934 as non-syphilitic interstitial keratitis with vestibular dysfunction. However, Dr. David Cogan defined it as a clinical entity in 1945.[4]
Cogan syndrome is a diagnosis of exclusion, and other differentials, including syphilis, have to be ruled out before diagnosing Cogan syndrome. Other features of Cogan syndrome include fever, arthralgia, arthritis, headache, and myalgia. Vascular involvement, including aortitis, is an important manifestation of the disease. Cogan syndrome is treated with corticosteroids and immunomodulatory therapy. Biologics and immunomodulatory therapy are promising therapies to improve the prognosis in such patients.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
At first, Cogan syndrome was believed to be a result of Chlamydia psittaci infection because of remarkably elevated titers of antibodies to chlamydia trachomatis and the previous infection reported in a few patients.[5] The role of Chlamydia was not established by Vollertsen et al.[6]
Further literature on an infectious agent causing it has continued to stay negative, and antibiotic therapy has been unsuccessful.[4] Garcia Berrocal et al., in 1999, suggested that Cogan syndrome was due to hypersensitivity response to certain infectious agents, probably virus infection that provokes antibody response and cross-immunity with the proteins of the eye, audiovestibular system, and other organs.[7]
Presently it is thought that Cogan syndrome is an autoimmune disease. However, no particular biomarker is present in the standard workup of Cogan syndrome.[4]
Epidemiology
Cogan syndrome is a rare disorder, with around 250 cases announced so far.[4] It occurs mainly in young White race adults in the third decade of life.[8] The mean age of onset is 25 years, with a range of 5 to 63 years.[9] No gender predominance seemed to occur in the reported cases.[10]
It is an exceedingly rare disorder in Middle Eastern countries. However, the first case was reported in Jordan in 2012.[4] The number of cases could be more than reported as many may be falsely diagnosed as idiopathic keratitis and idiopathic hearing loss or deafness.[11]
Pathophysiology
Cogan syndrome is believed to be an autoimmune disease due to the detection of different autoantibodies and associated vasculitis, polyarteritis nodosa, and collagen vascular disease.[4] Furthermore, the antibodies against the Cogan peptide demonstrated a cross-reaction with Reovirus type III structural protein, proposing the involvement of a virus through a molecular mimicry mechanism. This suggests similarities between foreign and self-peptides resulting in the cross-activation of the cells by the peptides.[12]
Molecular mimicry is one of the mechanisms through which autoimmunity can arise. This happens when the exogenous agents such as bacteria, viruses, and others and human normal host-cell components share the antigenic determinants.[12] However, before the onset of Cogan syndrome, infection with Reovirus type III causing upper respiratory infections, pharyngitis, and mild rhinitis are frequently observed.[9]
