Introduction
Intense pulsed light (IPL) therapy was first developed in 1992 by Doctors Goldman, Fitzpatrick, and Eckhouse for the treatment of leg telangiectasias. Proof-of-concept studies were conducted on rabbit ear veins, demonstrating IPL's ability to thermocoagulate vessels while minimizing purpura and epidermal damage.[1] Since the first United States Food and Drug Administration (FDA)-approved IPL device was brought to the market in 1995, this technology has undergone significant innovation and improvement in its clinical applications and affordability.[2][3]
IPL devices are unique in that they employ flashlamps and bandpass filters to produce pulsed light of varying wavelengths, durations, and fluences. These characteristics provide IPL versatility in addressing numerous dermatological conditions.[4][5] IPL is safe and effective in treating benign pigmented and vascular disorders as well as performing hair removal and reducing signs of photoaging.[6] Currently, IPL is an invaluable tool in dermatology and is frequently used to address a broad range of functional and cosmetic concerns.[7]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
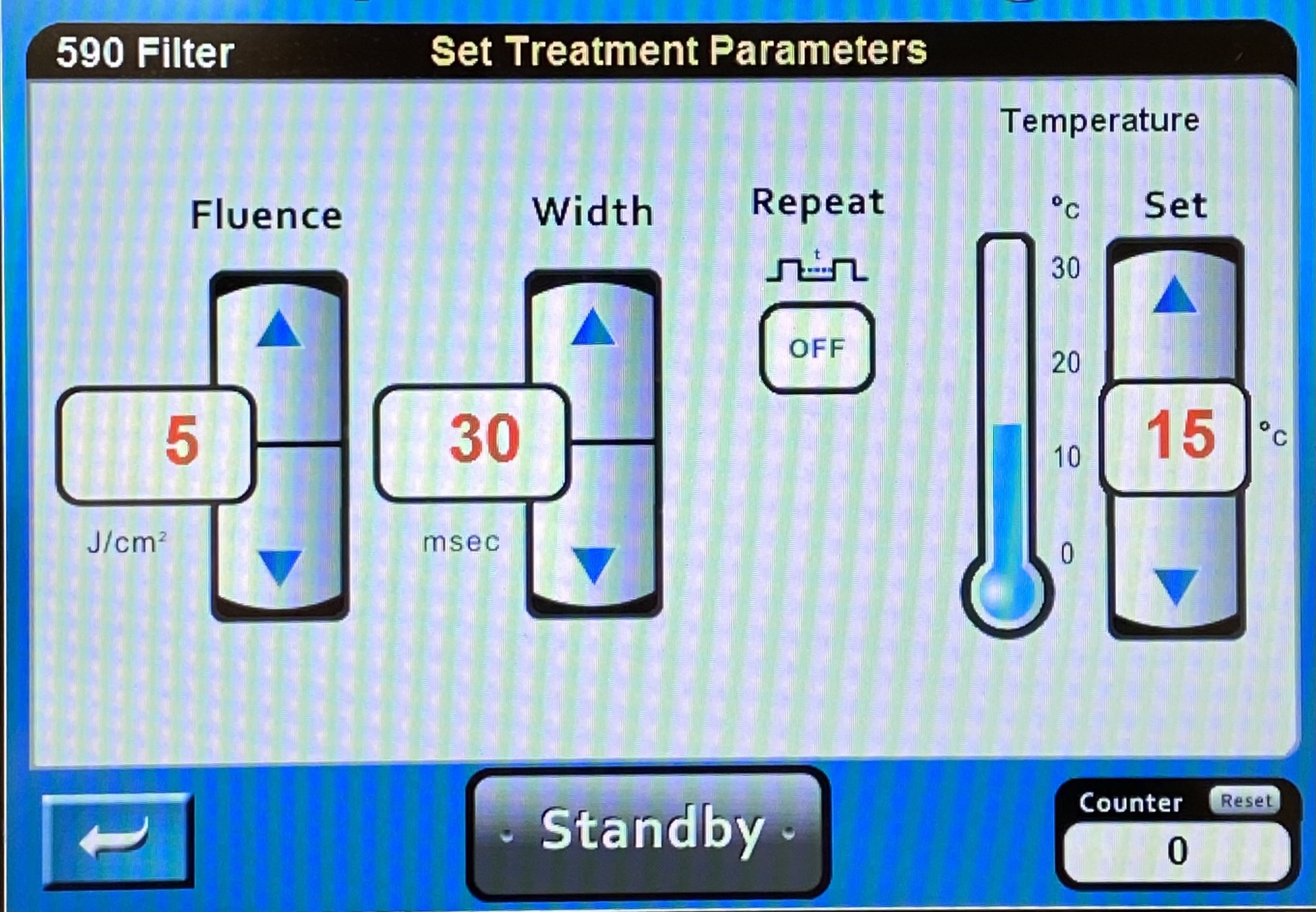
IPL uses a flashlamp to emit polychromatic light across a broad wavelength spectrum of approximately 400 to 1400 nm, which makes it fundamentally different from a laser (light amplification by stimulated emission of radiation), whose light is necessarily monochromatic (of a single wavelength), collimated (with waves running in parallel), and coherent (with waves in phase).[6] The advantage of broadband light is that it allows for greater versatility in treating a variety of skin types and conditions. Furthermore, the wavelength of light emitted from an IPL machine can be adjusted by applying filters that prevent the delivery of light with wavelengths shorter than the desired value (see Image. XXX). The result is that the desired wavelength is delivered along with longer wavelength light (such as infrared), but shorter wavelength light (such as ultraviolet) does not reach the patient.
