Introduction
Ectopia lentis refers to the hereditary or acquired malposition of the natural crystalline lens out of the patellar fossa.[1] The first report came from Berry, who documented the first case of lenticular dislocation in 1749. Later, Stellwag was the first to name it ectopia lentis in 1856 in a patient with congenital dislocation of the lens.[2] It can be hereditary (familial) or acquired. The lens can be subluxated or dislocated away from the patellar fossa. The cause can be traumatic or secondary to underlying systemic disease. The lens can be seen in the anterior chamber, vitreous phase, or retinal surface. Ectopia lentis can be a primary manifestation of a systemic disorder and should arouse suspicion of underlying systemic pathology. This is a disorder with varied etiologies.[3]
A detailed past and systemic history are necessary in each case. The patient should be questioned regarding cardiovascular, skeletal, and any other ocular abnormalities. A thorough ocular and systemic examination help in clinching the diagnosis. Family members should also be evaluated to pinpoint the genetic association. The pediatrician also plays a crucial role in ruling out familial disorders. The patient's visual outcome depends on the degree and extent of subluxation or dislocation and the presence and absence of complications.[4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology of ectopia lentis is broadly grouped as congenital, traumatic, metabolic/syndromic, and consecutive/spontaneous.[5]
Trauma
Ectopia lentis can be a manifestation of trauma, ocular pathology, or systemic disease. The most common cause is trauma. It can occur secondary to blunt trauma to the head and eye or directly impact the eye. Traumatic ectopia lentis can be present at birth or manifest at any age. In case of minor traumatic injury, other causes and associations of ectopia lentis should be ruled out.[6]
Ocular Disease and Associations of Ectopia Lentis
Simple Ectopia Lentis
It can be congenital or acquired later spontaneously. Both can be autosomal dominant or recessive. Autosomal recessive inheritance is rare and is reported in families with a history of consanguineous marriage. In simple ectopia lentis, the lens displacement is usually bilateral and supero-temporal, and the degree of displacement varies between the two eyes. In autosomal recessive inheritance, a mutation in the ADAMTSL4 gene on chromosome 1 has been reported. In autosomal dominant inheritance, a mutation in the FBN1 gene located on chromosome 15 has been reported.[7]
FBN1 gene mutation has also been reported in Marfan syndrome. Hence there occurs a significant genetic overlap between simple ectopia lentis and systemic diseases like Marfan syndrome. Spontaneous, simple ectopia lentis is usually reported in the age group of 20 to 65 years. The congenital and spontaneous variety can be associated with cataracts, retinal detachment, or secondary glaucoma. With lens dislocation, there also occur vitreous prolapse through weak zonular fibers.[8]
Ectopia Lentis Et Pupillae
This is a rare and congenital autosomal recessive condition. In this, the pupil and lens are displaced in opposite directions. The pupil becomes asymmetric, eccentric, oval, and ectopic. There is minimal pupillary dilatation, and the lens displacement is usually bilateral and asymmetric. The iris atrophy is evident and appears as a transillumination defect on the slit lamp. Microspherophakia may be present.[9]
Ocular Associations of Ectopia Lentis
- Congenital glaucoma
- Chronic cyclitis
- Pseudoexfoliation syndrome
- Aniridia
- High myopia
- Retinitis pigmentosa
- Megalocornea
- Buphthalmos
- Intraocular tumors
- Hypermature cataract
- Syphilis
- Axenfeld-Rieger syndrome
- Trauma
- Persistent pupillary membrane
- Dominantly inherited blepharoptosis and high myopia
Ectopia Lentis- Systemic Associations
Marfan Syndrome
Marfan syndrome is the most common syndrome associated with ectopia lentis. It is seen in approximately 80% of the patients with Marfan syndrome. The syndrome is autosomal dominant with fibrillin-1 gene mutation located on chromosome 15.[10]
Ectopia lentis in Marfan syndrome is linked to alteration of fibrillin microfibers leading to deficient zonules and structural alteration in the lenticular capsule. The accommodation is usually retained, and rarely can the lens dislocate into the anterior chamber or vitreous cavity. A bilateral supero-temporal lens displacement is seen in Marfan syndrome. It can also be seen in other directions. The various systemic manifestations of Marfan syndrome can be remembered as the MASS phenotype (myopia, mitral valve prolapse, aortic root dilatation, skin, and skeletal involvement).[11]
- Cardiovascular
- Aortic root dilatation, aneurysms of the aorta, and mitral valve prolapse.[12]
- Musculoskeletal
- Lean, thin and tall stature, disproportionate arm and limb ratio, usually the arm span is greater than height, fingers and toes are relatively long leading to arachnodactyly, and a high arched palate also called as the gothic palate is seen. The other musculoskeletal features are kyphosis, Shprintzen–Goldberg syndrome, scoliosis, sternal bone abnormalities, hypermobile joints, muscular atrophy, hiatus, and inguinal hernia.