A study was done in 2002 in which a peptide called Cogan peptide was discovered in 8 patients. The peptide was like reovirus III major core protein lambda and SSA/Ro.[12] Recently, anti-neutrophil cytoplasmic autoantibodies (ANCA) were discovered in 5 patients, and a few cases showed ANCA-related glomerulonephritis.[13]
Histopathology
A histopathologic examination of corneal tissue and cochlea by multiple groups showed plasma cells and lymphocytes infiltration, indicating a cell-mediated reaction that may explain the audiovestibular dysfunction, which includes severe vertigo, bilateral fluctuating hearing loss, and tinnitus.[14]
In addition to cochlear neuron loss, endolymphatic hydrops, new bone formation, degenerative changes in the organ of Corti, and atrophy and demyelination of vestibulocochlear cranial nerve may be noted.[15][16]
Further pathologic findings that are nonspecific yet compatible with a chronic inflammatory process include damaged aortic valves in aortitis, aortic valve cusp detachments and outpouchings, thinning or thickening, fenestrations, and retraction.[17][18]
Microscopically, lymphoid cell infiltration, myxomatous changes, and fibrinoid necrosis were revealed in the affected valves.[19][20][21]
History and Physical
Haynes and co-authors brought up a classification of Cogan syndrome in 1980 as typical (defined by Cogan) and atypical (structures other than cornea are involved, such as uvea, conjunctiva, sclera, optic disc, and retinal vessels).[22] Typical or classic Cogan syndrome is characterized by:
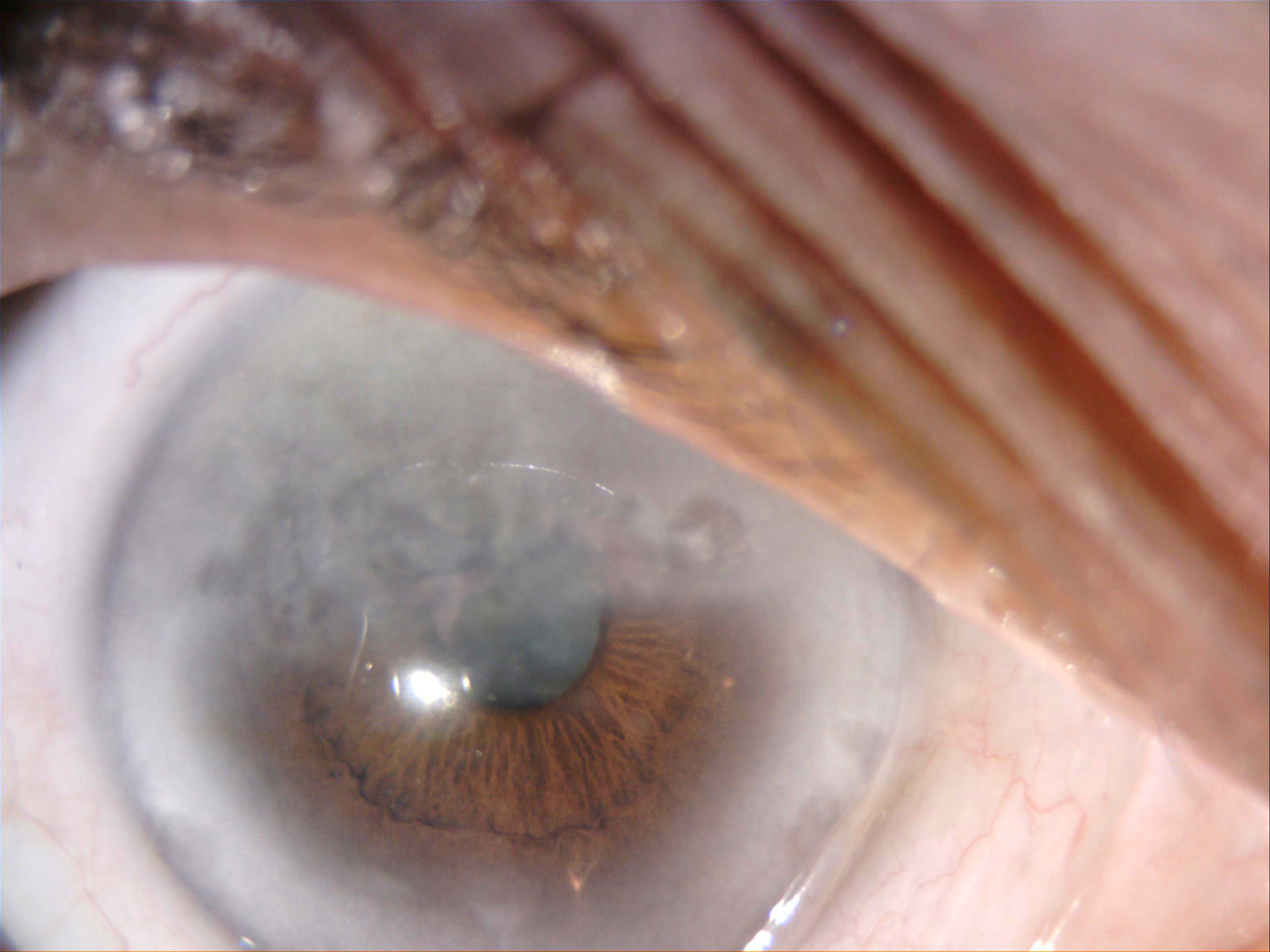
- 1- non-syphilitic interstitial keratitis (IK) with possible iritis, subconjunctival/conjunctival hemorrhage, lacrimation, and red-eye. The keratitis begins in the subepithelial region and rapidly evolves into interstitial keratitis that usually develops corneal neovascularization. Interstitial keratitis is the most common ocular feature of Cogan syndrome. One or both eyes can be involved. Usually, the visual prognosis is good. The interstitial keratitis progresses rapidly and then resolves, usually with corneal scarring and ghost vessels. The symptoms of active IK include redness, sensitivity to light (photophobia), visual decline, ocular pain, and watering. There may be recurrences of these symptoms years after initial resolution.
- 2- vestibular association similar to Ménière disease, with gradual hearing loss that might lead to deafness occurring within two years from the eye symptoms. The sensorineural hearing loss usually aggravates rapidly, usually leading to deafness in 1 to 3 months. In typical Cogan syndrome, the vestibulo-auditory symptoms arise within two years of ocular involvement.[5]
In contrast, atypical Cogan syndrome is when
- 1. other types of ocular involvement are present such as conjunctivitis, scleritis, choroiditis, episcleritis, uveitis, closed-angle glaucoma, retinal vasculitis, retinal hemorrhages, retinal artery occlusion, central retinal vein occlusion, exophthalmos, vasculitis optic neuropathy, papillitis, or optic disc edema,
- 2. audiovestibular symptoms do not resemble Ménière disease or appear before or after ocular symptoms for more than two years.[7] Systemic features are more common in atypical Cogan syndrome.