Lasers and light energy delivery devices produce a clinical effect when their photons are absorbed by the skin, resulting in the deposition of thermal energy.[8] Chromophores (eg, hemoglobin, water, melanin) in the skin absorb the photons and are subsequently heated, causing their destruction through thermocoagulation. This phenomenon of selective photothermolysis is the underlying basis of IPL technology.[9]
Indications
The FDA has approved IPL therapy for:
- Telangiectasias
- Photorejuvenation
- Facial wrinkles
- Hyperpigmentation
- Lentigines
- Ephelides
- Melasma
- Rosacea
- Acne vulgaris
- Poikiloderma of Civatte
- Port-wine stains
- Hemangiomas
- Leg veins
- Venous malformations
- Removal of unwanted hair [10]
IPL was also recently introduced to ophthalmology to manage dry eye disease due to meibomian gland dysfunction.[11]
Contraindications
IPL treatment sessions are generally safe and tolerable. However, it may be beneficial to avoid IPL in certain individuals, such as those with a recent sunburn and in pregnant or breastfeeding women. IPL has also been found to induce herpes simplex virus (HSV) outbreaks, similar to laser treatments, via transient hyperthermia and reactivation of latent HSV in the trigeminal ganglion.[12] In patients with a previous history of HSV infection, starting prophylactic antiviral therapy (oral acyclovir, valacyclovir, or famciclovir) may be warranted a day before IPL treatment and continue for up to 2 weeks afterward.[13][14]
Equipment
The underlying mechanism of IPL therapy involves 4 crucial concepts: wavelength, pulse duration, fluence, and spot size.
Wavelength
Flashlamps emit polychromatic light within a wavelength spectrum of approximately 400 to 1400 nm.[15] The wavelength of light that reaches the patient can be adjusted using cut-off filters, which allow certain tissues to be targeted via selective photothermolysis. The skin contains different chromophores (molecules that absorb light of a specific wavelength), thereby converting it to thermal energy. When selecting a wavelength, the healthcare provider should be aware of competing chromophores within the treatment area. For example, melanin in the epidermis may shield the targeted chromophores located in a deeper layer of the skin.
This concept is particularly important when administering IPL in patients with darker skin types, as special attention must be given to treating them safely and preventing dyschromia. Since melanin tends to absorb light at shorter wavelengths, selecting longer wavelengths that penetrate deeper and spare the epidermis may benefit patients with darker skin. Given this same principle, shorter wavelengths effectively treat pigmented lesions in patients with lighter skin.[16]
Pulse Duration
Selection of the pulse duration is based on the thermal relaxation time (TRT) of the chromophore, or the time required for the temperature in the heated tissue to decrease to 37% of its peak.[17] To minimize thermal damage to the target tissue, the pulse duration (ie, the length of time the energy is being delivered) should be shorter than the target tissue's TRT. If the target is reheated before the TRT has elapsed after the last pulse of light is delivered, the surrounding tissue may suffer subsequent scarring or hypopigmentation.
Some IPL devices can only produce a single pulse, whereas others can produce multiple sequential pulses. Delay times between sequential pulses are routinely 10 to 12 ms to accommodate epidermal TRT, whereas a 20-to-40 ms TRT is advised for patients with darker skin types. Thermal relaxation time is also adjusted to account for chromophore and lesion size. Larger chromophores, such as hair follicles, require more time to cool down due to their longer TRT. Allowing appropriate TRT between pulses minimizes the risk of complications by preventing epidermal temperatures from rising above 70 ºC.
