Fluoroscopic Percutaneous Coronary Interventions, Assessment, Protocols, and Interpretation
Fluoroscopic Percutaneous Coronary Interventions, Assessment, Protocols, and Interpretation
Introduction
Ischemic heart disease is the leading cause of death globally. Percutaneous coronary intervention (PCI) has played a vital role in managing obstructive coronary artery disease.[1] Nearly all percutaneous coronary intervention was carried out under fluoroscopic guidance by utilizing ionizing radiation. It is essential to take appropriate fluoroscopic views according to vessel anatomy during percutaneous coronary intervention so that the diseased segment should not be missed.[2][3][4]
The knowledge of appropriate views for percutaneous coronary intervention helps cover the diseased segment of the artery and reduces radiation exposure to both patients and healthcare workers by decreasing fluoroscopic time and radiation dose. In this chapter, we will discuss percutaneous coronary intervention under fluoroscopic guidance in detail.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The heart is Supplied by Three Major Coronary Arteries
- Left anterior descending with Septal and diagonal branches
- Left circumflex artery
- The right coronary artery bifurcates into the right posterior descending artery and right posterior left ventricular branch.
However, in a patient with a previous history of coronary artery bypass graft, grafts are placed distal to the narrowed segment of the coronary artery. The most commonly used vessels for grafts are saphenous vein graft, left internal mammary artery, right internal mammary artery, radial artery, gastroepiploic artery, and inferior epigastric artery. It is essential to know the site and number of grafts before the graft study.
Indications
2011, ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention
Indications of percutaneous coronary intervention to improve mortality:[5]
- In unprotected left main artery with ST-elevation myocardial infarction: If distal flow to vessel less than TIMI III and percutaneous coronary intervention can be done much quicker and safer than CABG (Class II-a)
- In unprotected left main artery with non-ST-elevation myocardial infarction or Unstable angina: If CABG can not be performed (Class II-a)
- In unprotected left main artery with stable ischemic heart disease: If two of the following present 1) LOW-risk PCI (Syntax<22) and ostial or trunk involvement 2) Increase risk of surgical adverse events ( STS score < 5 (Class II-a)
- In triple vessel coronary artery disease with or without Proximal LAD: (Class II-a)
- In two-vessel disease with proximal LAD: (Class II-b)
- In two-vessel disease without proximal LAD: (Class II-b)
- In one vessel disease with proximal LAD: (Class II-b)
- For patients with the survivor of sudden cardiac death with presumed ischemia-mediated ventricular tachycardia (Class I)
Indications of percutaneous coronary intervention to improve symptoms:
- Percutaneous coronary intervention in patients with persistent angina despite optimal medical management to improve symptoms with single or more significant (>70% diameter) coronary artery disease and amenable to revascularization. (Class I)
- Percutaneous coronary intervention in patients with persistent angina to improve symptoms with single or more significant (>70% diameter) coronary artery disease and medical management can not be given because of medication contraindication, adverse effects, or patient preferences. (Class II-a)
- Percutaneous coronary intervention in patients with persistent angina despite optimal medical management to improve symptoms with single or more significant (>70% diameter) coronary artery disease and associated with ischemia. (Class II-a)
Contraindications
The following are the contraindications of percutaneous coronary intervention
Absolute Contraindication
- Intolerance to dual antiplatelets
- Severe illness which reducing the lifespan to less than one year
Relative Contraindication
- Coronary artery vessel diameter < 2.5 mm
- Anatomy not feasible for coronary intervention
- Diffusely disease saphenous vein graft
Equipment
For fluoroscopic percutaneous coronary intervention, the following equipment is essential:
- Fluoroscopic machine
- Contrast agent
- Guide catheters
- Guide wires
- Coronary balloon
- Coronary stent
To prevent radiation exposure during the fluoroscopic guided percutaneous coronary intervention, each medical staff require protective measure during the procedure which includes:
- Lead apron
- Thyroid collar
- Radiation protective glasses
- Radiation monitoring badges
Personnel
- Intervention cardiologist
- Radiation technician
- Cath lab technician
- Staff nurse
Preparation
Informed consent should be taken before the procedure. It is essential to take a complete history and perform a physical examination pre-procedure to determine the indication of the procedure. The patient should be premedicated with antiplatelets.