However, patients with typical Cogan syndrome may develop features of atypical Cogan syndrome later.[23]
Cogan syndrome follows an upper respiratory tract infection (URTI) episode in almost 27% of reported cases. A history of diarrhea, immunization or dental infections may be present. Mostly, the ears or the eyes alone are firstly affected. The most common ocular involvement is interstitial keratitis and other presentations: retinal vascular disease, scleritis, uveitis, episcleritis, papilledema, exophthalmos, conjunctivitis, and tendonitis. Seventy-four percent of patients present with ocular redness, 50% with pain, 50% with photophobia and tearing, and 42% with diminished visual acuity.
Examination shows ciliary injection associated with iritis, opacities in the corneal stroma, and a granular corneal infiltration, especially in the posterior portion of the cornea close to the limbus. Secondary corneal neovascularization usually occurs. Both eyes are involved in most patients. However, the symptoms may differ in each eye. Some patients may present with blindness or amaurosis.[24]
Multiple organs are affected in 2/3rd of cases, and another systemic disorder was seen in 1/3rd of the cases. Interstitial keratitis may not be the presenting feature and may develop years later. There may be sectoral conjunctival congestion with subepithelial/anterior corneal stromal peripheral or mid-peripheral keratitis.
The first system affected is the vestibular system, followed by the cochlear system in days or weeks. The symptoms are similar to recurrent Ménière disease, including nausea, vomiting, vertigo, and tinnitus. Progressive sensory hearing loss is noted that causes deafness in 1-3 months. Spontaneous nystagmus and a degree of ataxia can occur. A study by Grasland et al. showed that the disease affects both the ocular and audiovestibular system in 17/52 (33%) patients with typical Cogan syndrome compared to atypical Cogan syndrome (12% of patients).[24]
Systemic involvement is present in around 30 to 80% of patients. Cardiovascular manifestations typically involve aortitis, which leads to aortic insufficiency in around 10% of patients and congestive heart failure.[25]
Neurologic symptoms are nonspecific, including headache and coma. Some rare manifestations such as pyramidal syndrome, spinal cord disease, cerebellar syndrome, meningeal syndrome, peripheral neuropathy, facial palsy, and encephalitis may occur.[24]
Musculoskeletal manifestations may occur, including arthritis, myalgias, synovitis, arthralgia, and articular effusion. Results of muscle biopsies may be abnormal and show atrophy and muscle necrosis and may mimic myositis. The rest of the systemic manifestations are quite rare such as cutaneous signs (urticarial rash, erythematous rash, nodules, ulcerations, vascular purpura), lung involvement (dyspnea, cough, pleurisy, hemoptysis, thoracic pain, discrete abnormalities on radiological images), urinalysis abnormalities, and lymphadenopathies.[26]
Evaluation
Unfortunately, there is no particular marker for Cogan syndrome. However, some labs can be abnormal. Differential diagnoses must be ruled out by extensive investigations as Cogan syndrome is a diagnosis of exclusion. The usual findings are anemia, leukocytosis, thrombocytosis, and elevated ESR (erythrocyte sedimentation rate) along with hypofibrinogenemia and high CRP (c-reactive protein) during acute attacks. In some cases, antibodies against Chlamydia trachomatis or Chlamydia psittaci may be discovered. However, other features of infections may be absent.[24]
On urinalysis, proteinuria and hematuria may be present. Certain antibodies may be present, including antinuclear antibodies (ANA), antibodies to smooth muscle, lupus anticoagulants, cryoglobulins, anti-neutrophil cytoplasmic autoantibodies (ANCA), or rheumatoid factor (RF). In some cases, direct antibodies were detected against components of the inner ear and corneal antigen.[24]
Antibodies against heat shock protein may be present in around half of the patients with Cogan syndrome. Audiometry shows sensorineural hearing loss of all frequencies. Word recognition ability might improve or deteriorate; the initial evaluation demonstrates sensory hearing loss with abnormal electronystagmography.[27]
Treatment / Management
Treatment of Cogan syndrome depends on its severity, whether it is limited to ocular disease or extensive inner ear, ocular or systemic vasculitis. High-dose corticosteroids (1 to 2 mg/kg/day) for systemic vasculitis are the first line to obtain remission.[28]
If an improvement occurs, corticosteroids may be tapered over 2 to 6 months. The corticosteroid should be discontinued if no response occurs. Failure of treatment will require additional immunosuppressive therapy like methotrexate, azathioprine, cyclophosphamide, and cyclosporine A, which have shown better outcomes.[29][30] (B3)
Interstitial keratitis is treated with topical steroids and cycloplegics, systemic steroids, disease-modifying anti-rheumatic drugs (DMARDs), and biologics.
