Introduction
Optic nerve drusen are refractive, calcified nodules located within the optic disc, the most anterior part of the optic nerve. The optic disc is visible in the retina on indirect fundoscopy. Anatomically, optic nerve drusen are located just anterior to the lamina cribrosa and are most commonly seen in the nasal part of the disc.[1]
These largely acellular calcifications, usually detected incidentally on an exam, may progress and become more visible during earlier decades of life but rarely change significantly over a patient's lifetime and are generally asymptomatic.[2] Although most are asymptomatic, optic nerve drusen have been associated with visual field defects, anterior ischemic optic neuropathy, transient visual obscurations, and more rare complications.[3]
Superficial drusen can be diagnosed clinically; however, deeper or buried drusen may give the appearance of a swollen disc or edema (i.e., papilledema or bilateral disc swelling secondary to increased intracranial pressure) and require further evaluation and testing to confirm the diagnosis.[4] Despite their different locations, superficial and deep drusen represent the same pathology.[5]
While drusen may give the appearance of disc edema or swelling, or pseudo papilledema, the presence of drusen does not exclude the presence of actual edema. For example, there is a high prevalence of nerve drusen in young patients with idiopathic intracranial hypertension.[6] Although no pattern of inheritance has been fully elucidated, autosomal dominant inherence with incomplete penetrance is the leading suspicion.[7]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology of optic nerve drusen is considered secondary to the slowing of axoplasmic flow from blood supply compromise of the optic disc. This stasis in the axoplasmic flow then leads to the accumulation of calcified and degenerated mitochondria that create a nidus for nerve drusen to form. Compromise of axoplasmic flow has been theorized to be related to various factors, including an inherited dysplasia of the optic nerve head, errors in transcellular mitophagy, and small scleral canals.[2]
Epidemiology
The prevalence of optic nerve drusen is estimated to be 3.4 to 24 per 1000, equally affecting males and females and Caucasians more than other ethnicities.[8]
History and Physical
Typically, patients are asymptomatic, and the drusen are noticed incidentally on examination. However, up to 10% of patients may report transient visual obscurations, and up to 25% may present with visual field defects, including enlarged blind spots.
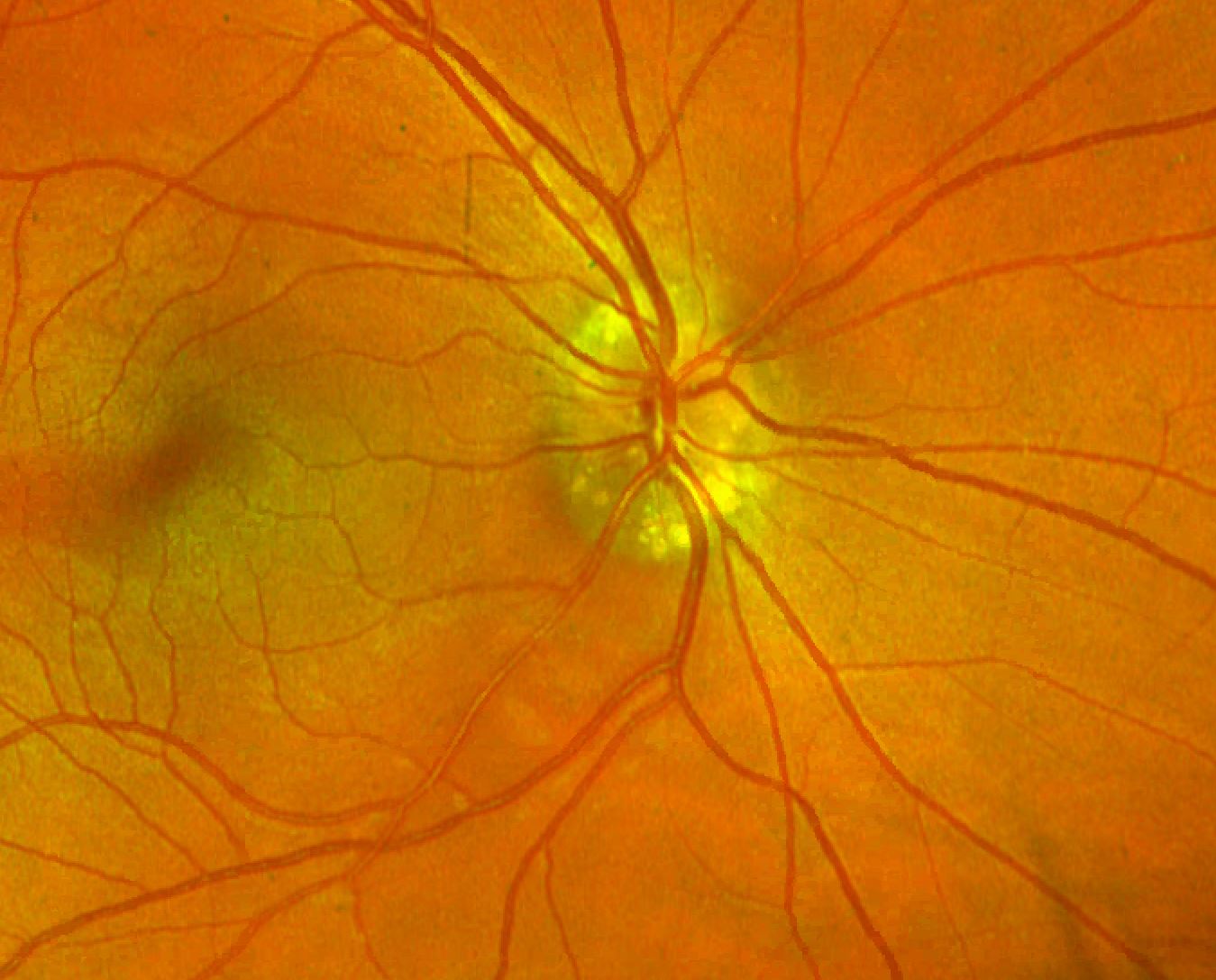
On physical exam, superficial drusen can be seen without the aid of imaging modalities. The nerve is classically described as having a "lumpy, bumpy" appearance. The drusen appear as round, refractile bodies which may be yellow or white in color and located on the surface of or buried under the nerve. Drusen are most commonly located on the nasal aspect of the disc. Additionally, if there is asymmetric nerve involvement, patients may have an afferent pupillary defect. Spontaneous venous pulsations and tortuous or anomalous vessel branching and caliber can be seen.