Fluence
Fluence, or energy density, describes the amount of energy delivered per unit area. IPL can deliver a fluence of up to 40 J/cm^2, whereas pigmented lesions are usually treated with a fluence of only 16 to 20 J/cm^2. A higher fluence may be used if a target is located deep within the skin or the chromophores are inefficient at absorbing light. Importantly, side effects tend to occur more frequently at higher fluences and in darker-skinned individuals.[18] Cooling devices assist with the delivery of higher fluences while protecting the epidermis from damage (epidermal bypass), as the thermal energy is delivered to deeper tissue.[19]
Cooling systems
Cooling systems provide epidermal protection and permit greater fluences to reach deeper targets. Cooling systems can be internal, such as integrated chilled tips, pulsed cryogen sprays, or cooled glass chambers. External cooling methods include ice packs, forced-air cooling, or cold ultrasound gel applied to the skin before a treatment session. The cold gel reduces the friction of the handpiece on the skin, diffuses the surface heat released from the handpiece, and decreases the refractive index between air and skin, allowing for better penetration and light absorption.
Spot Size
Spot size is the diameter of light that is emitted from the flashlamp. Increased spot size allows for light to penetrate deeper because scattering is minimized. Thus, a smaller spot size will require higher fluences to target deeper dermal targets effectively. Spot size is controlled using interchangeable aperture pieces (see Image. XXX).
Personnel
IPLght treatments, like many laser treatments, are typically provided in the outpatient clinic setting. A physician or surgeon may perform them, but it is frequently a midlevel healthcare provider, such as a physician assistant or a nurse practitioner, providing the treatments. In some regions, registered nurses are permitted to provide laser and IPL treatments as well. Regardless, having a physician, such as a plastic surgeon or dermatologist, involved in the care team ensures that an experienced clinician can manage complications promptly should they arise.
Preparation
Preparation for IPL treatment requires finding the patient a comfortable, private treatment room to expose whatever skin area is problematic without fear of embarrassment. The IPL machine requires a few square feet of floor space and frequently a 220-V outlet for power, which is not uniformly available in the United States. A cold gel is also helpful for improving patient comfort as well as energy transmission from the handpiece to the skin.
IPL can damage pigmented ocular tissues such as the retina; therefore, eye protection with the appropriate optical density is critical for the patient and the IPL treatment provider. Eye shields should not be repositioned midprocedure, as this may interfere with the treatment session and lead to inadvertent ocular damage.
Preprocedure informed consent is important for IPL treatments, as it is for any procedure, and the discussion should focus on the development of reasonable expectations, particularly with respect to final outcome, anticipated number of treatments required to achieve the desired result, postprocedure precautions, like avoiding sun exposure, and the potential for complications, such as temporary or permanent hyper or hypopigmentation, erythema, crusting, blistering, and scarring.[20][21]
Technique or Treatment
In contrast to lasers, IPL devices produce noncoherent, polychromatic light with a broad range of wavelengths. Their fluence, pulse duration, spot size, and filter wavelength can be adjusted in order to target specific chromophores. Thus, IPL devices can treat a wide variety of lesions and skin types. Lesion clearance often depends on the frequency of treatment sessions because the effect of pulsed light is cumulative, routinely requiring 3 to 6 treatments every 2 to 4 weeks for the full clinical effect to be achieved.[4]
Lesions that are more heavily pigmented may require a higher number of treatment sessions. Lesions deeper within the dermis may also require more treatments as they are more challenging to reach. Compared with laser devices, IPL is associated with a shorter recovery time and lower equipment costs. Disadvantages of IPL include incorporating the lamp and cooling device into the handpiece, which contributes to device heaviness (see Image. XXX). Cold gel applied to the skin also diminishes the visibility of immediate local skin reactions.[6]
Selection of the appropriate filter is critical to achieving the desired results, just as setting appropriate fluence and pulse duration is essential for avoiding complications. The default settings on most IPL devices are designed to provide safe treatments with minimal risk of complications, but using these cautious settings may prove less clinically effective than more aggressive energy delivery parameters (see Image. XXX). Starting a course of treatment with conservative settings, however, is advisable. Shorter wavelength filters permit less skin penetration than longer wavelength filters. Typical filter wavelengths and their indications are listed in the table below:
|
IPL Filter Settings |
|||||
|
Indication |
Acne |
Pigmented Lesions |
Vascular Lesions |
Rejuvenation |
Hair Removal |
|
Wavelength |
420-430 nm |
515-530 nm |
560-590 nm |
570-690 nm |
640-800 nm |
Complications
Although side effects of IPL are typically rare and minimal in severity, the most common adverse events include pain and erythema. Other reported side effects include edema, bullae, hematoma, crusting, hyper- or hypopigmentation, leukotrichia, scarring, keloid formation, and infection.[21] For untrained medical providers, the use of inappropriate device settings and administration of excess energy can lead to nonspecific thermal damage and complications. IPL is particularly challenging to use on dark-skinned individuals, and careful consideration must be given to these patients.