The early treatment with systemic corticosteroids determines the course of audiovestibular involvement. However, corticosteroid eye drops or local atropine can be used for interstitial keratitis, which shows a good response. Cogan syndrome with large vessel vasculitis has also been treated with oral cyclophosphamide (starting at 2 to 3 mg/kg/day) given for four to six months. If no response to cyclophosphamide is noted, cyclosporine (4 mg/kg/day or less) may be used.[30](B3)
Tumor necrosis factors (TNF-a) inhibitory agents have recently been another therapeutic option, with infliximab, a chimeric anti-TNF-a monoclonal antibody being the most effective, according to a recent literature review that showed 11 out of 12 cases treated with infliximab have achieved clinical remission.[31][32] (B3)
Rituximab has been shown to reduce the medications used to control the systemic manifestations and help avoid cochlear implants or deafness in certain severe cases; however, it is not used as a first-line.[33] For those who did not respond to pharmacologic therapy for hearing loss, cochlear implants have been beneficial.[34][35] (B2)
Benzodiazepines, antihistamines, or vestibular therapy can be used for chronic vestibular dysfunction that occurs in a few cases.[36] A fast-growing interest in stem-cell-based treatment has developed for autoimmune disorders; however, additional studies are required to confirm the long-term safety and efficacy.[37](B3)
Differential Diagnosis
Various diseases have been included in the differential diagnosis of Cogan syndrome due to the audiovestibular and ocular associations such as these:
- Susac syndrome (retinocochleocerberal vasculopathy or SICRET syndrome-small infarctions of cochlear, retinal, and encephalic tissue): Susac syndrome is characterized by lesions of the cochlear, retinal, and cerebral arterioles.[4]
- Congenital syphilis: The Hutchinson triad of congenital syphilis includes Hutchinson teeth (notched peg-shaped upper incisors), interstitial keratitis, and sensorineural hearing loss.[38] Serology for syphilis must be negative for making a diagnosis of Cogan syndrome.
- The association of necrotizing vasculitis after acute serous otitis media and acute episcleritis described by Sergent and Christian in 1994 (with no inner ear involvement)
- Vogt-Koyanagi-Harada syndrome: Vogt-Koyanagi-Harada syndrome is identified by diminished visual acuity, sensorineural hearing loss, and uveoencephalitis with meningism (which sometimes occurs in Cogan syndrome), poliosis, and alopecia. Meningism may occur in patients with Cogan syndrome. However, alopecia and poliosis do not.[26]
- Polyarteritis nodosa
- Granulomatosis with polyangiitis: Granulomatosis with polyangiitis often involves the ear and eye. Vasculitic changes involving small vessels, pulmonary infiltrates, glomerulonephritis, hemorrhagic lesions of the nose and throat, and the presence of c-ANCA (cytoplasmic ANCA) are usually seen in patients with granulomatosis with polyangiitis (previously called Wegner granulomatosis). Cogan syndrome patients do not fulfill these criteria.
- Takayasu arteritis[11]
It is challenging to diagnose Cogan syndrome during the early stages of the disease. However, the coexistence between Cogan syndrome and other autoimmune disorders has been revealed by a literature review, such as the presence of Cogan syndrome with rheumatoid arthritis, granulomatosis with polyangiitis, and tubulointerstitial nephritis, and uveitis (TINU syndrome).[39]
A study showed that four patients with inflammatory bowel disease (IBD) presented with Cogan syndrome, ocular inflammation, and sensorineural hearing loss (SNHL) after the GI (gastrointestinal) symptoms.[40] A large international multicenter study reported 22 CS-IBD patients; half of them had Cogan syndrome onset after the GI symptoms.[41]
Differential diagnoses of interstitial keratitis include syphilis, chlamydia, leprosy, tuberculosis, brucellosis, leptospirosis, Lyme disease, herpes, measles, mumps, pox, parasitic infestation (onchocerciasis), and autoimmune diseases (rheumatoid arthritis, sarcoidosis, granulomatosis with polyangiitis).[42]
Prognosis
The prognosis for Cogan syndrome is generally poor when ear, eye, and cardiovascular involvement occur. In contrast to corneal disease, ear disease has a poor prognosis in the long term as deafness will be irreversible.[26]
Complete hearing loss was noted in one ear in 18 percent and both ears in 52 percent of 60 patients who received care at Mayo clinic between 1940 and 2002. At the final follow-up, most patients had normal or near-normal eyesight in this study. A retrospective study on Cogan syndrome from France showed higher relapse rates from patients at Mayo clinic (78% during 7.1 years of follow-up) than relapse rates (13 and 31 percent of patients relapsed at 5 and 10 years, respectively).[43]
Both groups were uniformly treated with high doses of glucocorticoids. However, the patients from the French study had more use of immunosuppressive agents than those managed at the Mayo Clinic. In the French study, ten patients were treated with infliximab which was only approved in late 1998. Deterioration of auditory performance after cochlear implants have been noticed by Bovo et al. due to the progression of new bone in the cochlea, which separates the electrode from neural structures.[44][45]
Complications
Systemic vasculitis, usually involving large and/or medium vessels, has been reported in 15 to 21% of cases. However, vessels of any size may be affected.[46] Life-threatening complications were reported in 10% of cases like aortic insufficiency, aneurysms, and dissection.[47] Other valves were involved leading to complications including mitral insufficiency.[48]
Organs that may be affected by systemic vasculitis include the brain and kidneys, as the stroke was seen in some Cogan syndrome patients.[49] Neurological symptoms include aphasia due to TIA (transient ischemic attack), hemiplegia, and hemiparesis due to a cerebral vascular accident.