In some cases, the irregular border of the nerve secondary to drusen may give the appearance of edema, creating diagnostic confusion. Clinically, true edema from pseudo edema can be distinguished based on the appearance of the nerve. Particular attention should be paid to the disc microvasculature as there will often be peripapillary flame hemorrhages and a reddish hue of the disc in cases of true disc edema. Additionally, in true edema, both retinal vessels and vessels at the disc margin may be obscured, while vessels are clearly visible in pseudo edema. In borderline situations and cases of suspected deeper drusen, further investigation is warranted through other imaging modalities to confirm the presence of drusen.[9]
Evaluation
If the diagnosis remains unclear on physical exam, further investigation is warranted to confirm the diagnosis and rule out disc edema. Imaging modalities include B-Scan ultrasonography, CT scan, fluorescein angiography, fundus autofluorescence, and optical coherence tomography (OCT).
For both superficial and deep drusen, ultrasound may demonstrate a highly echogenic focus at the disc, representing calcification.[10] CT has utility in showing calcified drusen; however, it can not detect noncalcified drusen. Fluorescein angiography was classically utilized to distinguish true disc edema from buried nerve drusen; however, data reveals variability in the effectiveness of fluorescein angiography in detecting optic nerve drusen, especially in borderline cases.[11]
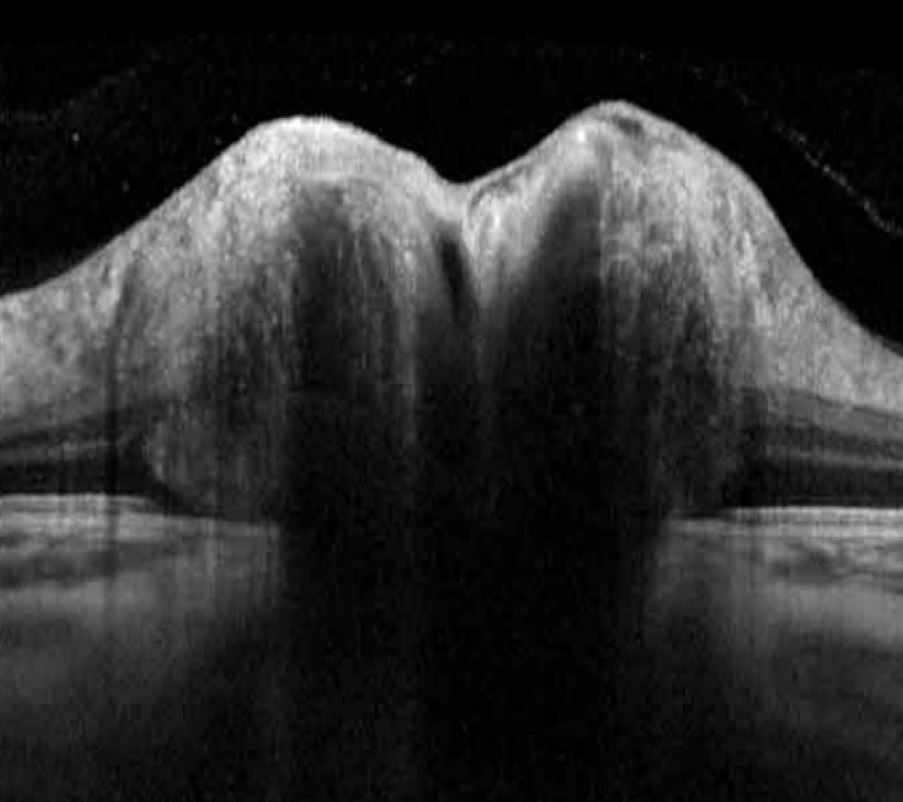
Fundus autofluorescence will demonstrate optic nerve drusen as bright hyperfluorescent foci in the disc, revealing all visible and most buried drusen.[12] OCT will reveal nerve drusen as areas of irregular or spherical hyporeflective cores with a uniform internal structure and hyperreflective borders at the surface.[13]
While ultrasound and OCT provide excellent mechanisms to identify nerve drusen, OCT with enhanced depth imaging provides superior visualization, with one study revealing a 100% detection rate of buried drusen compared to 82% by non-EDI OCT and 41% by ultrasound.[14]
In addition to detecting the presence of nerve drusen, certain imaging modalities can assist the physician in assessing possible complications and effects of the drusen. For example, OCT can help track nerve fiber thinning that can predict visual field loss.[15]
Treatment / Management
Optic nerve drusen on their own do not necessitate treatment. Typically, patients have a good visual prognosis, and drusen can be re-evaluated periodically. There is no strong evidence for initiating treatment for those individuals without visual field loss, although treatment with IOP lowering therapy or optic nerve sheath fenestration has been undertaken in some cases. Additionally, there are no established surgical interventions for removing optic nerve drusen. Surgical excision and radial optic neurotomy have been attempted without evidence to back their utilization. On the contrary surgical excision has been shown to have negative consequences.[16] (B3)