- Other features- Secondary glaucoma, lattice retinal degeneration, retinal detachment, microspherophakic lens, strabismus, and hypoplasia of dilator pupillae.[13]
Weill–Marchesani Syndrome
It is the reverse of Marfan's syndrome, in which the primary defect is in the connective tissue. The gene involved is FBN1 (polymorphisms), and it can be autosomal dominant or recessive. Ectopia lentis is seen in approximately 50% with inferior lens subluxation. It can be seen in adolescence or early adulthood. The other common ocular manifestations can be microspherophakic and pupillary block glaucoma. The systemic features can be short stature, short fingers of hands and toes, brachydactyly, and delayed milestones resulting in learning difficulty.[14]
Homocystinuria
This is the second most common etiology for inheritable ectopia lentis. The condition is autosomal recessive, and there is a deficiency of enzyme cystathionine b- synthetase. There occurs systemic accumulation of methionine and homocysteine. It is often characterized by mental handicap, osteoporosis, chest abnormalities, atherosclerosis, and increased incidence of thrombosis.[15]
The other features include blue iris, coarse blonde hair, marfanoid habitus, and malar flush. Ectopia lentis is seen in nearly 90%, probably due to deficient zonules secondary to enzymatic deficiency. Ectopia lentis is bilateral, and in 60%, inferonasal dislocation is seen. Ectopia lentis is observed in nearly 100% of cases by 25 years. The treatment includes oral vitamin B6, B12, and folic acid to alleviate plasma homocysteine and methionine levels. The other ocular complications can be iris transillumination defects, optic atrophy, cataract, retinal detachment, and myopia.[16]
Other Systemic Associations
- Sulfite oxidase deficiency (ectopia lentis in 100% cases)
- Hyperlysinemia
- Ehlers Danlos syndrome
- Sturge Weber syndrome
- Sticklers syndrome
- Sprengel deformity
- Pierre Robin syndrome
- Mandibulofacial dysostosis
- Wildervanck syndrome
- Conradi syndrome
- Pfaundler syndrome
- Crouzon syndrome
- Marfan-like syndrome with hyaloretinal degeneration
- Syphilis
- Crouzon disease
- Refsum syndrome
- Scleroderma
- Kniest syndrome
Epidemiology
Ectopia lentis is more common in males than females, probably due to trauma. The proportion of male and female ocular involvement can vary with the degree of lens displacement. It can manifest at any age, from birth to adulthood. The reported prevalence of congenital ectopia lentis is 6 per 100,000.[5]
Pathophysiology
In Marfan syndrome, ectopia lentis occurs due to heterozygous mutations in the FBN1 gene, which result in haploinsufficiency of the protein fibrillin-1.[17] This causes architectural damage to the microfibrillar extracellular matrix. Fibrillin is a component of ciliary zonules, and mutations in fibrillin result in a deficiency of zonular fibers, which manifests as a subluxated lens.[18]
Ahram et al. documented homozygous mutations in ADAMTSL4 on chromosome 1 of Jordanian patients, responsible for autosomal recessive ectopia lentis.[19] In ectopia lentis, et pupillae, the persistent mesodermal remnants of tunica vasculosa lentis result in faulty development of the zonules.