Deterrence and Patient Education
Cogan syndrome is a rare autoimmune disorder that presents with audiovestibular symptoms and non-syphilitic interstitial keratitis. The beneficial response to corticosteroids supports autoimmune pathogenesis. However, the treatment is sometimes difficult as failure to treat hearing loss may cause deafness. Permanent hearing loss usually occurs due to recurrent flares.[50]
The first line of treatment is corticosteroids. Additionally, multiple immunosuppressive drugs have been used.[50] Cochlear implantation is a surgical strategy used in cases with severe sensorineural hearing loss and failure of intensive immunosuppressive regimens.[50]
The patients and caregivers should be explained the prognosis, management, and outcome to ensure compliance and the best possible outcome.
Enhancing Healthcare Team Outcomes
The collaboration of the entire healthcare team is mandatory for the management of this condition. The primary care providers should be oriented about this disorder, especially if they present with progressive hearing loss and eye pain. A referral to an ophthalmologist and otolaryngologist for further assessment is mandatory. Screening for other autoimmune diseases should be considered to improve prognosis and outcomes.
Media
(Click Image to Enlarge)
References
Kessel A, Vadasz Z, Toubi E. Cogan syndrome--pathogenesis, clinical variants and treatment approaches. Autoimmunity reviews. 2014 Apr-May:13(4-5):351-4. doi: 10.1016/j.autrev.2014.01.002. Epub 2014 Jan 10 [PubMed PMID: 24418297]
McCabe BF. Autoimmune sensorineural hearing loss. The Annals of otology, rhinology, and laryngology. 1979 Sep-Oct:88(5 Pt 1):585-9 [PubMed PMID: 496191]
Level 3 (low-level) evidenceGoodall AF, Siddiq MA. Current understanding of the pathogenesis of autoimmune inner ear disease: a review. Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 2015 Oct:40(5):412-9. doi: 10.1111/coa.12432. Epub [PubMed PMID: 25847404]
Level 3 (low-level) evidenceIliescu DA, Timaru CM, Batras M, De Simone A, Stefan C. COGAN'S SYNDROME. Romanian journal of ophthalmology. 2015 Jan-Mar:59(1):6-13 [PubMed PMID: 27373108]
Haynes BF, Kaiser-Kupfer MI, Mason P, Fauci AS. Cogan syndrome: studies in thirteen patients, long-term follow-up, and a review of the literature. Medicine. 1980 Nov:59(6):426-41 [PubMed PMID: 6969345]
Vollertsen RS. Vasculitis and Cogan's syndrome. Rheumatic diseases clinics of North America. 1990 May:16(2):433-9 [PubMed PMID: 2189159]
García Berrocal JR, Vargas JA, Vaquero M, Ramón y Cajal S, Ramírez-Camacho RA. Cogan's syndrome: an oculo-audiovestibular disease. Postgraduate medical journal. 1999 May:75(883):262-4 [PubMed PMID: 10533627]
Level 3 (low-level) evidenceTayer-Shifman OE, Ilan O, Tovi H, Tal Y. Cogan's syndrome--clinical guidelines and novel therapeutic approaches. Clinical reviews in allergy & immunology. 2014 Aug:47(1):65-72. doi: 10.1007/s12016-013-8406-7. Epub [PubMed PMID: 24385257]
Level 3 (low-level) evidenceVollertsen RS, McDonald TJ, Younge BR, Banks PM, Stanson AW, Ilstrup DM. Cogan's syndrome: 18 cases and a review of the literature. Mayo Clinic proceedings. 1986 May:61(5):344-61 [PubMed PMID: 3486332]
Level 3 (low-level) evidenceAzami A, Maleki N, Kalantar Hormozi M, Tavosi Z. Interstitial Keratitis, Vertigo, and Vasculitis: Typical Cogan's Syndrome. Case reports in medicine. 2014:2014():830831. doi: 10.1155/2014/830831. Epub 2014 Mar 4 [PubMed PMID: 24715922]