Complications associated with optic nerve drusen may require treatment. Choroidal neovascularization occurring in association with the presence of nerve drusen, though rare, may lead to complications such as central retinal vein occlusion or ischemic optic neuropathy. These entities are treated with intravitreal injections of anti-VEGF medication, laser photocoagulation, and photodynamic therapy.[17](B3)
Differential Diagnosis
A critical differential to rule out is actual disc edema or papilledema (bilateral disc edema). Imaging modalities can help make this distinction. It is also important to remember that real edema can be present in addition to nerve drusen. OCT will reveal NFL thickening in cases of the presence of disc edema.
Fluorescein angiography will reveal early diffuse hyperfluorescence with late leakage on and near the disc in cases of edema. On B-scan, calcified drusen maintain signal intensity despite a decrease in the gain setting, while in cases of true edema, the signal intensity decreases as the gain decreases.[18]
Pseudopapilledema from other etiologies such as congenital anomalies, infiltrative lesions, vitreopapillary traction, and genetic disease such as Lebers hereditary optic neuropathy are other important differentials to keep in mind. History and the greater clinical picture, in addition to imaging modalities, can assist the physician in distinguishing between these entities.
Other differentials include peripapillary hyperreflective ovoid mass-like structures (PHOMS), tilted discs, myelinated nerve fiber layer, crowded discs, and idiopathic intracranial hypertension. In the case of idiopathic intracranial hypertension, certain characteristic imaging findings on MRI can aid in diagnoses such as flattening of the posterior globe, kinking of optic nerves, empty sella, tonsillar ectopia, slit-like ventricles, and other findings. Lumbar puncture is another key tool in diagnosing idiopathic intracranial hypertension.[19]
Prognosis
Typically overall visual morbidity is minimal. Nerve drusen can be followed periodically and do not typically cause visual acuity loss. However, visual field loss is more common, with some estimates stating as many as 50% of children and nearly 90% of adults may have visual field defects, most commonly enlarged blind spots and peripheral constriction, or less commonly arcuate defects. More severe visual morbidity may arise from rare complications associated with nerve drusen, such as ischemic optic neuropathy.[20]
As patients become older, the nerve drusen likely will become more visible clinically. There is a greater likelihood of visual field defects; however, this increase in visibility and visual field defect probability tends to stabilize in adulthood. The presence of visual field defects is significantly more common than the presence of practical visual symptoms.[21]
Complications
Although rare, complications do exist with optic nerve drusen. Complications include anterior ischemic optic neuropathy, retinal vascular occlusions, choroidal neovascular membranes, and flame disc hemorrhages.