Shorter wavelengths are generally reserved for fair skin types, as these wavelengths are absorbed by melanin and lead to pigmentation changes in patients with darker skin. However, device-related cooling technology has helped minimize these side effects in patients with darker complexions. Skin reactions typically last for about 2 to 48 hours after treatment and often depend on the fluence, pulse duration, and specific treatment area. Higher fluences and pulse durations, thinner skin, and darker skin types may increase the likelihood of adverse events.
In patients undergoing hair removal, the adverse effect of paradoxical hypertrichosis may occur.[22] This is the phenomenon of the growth of fine, dark hair in areas close to the target tissue, especially in patients with darker skin types (Fitzpatrick III-VI). The underlying mechanism has not been fully elucidated. Still, potential causes include IPL stimulating hair follicular stem cells to promote hair growth and inducing the release of cytokines and growth factors with the conversion of vellus hairs to terminal hairs.[23][24] Treatment options include increasing the energy, decreasing the interval between treatments, using more cooling, changing the wavelengths (eg, from IPL to 1,064-nm Nd:YAG laser), and using topical eflornithine to slow down hair regrowth after treatments.
Clinical Significance
IPL utilizes high-intensity light sources to treat a wide range of dermatological conditions. IPL technology has evolved tremendously since the 1990s with the addition of higher-intensity flashlamps, cut-off filters, and cooling systems. These features have enabled IPL to be an ideal tool for treating a variety of pigmented lesions, including solar lentigines and ephelides, vascular lesions such as telangiectasias, port-wine stains, hemangiomas, and leg veins, as well as unwanted hair and photoaging.[25][26] Newer IPL devices also allow for more specific targeting with increased accuracy and less light scattering.
Enhancing Healthcare Team Outcomes
Achieving the best outcomes with intense pulsed light therapy involves an interprofessional team of healthcare providers, including a skilled dermatologist or plastic surgeon and often a physician assistant or nurse practitioner, aesthetician, medical assistant, and office staff. The patient should be educated on what to expect during and after the procedure as well as potential side effects. For example, the patient should be counseled on cold gel application before IPL delivery and using protective eyewear during sessions as well as the importance of sun protection after treatment. It is also important to gauge the patient's expectations and assess clinical improvement accordingly. Patients should be informed that the best results are achieved after a series of at least 2 or more IPL treatments.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Goldman MP, Martin DE, Fitzpatrick RE, Ruiz-Esparza J. Pulsed dye laser treatment of telangiectases with and without subtherapeutic sclerotherapy. Clinical and histologic examination in the rabbit ear vein model. Journal of the American Academy of Dermatology. 1990 Jul:23(1):23-30 [PubMed PMID: 2365873]
Level 3 (low-level) evidenceRaulin C, Greve B, Grema H. IPL technology: a review. Lasers in surgery and medicine. 2003:32(2):78-87 [PubMed PMID: 12561039]
Raulin C, Weiss RA, Schönermark MP. Treatment of essential telangiectasias with an intense pulsed light source (PhotoDerm VL). Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 1997 Oct:23(10):941-5; discussion 945-6 [PubMed PMID: 9357506]
Husain Z, Alster TS. The role of lasers and intense pulsed light technology in dermatology. Clinical, cosmetic and investigational dermatology. 2016:9():29-40. doi: 10.2147/CCID.S69106. Epub 2016 Feb 4 [PubMed PMID: 26893574]
Li D, Lin SB, Cheng B. Intense Pulsed Light: From the Past to the Future. Photomedicine and laser surgery. 2016 Oct:34(10):435-447 [PubMed PMID: 27697004]
Babilas P, Schreml S, Szeimies RM, Landthaler M. Intense pulsed light (IPL): a review. Lasers in surgery and medicine. 2010 Feb:42(2):93-104. doi: 10.1002/lsm.20877. Epub [PubMed PMID: 20166155]