Level 3 (low-level) evidenceGaubitz M, Lübben B, Seidel M, Schotte H, Gramley F, Domschke W. Cogan's syndrome: organ-specific autoimmune disease or systemic vasculitis? A report of two cases and review of the literature. Clinical and experimental rheumatology. 2001 Jul-Aug:19(4):463-9 [PubMed PMID: 11491507]
Level 3 (low-level) evidenceLunardi C, Bason C, Leandri M, Navone R, Lestani M, Millo E, Benatti U, Cilli M, Beri R, Corrocher R, Puccetti A. Autoantibodies to inner ear and endothelial antigens in Cogan's syndrome. Lancet (London, England). 2002 Sep 21:360(9337):915-21 [PubMed PMID: 12354474]
Level 3 (low-level) evidenceYamanishi Y, Ishioka S, Takeda M, Maeda H, Yamakido M. Letter to the Editor. Atypical Cogan's syndrome associated with antineutrophil cytoplasmic autoantibodies. British journal of rheumatology. 1996 Jun:35(6):601-2 [PubMed PMID: 8670587]
Level 3 (low-level) evidenceFISHER ER, HELLSTROM HR. Cogan's syndrome and systemic vascular disease. Analysis of pathologic features with reference to its relationship to thromboangiitis obliterans (Buerger). Archives of pathology. 1961 Nov:72():572-92 [PubMed PMID: 13893233]
Level 3 (low-level) evidenceRarey KE, Bicknell JM, Davis LE. Intralabyrinthine osteogenesis in Cogan's syndrome. American journal of otolaryngology. 1986 Nov-Dec:7(6):387-90 [PubMed PMID: 3099589]
Level 3 (low-level) evidenceSchuknecht HF, Nadol JB Jr. Temporal bone pathology in a case of Cogan's syndrome. The Laryngoscope. 1994 Sep:104(9):1135-42 [PubMed PMID: 8072362]
Level 3 (low-level) evidenceCochrane AD, Tatoulis J. Cogan's syndrome with aortitis, aortic regurgitation, and aortic arch vessel stenoses. The Annals of thoracic surgery. 1991 Nov:52(5):1166-7 [PubMed PMID: 1953144]
Level 3 (low-level) evidenceLivingston JZ, Casale AS, Hutchins GM, Shapiro EP. Coronary involvement in Cogan's syndrome. American heart journal. 1992 Feb:123(2):528-30 [PubMed PMID: 1736593]
Level 3 (low-level) evidenceGelfand ML, Kantor T, Gorstein F. Cogan's syndrome with cardiovascular involvement: aortic insufficiency. Bulletin of the New York Academy of Medicine. 1972 May:48(4):647-60 [PubMed PMID: 4503925]
EISENSTEIN B, TAUBENHAUS M. Nonsyphilitic interstitial keratitis and bilateral deafness (Cogan's syndrome) associated with cardiovascular disease. The New England journal of medicine. 1958 May 29:258(22):1074-9 [PubMed PMID: 13552923]
Level 3 (low-level) evidencePinals RS. Cogan's syndrome with arthritis and aortic insufficiency. The Journal of rheumatology. 1978 Fall:5(3):294-8 [PubMed PMID: 748553]
Level 3 (low-level) evidenceBonaguri C, Orsoni J, Russo A, Rubino P, Bacciu S, Lippi G, Melegari A, Zavota L, Ghirardini S, Mora P. Cogan's syndrome: anti-Hsp70 antibodies are a serological marker in the typical form. The Israel Medical Association journal : IMAJ. 2014 May:16(5):285-8 [PubMed PMID: 24979832]
Espinoza GM, Wheeler J, Temprano KK, Keller AP. Cogan's Syndrome: Clinical Presentations and Update on Treatment. Current allergy and asthma reports. 2020 Jun 16:20(9):46. doi: 10.1007/s11882-020-00945-1. Epub 2020 Jun 16 [PubMed PMID: 32548646]
Grasland A, Pouchot J, Hachulla E, Blétry O, Papo T, Vinceneux P, Study Group for Cogan's Syndrome. Typical and atypical Cogan's syndrome: 32 cases and review of the literature. Rheumatology (Oxford, England). 2004 Aug:43(8):1007-15 [PubMed PMID: 15150435]
Level 3 (low-level) evidenceKaya M, Erkanlı K, Kılınç F, Sar M, Bakır İ. Surgical Treatment in a Case of Cogan's Syndrome Complicated With Proximal Aortic Vasculitis. The Annals of thoracic surgery. 2015 Oct:100(4):1467-9. doi: 10.1016/j.athoracsur.2015.01.049. Epub [PubMed PMID: 26434452]