Deterrence and Patient Education
Patients should be educated that they will likely not experience visual symptoms in the presence of nerve drusen. However, they are highly likely to develop some visual field defects detectable on visual field testing. Education should also be given that despite the benign nature of nerve drusen, imaging is warranted in general and especially in borderline cases to confirm no presence of disc edema.
Patients should also be educated that there are rarely associated complications possible and that treatment and prognosis of complications depend on the nature of the complication. Lastly, patients should understand that treatment options targeting nerve drusen are not widely available or well studied.
Enhancing Healthcare Team Outcomes
Optic nerve drusen are typically benign findings discovered on routine examinations. While superficial drusen may be diagnosed clinically, buried or deeper nerve drusen may present diagnostic uncertainty and require work up to establish and confirm the diagnosis. Imaging modalities such as ultrasound, fundus autofluorescence, and OCT with enhanced depth imaging represent premier techniques in confirming the diagnosis.
In addition to confirming the diagnosis, it is critical to rule out the concurrent presence of edema. This can be done in part through the same imaging modalities used to diagnose nerve drusen.
Patients must understand that although nerve drusen are usually not vision-threatening, they can cause visual field defects and have been associated with rare, potentially visually devastating complications such as anterior ischemic optic neuropathy and retinal vascular occlusions.
It is important to refer patients suspected of having nerve drusen to an ophthalmologist for further evaluation and testing to confirm the diagnosis, the patient appropriately followed, disc edema ruled out, and complications managed should they arise. Due to the complexity of diagnosis and potentially devastating consequences of disc edema, consultation with ophthalmology should be done promptly by the healthcare professional in cases of suspected optic nerve drusen.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Friedman AH, Henkind P, Gartner S. Drusen of the optic disc. A histopathological study. Transactions of the ophthalmological societies of the United Kingdom. 1975 Apr:95(1):4-9 [PubMed PMID: 1064209]
Palmer E, Gale J, Crowston JG, Wells AP. Optic Nerve Head Drusen: An Update. Neuro-ophthalmology (Aeolus Press). 2018 Dec:42(6):367-384. doi: 10.1080/01658107.2018.1444060. Epub 2018 Apr 25 [PubMed PMID: 30524490]
Lee KM, Woo SJ, Hwang JM. Factors associated with visual field defects of optic disc drusen. PloS one. 2018:13(4):e0196001. doi: 10.1371/journal.pone.0196001. Epub 2018 Apr 30 [PubMed PMID: 29708976]
Guarnizo A,Albreiki D,Cruz JP,Létourneau-Guillon L,Iancu D,Torres C, Papilledema: A Review of the Pathophysiology, Imaging Findings, and Mimics. Canadian Association of Radiologists journal = Journal l'Association canadienne des radiologistes. 2022 Jan 19; [PubMed PMID: 35044276]
Flores-Rodríguez P, Gili P, Martín-Ríos MD. Ophthalmic features of optic disc drusen. Ophthalmologica. Journal international d'ophtalmologie. International journal of ophthalmology. Zeitschrift fur Augenheilkunde. 2012:228(1):59-66. doi: 10.1159/000337842. Epub 2012 May 12 [PubMed PMID: 22584542]
Genizi J, Meiselles D, Arnowitz E, Segal I, Cohen R, Goldenberg-Cohen N. Optic Nerve Drusen Is Highly Prevalent Among Children With Pseudotumor Cerebri Syndrome. Frontiers in neurology. 2021:12():789673. doi: 10.3389/fneur.2021.789673. Epub 2021 Dec 13 [PubMed PMID: 34966353]
Auw-Haedrich C, Staubach F, Witschel H. Optic disk drusen. Survey of ophthalmology. 2002 Nov-Dec:47(6):515-32 [PubMed PMID: 12504737]
Level 3 (low-level) evidenceAntcliff RJ, Spalton DJ. Are optic disc drusen inherited? Ophthalmology. 1999 Jul:106(7):1278-81 [PubMed PMID: 10406605]