History and Physical
In every case of ectopia lentis, a history of trauma should be ruled out. These patients usually present with redness, pain, defective vision, monocular diplopia, and difficulty reading fine prints due to poor near vision secondary to loss of accommodation. A detailed systemic history is critical to rule out cardiac, skeletal neurological involvement, family history of consanguinity, and unexplained death at a young age due to syndromic features. All patients with ectopia lentis must undergo a detailed ophthalmic evaluation which includes an external ocular examination to rule out hereditary ocular malformations like enophthalmos, tall, long myopathic face as in Marfan's syndrome, white to white corneal diameter to check for megalocornea in Marfan's and squint evaluation to rule out amblyopia.[20]
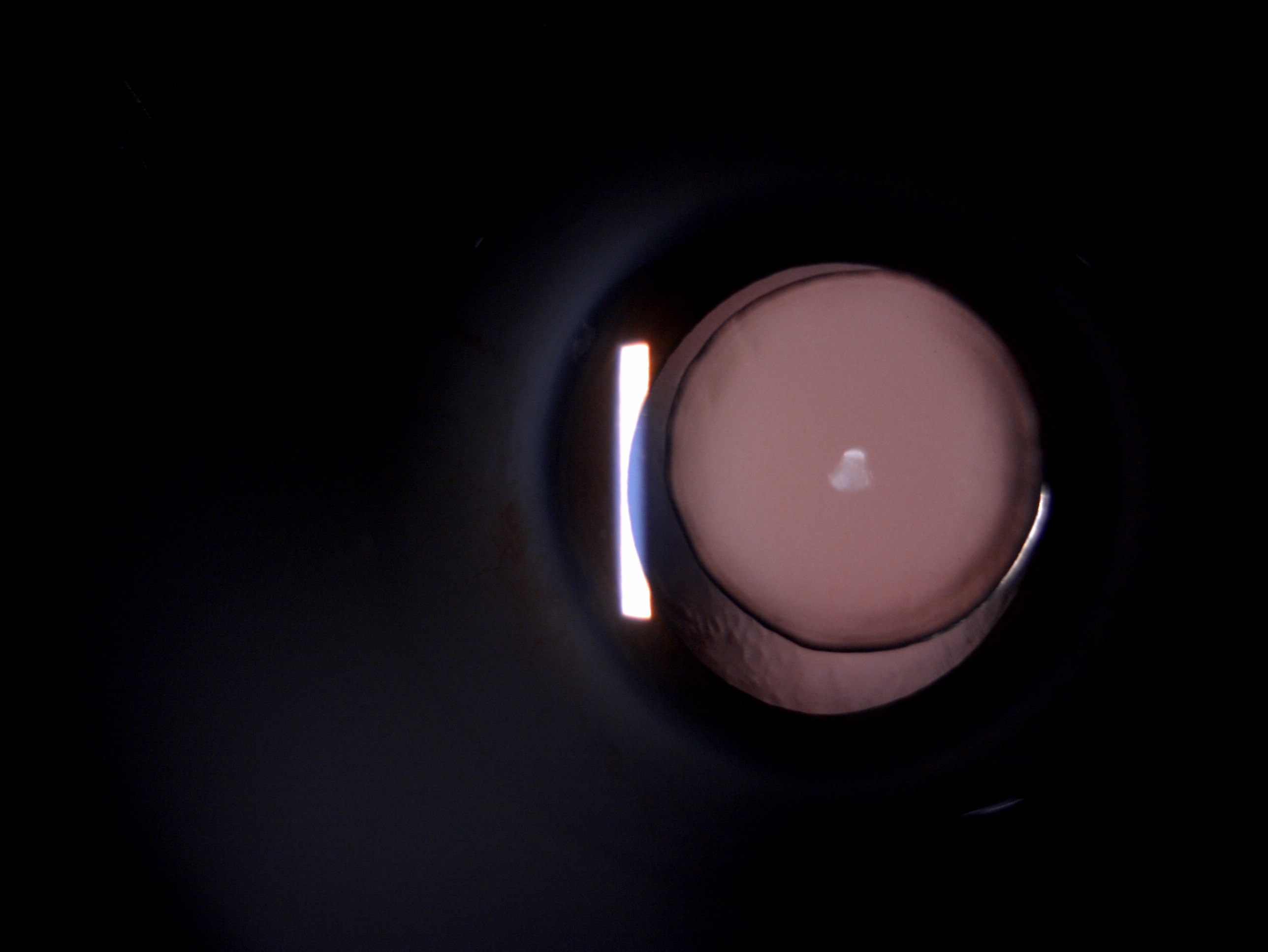
A detailed anterior segment examination to look for blue sclera, corneal diameter, cornea plana, corneal endothelial damage, anterior chamber depth, cells, flare, presence of dislocated lens, vitreous prolapse, presence or absence of peripheral anterior synechiae, iridodonesis, iris transillumination defects, pupillary margin and shape in case of ectopia lentis et pupillae, adequacy of the pupil to check for aphakic correction, cataractous changes in the lens, phacodonesis, appearance of zonules, subluxation or dislocation of the lens, aphakia, lens in the vitreous cavity or on the retinal surface, clear lens dislocated in the anterior chamber (oil droplet sign) and mature cataractous lens in the anterior chamber (white disc). A detailed dilated fundus examination to rule out pathological myopia, myopic macular degeneration, posterior vitreous detachment, lattice, holes, and retinal detachment.[21]
Evaluation
Visual Acuity
Thi8s examination is performed using a standardized Snellen visual acuity chart. The unaided, best-corrected, and pinhole visual acuity must be checked. Ectopia lentis results in severe vision loss, and it also rules out amblyopia. When planning a secondary IOL implantation, the +10 D correction should be checked in the aphakic eye.[22]
Refraction and Retinoscopy
It is essential to perform retinoscopy to ascertain the type of reflex: myopic, hypermetropic, clear, or dull. Refraction will help document the myopic and astigmatic correction needed while prescribing glasses.[23]
Keratometry
To know the amount of corneal astigmatism.[24]
Genetic Analysis
To rule out hereditary conditions associated with ectopia lentis.[25]
Systemic Evaluation
Cardiac- Auscultation, electrocardiogram, and 2D echocardiography to rule out aortic root dilatation, aneurysms of the aorta, and mitral valve prolapse in case of Marfan's syndrome.[26]
Musculoskeletal- Orthopaedic examination to rule out skeletal involvement in case of Marfan syndrome, homocystinuria, and Weill–Marchesani syndrome.
Lab Investigations
Serum and urine levels of homocysteine in case of homocystinuria.