Level 3 (low-level) evidenceNdiaye IC, Rassi SJ, Wiener-Vacher SR. Cochleovestibular impairment in pediatric Cogan's syndrome. Pediatrics. 2002 Feb:109(2):E38 [PubMed PMID: 11826248]
Level 3 (low-level) evidenceOsborne DC, Jacobson JT, Olsen ML. Cogan's syndrome: auditory and medical management. Journal of the American Academy of Audiology. 1992 May:3(3):225-9 [PubMed PMID: 1581598]
Level 3 (low-level) evidenceShamriz O, Tal Y, Gross M. Autoimmune Inner Ear Disease: Immune Biomarkers, Audiovestibular Aspects, and Therapeutic Modalities of Cogan's Syndrome. Journal of immunology research. 2018:2018():1498640. doi: 10.1155/2018/1498640. Epub 2018 Apr 23 [PubMed PMID: 29850616]
Matteson EL, Tirzaman O, Facer GW, Fabry DA, Kasperbauer J, Beatty CW, McDonald TJ. Use of methotrexate for autoimmune hearing loss. The Annals of otology, rhinology, and laryngology. 2000 Aug:109(8 Pt 1):710-4 [PubMed PMID: 10961801]
Allen NB, Cox CC, Cobo M, Kisslo J, Jacobs MR, McCallum RM, Haynes BF. Use of immunosuppressive agents in the treatment of severe ocular and vascular manifestations of Cogan's syndrome. The American journal of medicine. 1990 Mar:88(3):296-301 [PubMed PMID: 2309745]
Level 3 (low-level) evidenceTouma Z, Nawwar R, Hadi U, Hourani M, Arayssi T. The use of TNF-alpha blockers in Cogan's syndrome. Rheumatology international. 2007 Aug:27(10):995-6 [PubMed PMID: 17564714]
Level 3 (low-level) evidenceKalogeropoulos C, Karachalios D, Pentheroudakis G, Tsikou-Papafrangou A, Abou-Asabeh L, Argyropoulou M, Drosos A, Pavlidis N. Development of a low grade lymphoma in the mastoid bone in a patient with atypical Cogan's syndrome: A case report. Journal of advanced research. 2015 May:6(3):523-7. doi: 10.1016/j.jare.2014.05.003. Epub 2014 May 16 [PubMed PMID: 26257951]
Level 3 (low-level) evidenceOrsoni JG, Laganà B, Rubino P, Zavota L, Bacciu S, Mora P. Rituximab ameliorated severe hearing loss in Cogan's syndrome: a case report. Orphanet journal of rare diseases. 2010 Jun 16:5():18. doi: 10.1186/1750-1172-5-18. Epub 2010 Jun 16 [PubMed PMID: 20550723]
Level 3 (low-level) evidencePeters BR, Wyss J, Manrique M. Worldwide trends in bilateral cochlear implantation. The Laryngoscope. 2010 May:120 Suppl 2():S17-44. doi: 10.1002/lary.20859. Epub [PubMed PMID: 20422715]
Level 2 (mid-level) evidenceWang JR, Yuen HW, Shipp DB, Stewart S, Lin VY, Chen JM, Nedzelski JM. Cochlear implantation in patients with autoimmune inner ear disease including cogan syndrome: a comparison with age- and sex-matched controls. The Laryngoscope. 2010 Dec:120(12):2478-83. doi: 10.1002/lary.21060. Epub [PubMed PMID: 21082747]
Level 2 (mid-level) evidenceCoelho DH, Lalwani AK. Medical management of Ménière's disease. The Laryngoscope. 2008 Jun:118(6):1099-108. doi: 10.1097/MLG.0b013e31816927f0. Epub [PubMed PMID: 18418279]
Ben-Ami E, Berrih-Aknin S, Miller A. Mesenchymal stem cells as an immunomodulatory therapeutic strategy for autoimmune diseases. Autoimmunity reviews. 2011 May:10(7):410-5. doi: 10.1016/j.autrev.2011.01.005. Epub 2011 Jan 20 [PubMed PMID: 21256250]
Level 3 (low-level) evidenceTripathy K, Sharma YR, Chawla R, Basu K, Vohra R, Venkatesh P. Triads in Ophthalmology: A Comprehensive Review. Seminars in ophthalmology. 2017:32(2):237-250. doi: 10.3109/08820538.2015.1045150. Epub 2015 Jul 6 [PubMed PMID: 26148300]