Technique or Treatment
It is essential to know in which view a specific part of the artery will be visible while performing coronary angioplasty under fluoroscopic guidance.[6][7]
|
Vessels |
Fluoroscopic views |
Additional views |
|
Left Main Coronary Artery (LM) |
||
|
Ostial part of LM |
LAO (left anterior oblique) caudal |
AP (Anteroposterior) Caudal |
|
Mid part of LM |
RAO (Right anterior oblique)cranial RAO (Right anterior oblique)caudal |
AP (Anteroposterior) Caudal |
|
Distal part of LM |
LAO(left anterior oblique) caudal RAO (Right anterior oblique) caudal |
LAO(left anterior oblique) cranial |
|
Left Anterior Descending Artery (LAD) |
||
|
Ostial part of LAD |
LAO(left anterior oblique) caudal |
AP(Anteroposterior) Caudal RAO(Right anterior oblique) caudal |
|
Mid part of LAD |
RAO (Right anterior oblique) cranial LAO(left anterior oblique) cranial RAO (Right anterior oblique) caudal |
AP(Anteroposterior) Cranial |
|
Distal part of LAD |
RAO (Right anterior oblique) cranial |
LAO(left anterior oblique) cranial RAO (Right anterior oblique) caudal |
|
Left Circumflex Artery (LCX) |
||
|
Ostial part of LCX |
LAO(left anterior oblique) caudal |
AP(Anteroposterior) Caudal |
|
Mid part of LCX |
RAO (Right anterior oblique) LAO(left anterior oblique) |
LAO(left anterior oblique) cranial AP(Anteroposterior) Caudal |
|
Distal part of LCX |
RAO (Right anterior oblique) LAO(left anterior oblique) |
LAO(left anterior oblique) cranial |
|
Right Coronary Artery (RCA) |
||
|
Osteoproximal part of RCA |
LAO(left anterior oblique) |
AP(Anteroposterior) Caudal LAO(left anterior oblique) Caudal |
|
Mid part of RCA |
RAO (Right anterior oblique) |
LAO(left anterior oblique) |
|
The distal part of RCA at the level of bifurcation to RPDA(Right posterior descending artery) and RPLV (Right posterior left ventricular branch) |
LAO(left anterior oblique) Cranial
|
AP (Anteroposterior) Cranial |
|
RPDA |
RAO (Right anterior oblique)
|
AP (Anteroposterior) Cranial |
|
RPLV |
AP(Anteroposterior) Caudal |
|
|
Saphenous Vein-Graft to Coronary Artery |
||
|
Saphenous vein graft(SVG) to LAD |
AP (Anteroposterior) Cranial RAO (Right anterior oblique)cranial
|
Lateral |
|
Saphenous vein graft(SVG) to Left circumflex or Obtuse marginal artery |
RAO (Right anterior oblique) |
AP(Anteroposterior) Caudal |
|
Saphenous vein graft(SVG) to Right coronary artery |
LAO(left anterior oblique) |
LAO(left anterior oblique) Cranial
|
|
Left Internal Mammary Artery to LAD |
||
|
Osteoproximal part for Left internal mammary artery to LAD |
LAO(left anterior oblique) Cranial
|
|
|
Mid Part of LIMA |
RAO (Right anterior oblique) cranial |
|
|
The insertion site of LIMA to LAD |
Left Lateral (90 degrees) |
|
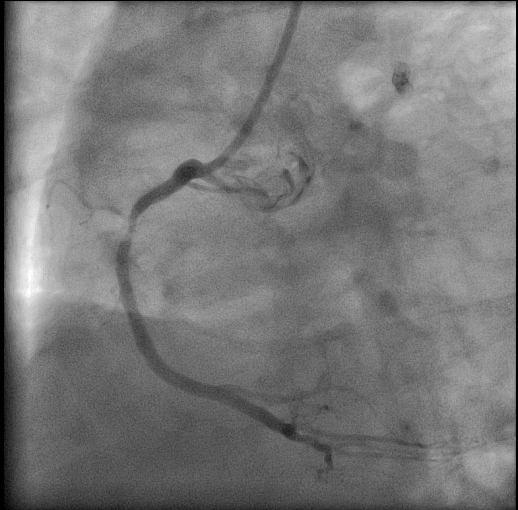
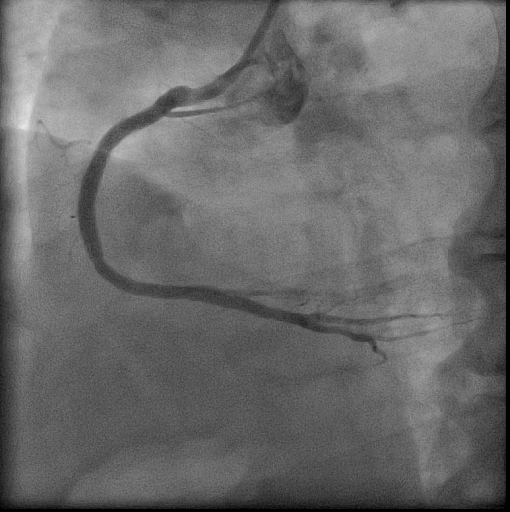
Images are shown before and after the percutaneous coronary intervention of RCA.
Complications
Following are the complications associated with the percutaneous coronary intervention.