A-Scan Ultrasonography
To rule out axial myopia in the case of Marfan syndrome.[27]
B Scan Ultrasonography
It is helpful to rule out retinal detachment, nucleus, or IOL drop in the vitreous cavity.[28]
Treatment / Management
Systemic Management
If a history of trauma is missing, all patients with ectopia lentis should be evaluated by a pediatrician to rule out a syndromic association. In patients with homocystinuria, dietary restrictions should be emphasized. In the case of Marfan's syndrome, repair of aortic aneurysm and mitral valve prolapse by a cardio surgeon can be lifesaving. Musculoskeletal problems also deserve attention with the help of a rheumatologist and orthopedist. Genetic screening and counseling of family members and evaluation of pedigree chart of family members.[10](B3)
Medical Management
It involved correction of refractive error by glass prescription or contact lenses. Timely intervention is needed to prevent irreversible amblyopia. Pharmacological dilatation with cycloplegics like 1% atropine or 2% homatropine is necessary in cases of dislocation of the lens in the anterior chamber. This will help in the posterior migration of the lens behind the iris. Antiglaucoma medication in the form of 1% timolol two times per day, acetazolamide 250 mg two times per day, or 0.1% brimonidine two per day to reduce intraocular pressure in cases of secondary glaucoma.[29](B3)
Refractive Correction
In ectopia lentis spectacles or contact lenses can be advised if the vision shows improvement well with refractive correction. Contact lens holds the advantage of less image magnification and better best-corrected visual acuity.[30]
Laser Peripheral Iridotomy
Pupillary block glaucoma can be a complication of ectopia lentis, and laser peripheral iridotomy is the treatment of choice in such cases. Prophylactic laser iridotomy is also indicated in patients with microspherophakia.[31]
Surgical Management
Indications for Surgery
- Lens induced glaucoma
- The dislocated lens in the anterior chamber with corneal endothelial touch
- Mature or Morgagnian cataract
- Lens induced uveitis
- Visual acuity not improving with refractive correction
- Retinal detachment
- A subluxated or dislocated lens in the vitreous cavity[32]
Surgical Techniques for Ectopia Lentis
- Pars plana vitrectomy with lensectomy
- Cataract extraction with anterior vitrectomy
- Anterior chamber IOL
- Iris claw or iris sutured IOL
- Scleral fixated IOL
- Posterior chamber IOL with capsular tension ring or capsular tension segment
- Femtosecond laser for subluxated lens management
- Optical iridectomy[33] (B2)
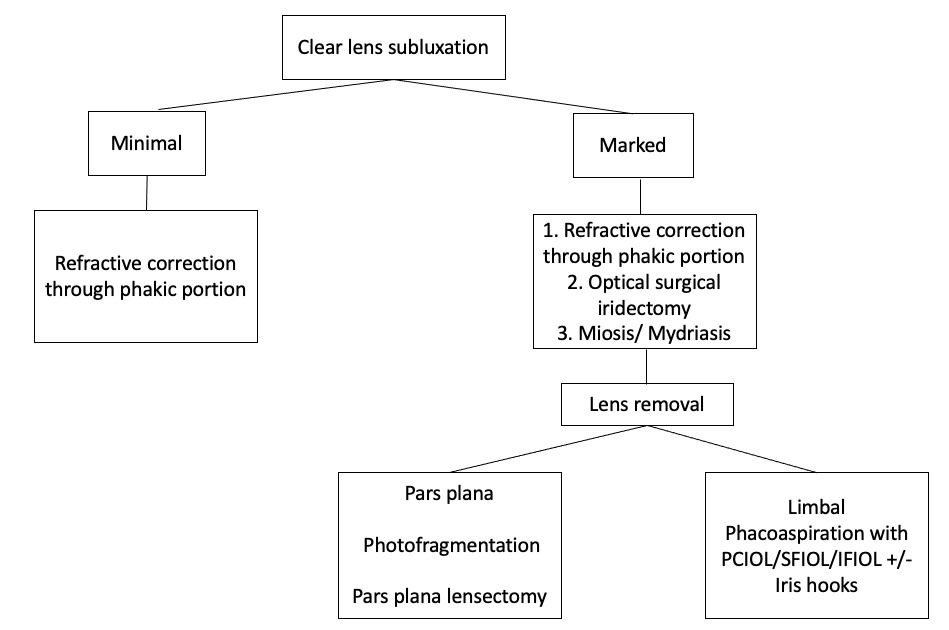
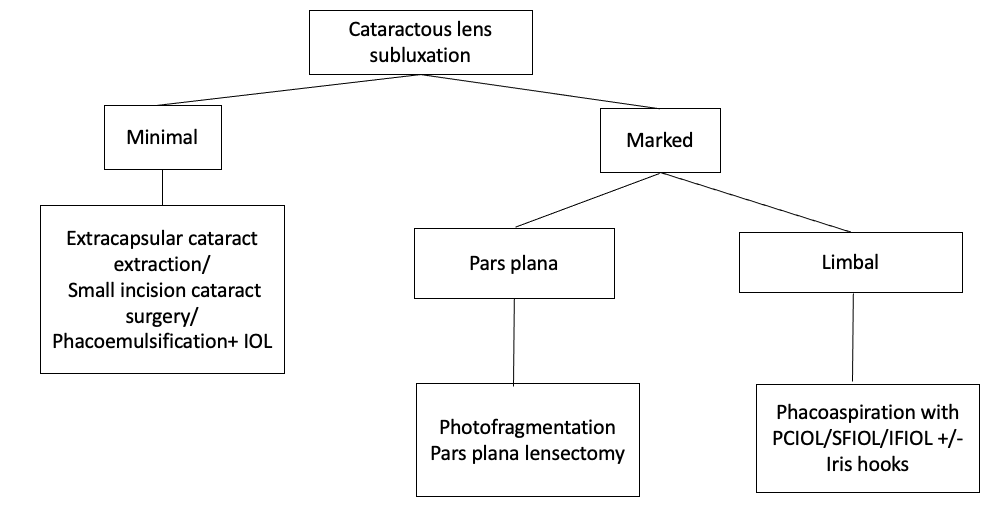
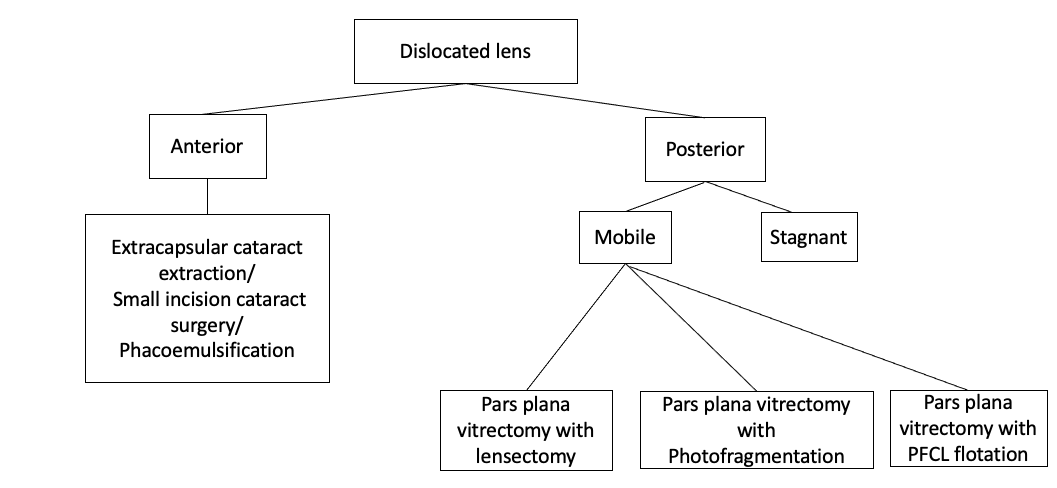
A detailed management algorithm for the subluxated clear lens, subluxated cataractous lens, and the dislocated lens are described in Figures 2, 3, and 4, respectively.