Brogan K, Eleftheriou D, Rajput K, Edelsten C, Sebire NJ, Brogan PA. Tubulointerstitial nephritis, uveitis, hearing loss and vestibular failure: TINU-atypical Cogan's overlap syndrome. Rheumatology (Oxford, England). 2012 May:51(5):950-2. doi: 10.1093/rheumatology/ker443. Epub 2012 Jan 11 [PubMed PMID: 22240503]
Level 3 (low-level) evidenceScharl M, Frei P, Fried M, Rogler G, Vavricka SR. Association between Cogan's syndrome and inflammatory bowel disease: a case series. Journal of Crohn's & colitis. 2011 Feb:5(1):64-8. doi: 10.1016/j.crohns.2010.09.003. Epub 2010 Oct 29 [PubMed PMID: 21272808]
Level 3 (low-level) evidenceVavricka SR, Greuter T, Scharl M, Mantzaris G, Shitrit AB, Filip R, Karmiris K, Thoeringer CK, Boldys H, Wewer AV, Yanai H, Flores C, Schmidt C, Kariv R, Rogler G, Rahier JF, ECCO CONFER investigators. Cogan's Syndrome in Patients With Inflammatory Bowel Disease--A Case Series. Journal of Crohn's & colitis. 2015 Oct:9(10):886-90. doi: 10.1093/ecco-jcc/jjv128. Epub 2015 Jul 17 [PubMed PMID: 26188351]
Level 2 (mid-level) evidenceGyasi ME, Okonkwo ON, Tripathy K. Onchocerciasis. StatPearls. 2025 Jan:(): [PubMed PMID: 32644453]
Durtette C, Hachulla E, Resche-Rigon M, Papo T, Zénone T, Lioger B, Deligny C, Lambert M, Landron C, Pouchot J, Kahn JE, Lavigne C, De Wazieres B, Dhote R, Gondran G, Pertuiset E, Quemeneur T, Hamidou M, Sève P, Le Gallou T, Grasland A, Hatron PY, Fain O, Mekinian A, SNFMI and CRI. Cogan syndrome: Characteristics, outcome and treatment in a French nationwide retrospective study and literature review. Autoimmunity reviews. 2017 Dec:16(12):1219-1223. doi: 10.1016/j.autrev.2017.10.005. Epub 2017 Oct 14 [PubMed PMID: 29037902]
Level 2 (mid-level) evidencePasanisi E, Vincenti V, Bacciu A, Guida M, Berghenti T, Barbot A, Orsoni JG, Bacciu S. Cochlear implantation and Cogan syndrome. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2003 Jul:24(4):601-4 [PubMed PMID: 12851552]
Level 2 (mid-level) evidenceKawamura S, Sakamoto T, Kashio A, Kakigi A, Ito K, Suzuki M, Yamasoba T. Cochlear implantation in a patient with atypical Cogan's syndrome complicated with hypertrophic cranial pachymeningitis. Auris, nasus, larynx. 2010 Dec:37(6):737-41. doi: 10.1016/j.anl.2010.04.005. Epub 2010 Jun 25 [PubMed PMID: 20576375]
Level 3 (low-level) evidenceGreco A, Gallo A, Fusconi M, Magliulo G, Turchetta R, Marinelli C, Macri GF, De Virgilio A, de Vincentiis M. Cogan's syndrome: an autoimmune inner ear disease. Autoimmunity reviews. 2013 Jan:12(3):396-400. doi: 10.1016/j.autrev.2012.07.012. Epub 2012 Jul 28 [PubMed PMID: 22846458]
Level 3 (low-level) evidenceSu JW, Low AH, Tay KH, Sebastian MG, Thumboo J, Sin KY. Recurrent aortic aneurysms following thoracic aortic stent-graft repair in a patient with Cogan syndrome. Journal of endovascular therapy : an official journal of the International Society of Endovascular Specialists. 2006 Dec:13(6):779-82 [PubMed PMID: 17154705]
Gasparovic H, Djuric Z, Bosnic D, Petricevic M, Brida M, Dotlic S, Biocina B. Aortic root vasculitis associated with Cogan's syndrome. The Annals of thoracic surgery. 2011 Jul:92(1):340-1. doi: 10.1016/j.athoracsur.2010.12.068. Epub [PubMed PMID: 21718871]
Level 3 (low-level) evidenceKarni A, Sadeh M, Blatt I, Goldhammer Y. Cogan's syndrome complicated by lacunar brain infarcts. Journal of neurology, neurosurgery, and psychiatry. 1991 Feb:54(2):169-71 [PubMed PMID: 2019845]
Level 3 (low-level) evidenceD'Aguanno V, Ralli M, de Vincentiis M, Greco A. Optimal management of Cogan's syndrome: a multidisciplinary approach. Journal of multidisciplinary healthcare. 2018:11():1-11. doi: 10.2147/JMDH.S150940. Epub 2017 Dec 22 [PubMed PMID: 29317827]