- Coronary artery dissection
- Coronary artery perforation
- Distal embolization of clot
- Side branch occlusion
- Stent thrombosis
- Access site bleeding
- Access site hematoma
- Acute kidney injury
- Stroke
- Allergic reaction to contrast
Following are the complications associated with fluoroscopic radiation exposure to patients or staff.[8]
Tissue Reaction
- Skin Injury: It is the most common tissue reaction at the beam entry site following fluoroscopic guided percutaneous coronary intervention and varies according to time of exposure:
- Few hours to days of post-exposure: Mild skin erythema
- A week to several weeks of post-exposure: Significant erythema
- After 4 to 8 weeks of post-exposure: Severe skin injury including ulceration in rare cases
- Bone Injury: In rare cases, radiation can cause necrosis of superficial bones such as ribs.
- Eye Injury: The single-dose threshold of radiation that can cause a cataract to believe to be 500 mGy with a minimum latency period of one year.
Stochastic Effects: Radiation-Induced Cancer
It is the most important and catastrophic result of radiation exposure. It is vital to provide knowledge of the scholastic risk of radiation exposure to both patients and healthcare workers. These steps are necessary to reduce the risk, which includes the use of radiation protection instruments.
Clinical Significance
Fluoroscopic percutaneous coronary intervention is a widely performed procedure for the last several years. In comparison to thrombolysis, percutaneous coronary intervention reduces morbidity and mortality significantly in patients with myocardial infarction. In chronic coronary syndrome patients, it has proven to improve the quality of life. Compared to CABG, it is associated with a shorter hospital stay, no scar on the chest, and early mobilization after the procedure. Because of advancement in percutaneous coronary intervention over time, survival improvement in patients with coronary artery disease was noted.
Enhancing Healthcare Team Outcomes
Fluoroscopic percutaneous coronary intervention requires an interprofessional team including an intervention cardiologist, cath lab technician, radiation technician, and staff nurse. To improve outcomes, good collaboration among team members is essential. It is vital that every team member should be aware of their roles to avoid complications.
Nursing, Allied Health, and Interprofessional Team Interventions
The nursing staff gives medications and monitors vitals during the procedure. The radiographic technician set views on the fluoroscopy machine for the procedure and supports performing procedures such as intravascular imaging and invasive physiological assessment. The cath lab technician prepares equipment such as a coronary balloon, coronary stent and guides catheters for the procedure.
Media
(Click Image to Enlarge)
References
. Invasive compared with non-invasive treatment in unstable coronary-artery disease: FRISC II prospective randomised multicentre study. FRagmin and Fast Revascularisation during InStability in Coronary artery disease Investigators. Lancet (London, England). 1999 Aug 28:354(9180):708-15 [PubMed PMID: 10475181]
Level 1 (high-level) evidenceLespérance J, Saltiel J, Petitclerc R, Bourassa MG. Angulated views in the sagittal plane for improved accuracy of cinecoronary angiography. The American journal of roentgenology, radium therapy, and nuclear medicine. 1974 Jul:121(3):565-74 [PubMed PMID: 4846573]
Sos TA, Lee JG, Levin DC, Baltaxe HA. New lordotic projection for improved visualization of the left coronary artery and its branches. The American journal of roentgenology, radium therapy, and nuclear medicine. 1974 Jul:121(3):575-82 [PubMed PMID: 4846574]
Aldridge HE, McLoughlin MJ, Taylor KW. Improved diagnosis in coronary cinearteriography with routine use of 110 degrees oblique views and cranial and caudal angulations. Comparison with standard transverse oblique views in 100 patients. The American journal of cardiology. 1975 Oct 6:36(4):468-73 [PubMed PMID: 1190051]
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011 Dec 6:124(23):e574-651. doi: 10.1161/CIR.0b013e31823ba622. Epub 2011 Nov 7 [PubMed PMID: 22064601]
Level 1 (high-level) evidenceElliott LP, Green CE, Rogers WJ, Mantle JA, Papapietro S, Hood WP Jr. The importance of angled right anterior oblique views in improving visualization of the coronary arteries. Part I: Caudocranial view. Radiology. 1982 Mar:142(3):631-6 [PubMed PMID: 7063677]
Green CE, Elliott LP, Rogers WJ, Mantle JA, Papapietro S, Hood WP Jr. The importance of angled right anterior oblique views in improving visualization of the coronary arteries. Part II: Craniocaudal view. Radiology. 1982 Mar:142(3):637-41 [PubMed PMID: 7063678]
Hirshfeld JW Jr, Ferrari VA, Bengel FM, Bergersen L, Chambers CE, Einstein AJ, Eisenberg MJ, Fogel MA, Gerber TC, Haines DE, Laskey WK, Limacher MC, Nichols KJ, Pryma DA, Raff GL, Rubin GD, Smith D, Stillman AE, Thomas SA, Tsai TT, Wagner LK, Wann LS. 2018 ACC/HRS/NASCI/SCAI/SCCT Expert Consensus Document on Optimal Use of Ionizing Radiation in Cardiovascular Imaging: Best Practices for Safety and Effectiveness: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. Journal of the American College of Cardiology. 2018 Jun 19:71(24):e283-e351. doi: 10.1016/j.jacc.2018.02.016. Epub 2018 May 2 [PubMed PMID: 29729877]
Level 3 (low-level) evidence