Differential Diagnosis
Pertinent Studies and Ongoing Trials
Chen et al. studied spherical aberration in Chinese families with ectopia lentis and concluded that spherical corneal aberrations were low in patients with Marfan's s syndrome.[37] Puthalath et al. reported a rare presentation of ectopia lentis with congenital aniridia and unilateral buphthalmos.[38] Muthukumar et al. did a comparative analysis of iris-claw lenses versus scleral fixated lenses in patients with ectopia lentis. They concluded that both are viable options to safeguard vision in pediatric aphakia cases secondary to ectopia lentis.[39]
Prognosis
The patient's prognosis depends on the presenting visual acuity, the extent of ocular and systemic involvement, degree of subluxation of the lens, age of onset of ectopia lentis, and associated systemic complications. Traumatic ectopia lentis patients usually have a very poor visual outcome. Large-scale studies are still pending in the literature to assess the visual outcome and prognosis of ectopia lentis cases. As per previous studies, the majority of ectopia lentis cases achieve a best-corrected visual acuity of 6/12 or better.[8]
Complications
- Amblyopia
- Corneal endothelial damage
- Corneal decompensation
- Chronic iridocyclitis
- Pupillary block glaucoma
- Phacoanaphylactic glaucoma
- Angle recession glaucoma
- Subluxated lens
- Dislocated lens
- Retinal detachment
Postoperative and Rehabilitation Care
All patients of ectopia lentis who have undergone surgical correction in the form of lens extraction and primary or secondary IOL implantation should be meticulously evaluated in detail postoperatively. A detailed anterior segment evaluation to look for IOL position and presence or absence of vitreous prolapse and a thorough fundus evaluation to rule out retinal detachment as these patients are at high risk of retinal detachment.
All patients should be started on topical antibiotic and steroid combination in the form of 0.1% dexamethasone and 0.5% moxifloxacin or 0.5% gatifloxacin in tapering doses 6/5/4/3/2/1 per week. Some surgeons prefer to add a separate antibiotic like 0.5% moxifloxacin or gatifloxacin four times per day for 15 days to prevent secondary bacterial infection.
The patient should be followed-up on days 1, 30, and 90 days to rule out any postoperative complications. The patient should be counseled regarding the long-term outcomes of ectopia lentis and the importance of regular follow-up and postoperative drug use.[40]
Consultations
The ophthalmologists should meticulously evaluate any patient presenting to the outpatient department with suspected ectopia lentis. If the diagnosis is in doubt and an expert opinion is mandated, the patient should be referred to the cataract and IOL specialist for a higher opinion. If the patient develops secondary glaucoma, it should be managed with the help of glaucoma specialists.