Level 2 (mid-level) evidenceElbaz H, Schulz A, Ponto KA, Nickels S, Pfeiffer N, Mirshahi A, Peto T. Posterior segment eye lesions: prevalence and associations with ocular and systemic parameters: results from the Gutenberg Health Study. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2019 Oct:257(10):2127-2135. doi: 10.1007/s00417-019-04416-w. Epub 2019 Jul 18 [PubMed PMID: 31321522]
De La Hoz Polo M, Torramilans Lluís A, Pozuelo Segura O, Anguera Bosque A, Esmerado Appiani C, Caminal Mitjana JM. Ocular ultrasonography focused on the posterior eye segment: what radiologists should know. Insights into imaging. 2016 Jun:7(3):351-64. doi: 10.1007/s13244-016-0471-z. Epub 2016 Feb 24 [PubMed PMID: 26910565]
Pineles SL, Arnold AC. Fluorescein angiographic identification of optic disc drusen with and without optic disc edema. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2012 Mar:32(1):17-22. doi: 10.1097/WNO.0b013e31823010b8. Epub [PubMed PMID: 21926917]
Level 2 (mid-level) evidenceGili P, Flores-Rodríguez P, Yangüela J, Orduña-Azcona J, Martín-Ríos MD. Sensitivity and specificity of monochromatic photography of the ocular fundus in differentiating optic nerve head drusen and optic disc oedema: optic disc drusen and oedema. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2013 Mar:251(3):923-8. doi: 10.1007/s00417-012-2223-1. Epub 2012 Dec 5 [PubMed PMID: 23212800]
Silverman AL, Tatham AJ, Medeiros FA, Weinreb RN. Assessment of optic nerve head drusen using enhanced depth imaging and swept source optical coherence tomography. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2014 Jun:34(2):198-205. doi: 10.1097/WNO.0000000000000115. Epub [PubMed PMID: 24662838]
Merchant KY, Su D, Park SC, Qayum S, Banik R, Liebmann JM, Ritch R. Enhanced depth imaging optical coherence tomography of optic nerve head drusen. Ophthalmology. 2013 Jul:120(7):1409-14. doi: 10.1016/j.ophtha.2012.12.035. Epub 2013 Mar 24 [PubMed PMID: 23531353]
Level 2 (mid-level) evidenceOrtiz-Toquero S, Muñoz-Negrete FJ, Rebolleda G. Enhanced Depth Imaging Optical Coherence Tomography Technology Reveals a Significant Association Between Optic Nerve Drusen Anterior Displacement and Retinal Nerve Fiber Layer Thinning Over Time. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2021 Dec 1:41(4):e483-e489. doi: 10.1097/WNO.0000000000001103. Epub [PubMed PMID: 33110003]
Pfriem M, Hoerauf H. Unsuccessful surgical excision of optic nerve drusen. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2011 Oct:249(10):1583-5. doi: 10.1007/s00417-011-1693-x. Epub 2011 Jun 3 [PubMed PMID: 21638031]
Level 3 (low-level) evidenceChang MY, Pineles SL. Optic disk drusen in children. Survey of ophthalmology. 2016 Nov-Dec:61(6):745-758. doi: 10.1016/j.survophthal.2016.03.007. Epub 2016 Mar 29 [PubMed PMID: 27033945]
Level 3 (low-level) evidenceCostello F, Rothenbuehler SP, Sibony PA, Hamann S, Optic Disc Drusen Studies Consortium. Diagnosing Optic Disc Drusen in the Modern Imaging Era: A Practical Approach. Neuro-ophthalmology (Aeolus Press). 2021:45(1):1-16. doi: 10.1080/01658107.2020.1810286. Epub 2020 Oct 26 [PubMed PMID: 33762782]
Bontzos G, Smoustopoulos G, Detorakis TE. Unilateral optic disc drusen mis-diagnosed as optic neuritis: Diagnostic and therapeutic implications. Romanian journal of ophthalmology. 2020 Oct-Dec:64(4):449-454. doi: 10.22336/rjo.2020.69. Epub [PubMed PMID: 33367185]
Malmqvist L, Lund-Andersen H, Hamann S. Long-term evolution of superficial optic disc drusen. Acta ophthalmologica. 2017 Jun:95(4):352-356. doi: 10.1111/aos.13315. Epub 2016 Dec 20 [PubMed PMID: 27996202]
Zhang X, Cheng X, Chen B, Sun X. Multimodal Imaging Characteristics and Presumed Cause of Intrapapillary Hemorrhage with Adjacent Peripapillary Subretinal Hemorrhage. Clinical ophthalmology (Auckland, N.Z.). 2021:15():2583-2590. doi: 10.2147/OPTH.S304861. Epub 2021 Jun 18 [PubMed PMID: 34177259]