In the case of corneal complications like corneal decompensation and megalocornea, the cornea specialist plays a crucial role in managing these cases. If the patient has pathological myopia, lattice retinal degeneration, or retinal detachment, the vitreoretinal surgeon help in managing these cases. Last but not least, all cases of ectopia lentis need a detailed systemic evaluation with the help of an internist. The cardiologist, rheumatologist, orthopedics, pediatrician, microbiologist, pathologist, and genetic specialist also have a crucial role in arriving at a final systemic diagnosis.[41]
Deterrence and Patient Education
All patients of ectopia lentis require detailed counseling regarding the pathology, long-term visual outcome, and prognosis of the condition. The importance of regular follow-up and post-operative medication use should be emphasized. The patient should also understand the complications associated with ectopia lentis. The importance of family screening, genetic counseling, and treatment of family members must be made clear to the patient. The patient should receive information regarding the familial pedigree chart and the role of consanguineous marriages in familial ectopia lentis.[42]
Pearls and Other Issues
To conclude, ectopia lentis is a rate familial or acquired displacement of crystalline lens from the patellar fossa. The subluxated or dislocated lens can be seen in the anterior chamber or posterior vitreous cavity. The patient can present with defective vision, loss of accommodation, monocular diplopia, pain, and redness. A detailed anterior segment, posterior segment, and systemic evaluation are necessary in each case. The management depends on the age of onset, visual acuity, the extent of subluxation or dislocation of the lens, and the presence of associated ocular and systemic complications. All patients should undergo a familial screening of ectopia lentis to rule out syndromic associations.[43]
Enhancing Healthcare Team Outcomes
Ectopia lentis is a familial or acquired displacement of crystalline lens which requires an interprofessional approach for meticulous management. The ophthalmologist, pediatrician, cardiologist, orthopedics, rheumatologist, microbiologist, and pathologist play a key role in managing these cases. The nursing team also plays a crucial role in the operating room and outpatient counseling regarding the long-term visual outcome and prognosis of ectopia lentis. They also emphasize the need for a meticulous follow-up and regular post-operative medications. The pharmacist plays a vital role in arranging the post-operative topical and systemic medications. Hence, an interprofessional, multidisciplinary team approach is warranted to achieve a perfect visual outcome in ectopia lentis cases.[44]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Sadiq MA, Vanderveen D. Genetics of ectopia lentis. Seminars in ophthalmology. 2013 Sep-Nov:28(5-6):313-20. doi: 10.3109/08820538.2013.825276. Epub [PubMed PMID: 24138040]
Chandra A, Charteris D. Molecular pathogenesis and management strategies of ectopia lentis. Eye (London, England). 2014 Feb:28(2):162-8. doi: 10.1038/eye.2013.274. Epub 2014 Jan 10 [PubMed PMID: 24406422]
Hsu HY, Edelstein SL, Lind JT. Surgical management of non-traumatic pediatric ectopia lentis: A case series and review of the literature. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2012 Jul:26(3):315-21. doi: 10.1016/j.sjopt.2012.05.001. Epub 2012 May 17 [PubMed PMID: 23961012]
Level 2 (mid-level) evidenceGoldberg MF. Clinical manifestations of ectopia lentis et pupillae in 16 patients. Ophthalmology. 1988 Aug:95(8):1080-7 [PubMed PMID: 3266004]
Level 3 (low-level) evidenceJin GM, Fan M, Cao QZ, Lin JX, Zhang YC, Lin JQ, Wang YY, Young CA, Zheng DY. Trends and characteristics of congenital ectopia lentis in China. International journal of ophthalmology. 2018:11(9):1545-1549. doi: 10.18240/ijo.2018.09.19. Epub 2018 Sep 18 [PubMed PMID: 30225232]
Masoud MT, Huda SN, Saboor T. Ectopia lentis caused by blunt eye trauma. British journal of hospital medicine (London, England : 2005). 2007 Mar:68(3):161 [PubMed PMID: 17419473]
Level 3 (low-level) evidenceChandra A, Aragon-Martin JA, Hughes K, Gati S, Reddy MA, Deshpande C, Cormack G, Child AH, Charteris DG, Arno G. A genotype-phenotype comparison of ADAMTSL4 and FBN1 in isolated ectopia lentis. Investigative ophthalmology & visual science. 2012 Jul 24:53(8):4889-96. doi: 10.1167/iovs.12-9874. Epub 2012 Jul 24 [PubMed PMID: 22736615]
Level 2 (mid-level) evidenceNelson LB, Maumenee IH. Ectopia lentis. Survey of ophthalmology. 1982 Nov-Dec:27(3):143-60 [PubMed PMID: 6984233]
Level 3 (low-level) evidenceSafi M, Nejad SK, O'Hara M, Shankar SP. Ectopia Lentis et Pupillae Caused by ADAMTSL4 Pathogenic Variants and an Algorithm for Work-up. Journal of pediatric ophthalmology and strabismus. 2019 Jul 5:56():e45-e48. doi: 10.3928/01913913-20190509-01. Epub 2019 Jul 5 [PubMed PMID: 31282960]
Judge DP, Dietz HC. Marfan's syndrome. Lancet (London, England). 2005 Dec 3:366(9501):1965-76 [PubMed PMID: 16325700]
Level 3 (low-level) evidenceRodrigo BJ, Paulina LL, Francesc Mde R, Eduardo TT, Alejandro N. Intraocular lens subluxation in marfan syndrome. The open ophthalmology journal. 2014:8():48-50. doi: 10.2174/1874364101408010048. Epub 2014 Sep 19 [PubMed PMID: 25279020]
Brown OR, DeMots H, Kloster FE, Roberts A, Menashe VD, Beals RK. Aortic root dilatation and mitral valve prolapse in Marfan's syndrome: an ECHOCARDIOgraphic study. Circulation. 1975 Oct:52(4):651-7 [PubMed PMID: 1157278]
Salik I, Rawla P. Marfan Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 30726024]
Yang GY, Huang X, Chen BJ, Xu ZP. Weill-Marchesani-like syndrome caused by an FBN1 mutation with low-penetrance. Chinese medical journal. 2021 Mar 23:134(11):1359-1361. doi: 10.1097/CM9.0000000000001406. Epub 2021 Mar 23 [PubMed PMID: 34075901]
Neely DE, Plager DA. Management of ectopia lentis in children. Ophthalmology clinics of North America. 2001 Sep:14(3):493-9 [PubMed PMID: 11705149]
Wasim M, Khan HN, Ayesha H, Iqbal M, Tawab A, Irfan M, Kanhai W, Goorden SMI, Stroomer L, Salomons G, Vaz FM, Karnebeek CDMV, Awan FR. Identification of three novel pathogenic mutations in cystathionine beta-synthase gene of Pakistani intellectually disabled patients. Journal of pediatric endocrinology & metabolism : JPEM. 2022 Mar 28:35(3):325-332. doi: 10.1515/jpem-2021-0508. Epub 2021 Dec 14 [PubMed PMID: 34905667]
Sakai LY, Keene DR, Renard M, De Backer J. FBN1: The disease-causing gene for Marfan syndrome and other genetic disorders. Gene. 2016 Oct 10:591(1):279-291. doi: 10.1016/j.gene.2016.07.033. Epub 2016 Jul 18 [PubMed PMID: 27437668]
Jones W, Rodriguez J, Bassnett S. Targeted deletion of fibrillin-1 in the mouse eye results in ectopia lentis and other ocular phenotypes associated with Marfan syndrome. Disease models & mechanisms. 2019 Jan 25:12(1):. doi: 10.1242/dmm.037283. Epub 2019 Jan 25 [PubMed PMID: 30642872]
Ahram D, Sato TS, Kohilan A, Tayeh M, Chen S, Leal S, Al-Salem M, El-Shanti H. A homozygous mutation in ADAMTSL4 causes autosomal-recessive isolated ectopia lentis. American journal of human genetics. 2009 Feb:84(2):274-8. doi: 10.1016/j.ajhg.2009.01.007. Epub 2009 Feb 5 [PubMed PMID: 19200529]
Chen T, Chen J, Jin G, Zhang M, Chen Z, Zheng D, Jiang Y. Clinical Ocular Diagnostic Model of Marfan Syndrome in Patients With Congenital Ectopia Lentis by Pentacam AXL System. Translational vision science & technology. 2021 Jun 1:10(7):3. doi: 10.1167/tvst.10.7.3. Epub [PubMed PMID: 34061947]
Wilczyński TK, Niewiem A, Leszczyński R, Michalska-Małecka K. Recurrent Intraocular Lens Dislocation in a Patient with Familial Ectopia Lentis. International journal of environmental research and public health. 2021 Apr 25:18(9):. doi: 10.3390/ijerph18094545. Epub 2021 Apr 25 [PubMed PMID: 33922930]
Rezar-Dreindl S, Stifter E, Neumayer T, Papp A, Gschliesser A, Schmidt-Erfurth U. Visual outcome and surgical results in children with Marfan syndrome. Clinical & experimental ophthalmology. 2019 Dec:47(9):1138-1145. doi: 10.1111/ceo.13596. Epub 2019 Aug 2 [PubMed PMID: 31325202]
Lian Z, Cao Q, Qi H, Young CA, Zhang X, Jin G, Zheng D. Accuracy of intraocular lens power formulas for eyes with scleral-sutured intraocular lenses in congenital ectopia lentis. Journal of cataract and refractive surgery. 2022 Apr 1:48(4):469-474. doi: 10.1097/j.jcrs.0000000000000874. Epub [PubMed PMID: 34978783]
Level 2 (mid-level) evidenceGehle P, Goergen B, Pilger D, Ruokonen P, Robinson PN, Salchow DJ. Biometric and structural ocular manifestations of Marfan syndrome. PloS one. 2017:12(9):e0183370. doi: 10.1371/journal.pone.0183370. Epub 2017 Sep 20 [PubMed PMID: 28931008]
Nistri S, De Cario R, Sticchi E, Spaziani G, Della Monica M, Giglio S, Favilli S, Giusti B, Stefano P, Pepe G. Differential Diagnosis between Marfan Syndrome and Loeys-Dietz Syndrome Type 4: A Novel Chromosomal Deletion Covering TGFB2. Genes. 2021 Sep 22:12(10):. doi: 10.3390/genes12101462. Epub 2021 Sep 22 [PubMed PMID: 34680857]
De Backer J. Cardiovascular characteristics in Marfan syndrome and their relation to the genotype. Verhandelingen - Koninklijke Academie voor Geneeskunde van Belgie. 2009:71(6):335-71 [PubMed PMID: 20232788]
Mansour AM, Younis MH, Dakroub RH. Anterior segment imaging and treatment of a case with syndrome of ectopia lentis, spontaneous filtering blebs, and craniofacial dysmorphism. Case reports in ophthalmology. 2013 Jan:4(1):84-90. doi: 10.1159/000350951. Epub 2013 Apr 25 [PubMed PMID: 23687502]
Level 3 (low-level) evidenceJin C, Wang Q, Li J, Zhu Y, Shentu X, Yao K. A recurrent PAX6 mutation is associated with aniridia and congenital progressive cataract in a Chinese family. Molecular vision. 2012:18():465-70 [PubMed PMID: 22393272]
Avalos-Lara SJ, Antonio-Aguirre B, Perez-Ortiz AC, Mendoza Velásquez C, Camacho-Ordoñez A, Palacio Pastrana C. Spherophakia and Ectopia Lentis in a Sturge-Weber Patient: A Case Report. Case reports in ophthalmology. 2020 May-Aug:11(2):356-363. doi: 10.1159/000508064. Epub 2020 Jul 14 [PubMed PMID: 32884550]
Level 3 (low-level) evidenceLalramhluni R, Rath S, Shrivastav A, Singh PK, Mayor R, Singh S. Refractive and Visual Outcomes after Scleral Fixated Intraocular Lens Implantation in Children with Ectopia Lentis. Nepalese journal of ophthalmology : a biannual peer-reviewed academic journal of the Nepal Ophthalmic Society : NEPJOPH. 2020 Jan:12(23):75-82. doi: 10.3126/nepjoph.v12i1.22252. Epub [PubMed PMID: 32799242]
Şimşek T, Beyazyıldız E, Şimşek E, Öztürk F. Isolated Microspherophakia Presenting with Angle-Closure Glaucoma. Turkish journal of ophthalmology. 2016 Oct:46(5):237-240. doi: 10.4274/tjo.47135. Epub 2016 Oct 17 [PubMed PMID: 28058167]
Erdogan G, Kandemir Besek N, Onal Gunay B, Agca A. Outcomes of three surgical approaches for managing ectopia lentis in Marfan syndrome. European journal of ophthalmology. 2022 Jan:32(1):242-248. doi: 10.1177/1120672121992950. Epub 2021 Feb 7 [PubMed PMID: 33550842]
Kazemi S, Wirostko WJ, Sinha S, Mieler WF, Koenig SB, Sheth BP. Combined pars plana lensectomy-vitrectomy with open-loop flexible anterior chamber intraocular lens (AC IOL) implantation for subluxated lenses. Transactions of the American Ophthalmological Society. 2000:98():247-51; discussion 251-3 [PubMed PMID: 11190027]
Level 2 (mid-level) evidenceGurnani B, Kaur K, Sekaran S. First case of coloboma, lens neovascularization, traumatic cataract, and retinal detachment in a young Asian female. Clinical case reports. 2021 Sep:9(9):e04743. doi: 10.1002/ccr3.4743. Epub 2021 Aug 30 [PubMed PMID: 34484773]
Level 3 (low-level) evidenceGurnani B, Kaur K, Gireesh P. A rare presentation of anterior dislocation of calcified capsular bag in a spontaneously absorbed cataractous eye. Oman journal of ophthalmology. 2021 May-Aug:14(2):120-121. doi: 10.4103/ojo.OJO_65_2019. Epub 2021 Jun 28 [PubMed PMID: 34345149]
Gurnani B, Kaur K. Rare traumatic anterior dislocation of capsular tension ring-intraocular lens complex in-toto. Indian journal of ophthalmology. 2020 Nov:68(11):2529. doi: 10.4103/ijo.IJO_807_20. Epub [PubMed PMID: 33120674]
Chen J, Tang Y, Jing Q, Lu Y, Jiang Y. Analysis of Corneal Spherical Aberrations in Chinese Bilateral Ectopia Lentis Patients. Frontiers in medicine. 2021:8():736686. doi: 10.3389/fmed.2021.736686. Epub 2021 Nov 19 [PubMed PMID: 34869429]
Puthalath AS, Gupta N, Samanta R, Verma PK. Congenital aniridia with ectopia lentis and unilateral buphthalmos: an unusual presentation. BMJ case reports. 2021 Aug 17:14(8):. doi: 10.1136/bcr-2021-244000. Epub 2021 Aug 17 [PubMed PMID: 34404663]
Level 3 (low-level) evidenceMuthukumar B, Chhablani PP, Salman A, Bhandari V, Kapoor R. Comparison of retropupillary fixated iris claw lens versus sclera fixated lens for correction of pediatric aphakia secondary to ectopia lentis. Oman journal of ophthalmology. 2021 Jan-Apr:14(1):20-26. doi: 10.4103/ojo.OJO_91_2020. Epub 2021 Feb 27 [PubMed PMID: 34084030]
Esfandiari H, Ansari S, Mohammad-Rabei H, Mets MB. Management Strategies of Ocular Abnormalities in Patients with Marfan Syndrome: Current Perspective. Journal of ophthalmic & vision research. 2019 Jan-Mar:14(1):71-77. doi: 10.4103/jovr.jovr_29_18. Epub [PubMed PMID: 30820290]
Level 3 (low-level) evidenceHoffman RS, Snyder ME, Devgan U, Allen QB, Yeoh R, Braga-Mele R, ASCRS Cataract Clinical Committee, Challenging/Complicated Cataract Surgery Subcommittee. Management of the subluxated crystalline lens. Journal of cataract and refractive surgery. 2013 Dec:39(12):1904-15. doi: 10.1016/j.jcrs.2013.09.005. Epub [PubMed PMID: 24286841]
Wu-Chen WY, Letson RD, Summers CG. Functional and structural outcomes following lensectomy for ectopia lentis. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2005 Aug:9(4):353-7 [PubMed PMID: 16102486]
Level 2 (mid-level) evidenceDuan Y, Li P, Ding T, Wang Y, Liao Y, Du Z, Ling J, Liu S, Li W, Liu Z. Combining clinical examination with exome sequencing for the diagnosis and treatment of Marfan syndrome: a case series of 6 families from China. Annals of palliative medicine. 2021 Sep:10(9):9953-9962. doi: 10.21037/apm-21-2305. Epub [PubMed PMID: 34628919]
Level 2 (mid-level) evidenceChee SP, Ti SE, Chan NS. Management of the subluxated crystalline lens: A review. Clinical & experimental ophthalmology. 2021 Dec:49(9):1091-1101. doi: 10.1111/ceo.13975. Epub 2021 Jul 29 [PubMed PMID: 34264007]