Wat H, Wu DC, Rao J, Goldman MP. Application of intense pulsed light in the treatment of dermatologic disease: a systematic review. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2014 Apr:40(4):359-77. doi: 10.1111/dsu.12424. Epub 2014 Feb 4 [PubMed PMID: 24495252]
Level 1 (high-level) evidencePatil UA, Dhami LD. Overview of lasers. Indian journal of plastic surgery : official publication of the Association of Plastic Surgeons of India. 2008 Oct:41(Suppl):S101-13 [PubMed PMID: 20174534]
Level 3 (low-level) evidenceAnderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science (New York, N.Y.). 1983 Apr 29:220(4596):524-7 [PubMed PMID: 6836297]
Level 3 (low-level) evidenceGoldberg DJ. Current trends in intense pulsed light. The Journal of clinical and aesthetic dermatology. 2012 Jun:5(6):45-53 [PubMed PMID: 22768357]
Giannaccare G, Taroni L, Senni C, Scorcia V. Intense Pulsed Light Therapy In The Treatment Of Meibomian Gland Dysfunction: Current Perspectives. Clinical optometry. 2019:11():113-126. doi: 10.2147/OPTO.S217639. Epub 2019 Oct 17 [PubMed PMID: 31802961]
Level 3 (low-level) evidenceAdamic M, Troilius A, Adatto M, Drosner M, Dahmane R. Vascular lasers and IPLS: guidelines for care from the European Society for Laser Dermatology (ESLD). Journal of cosmetic and laser therapy : official publication of the European Society for Laser Dermatology. 2007 Jun:9(2):113-24 [PubMed PMID: 17558762]
Qiao C, Li L, Wang H, Zhao C, Ke L, Sen D, Qi M, Li S, Wang M, Zeng Q. Adverse Events of Intense Pulsed Light Combined With Meibomian Gland Expression Versus Meibomian Gland Expression in the Treatment of Meibomian Gland Dysfunction. Lasers in surgery and medicine. 2021 Jul:53(5):664-670. doi: 10.1002/lsm.23339. Epub 2020 Nov 8 [PubMed PMID: 33161597]
Level 2 (mid-level) evidenceRemington BK, Remington TK. Treatment of facial lentigines in Peutz-Jeghers syndrome with an intense pulsed light source. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2002 Nov:28(11):1079-81 [PubMed PMID: 12460308]
Level 3 (low-level) evidenceAsh C, Dubec M, Donne K, Bashford T. Effect of wavelength and beam width on penetration in light-tissue interaction using computational methods. Lasers in medical science. 2017 Nov:32(8):1909-1918. doi: 10.1007/s10103-017-2317-4. Epub 2017 Sep 12 [PubMed PMID: 28900751]
Tanzi EL, Lupton JR, Alster TS. Lasers in dermatology: four decades of progress. Journal of the American Academy of Dermatology. 2003 Jul:49(1):1-31; quiz 31-4 [PubMed PMID: 12833005]
Yadav RK. Definitions in laser technology. Journal of cutaneous and aesthetic surgery. 2009 Jan:2(1):45-6. doi: 10.4103/0974-2077.53103. Epub [PubMed PMID: 20300375]
Halachmi S, Lapidoth M. Low-fluence vs. standard fluence hair removal: a contralateral control non-inferiority study. Journal of cosmetic and laser therapy : official publication of the European Society for Laser Dermatology. 2012 Feb:14(1):2-6. doi: 10.3109/14764172.2011.634421. Epub [PubMed PMID: 22129205]
Level 3 (low-level) evidenceWall TL. Current concepts: laser treatment of adult vascular lesions. Seminars in plastic surgery. 2007 Aug:21(3):147-58. doi: 10.1055/s-2007-991183. Epub [PubMed PMID: 20567666]
Riml S, Larcher L, Grohmann M, Kompatscher P. Second-degree burn within a tattoo after intense-pulsed-light epilation. Photodermatology, photoimmunology & photomedicine. 2013 Aug:29(4):218-20. doi: 10.1111/phpp.12039. Epub [PubMed PMID: 23815356]
Level 3 (low-level) evidenceRadmanesh M, Azar-Beig M, Abtahian A, Naderi AH. Burning, paradoxical hypertrichosis, leukotrichia and folliculitis are four major complications of intense pulsed light hair removal therapy. The Journal of dermatological treatment. 2008:19(6):360-3. doi: 10.1080/09546630802132627. Epub [PubMed PMID: 18654911]
Level 2 (mid-level) evidenceDesai S, Mahmoud BH, Bhatia AC, Hamzavi IH. Paradoxical hypertrichosis after laser therapy: a review. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2010 Mar:36(3):291-8. doi: 10.1111/j.1524-4725.2009.01433.x. Epub 2010 Jan 19 [PubMed PMID: 20100274]
Lolis MS, Marmur ES. Paradoxical effects of hair removal systems: a review. Journal of cosmetic dermatology. 2006 Dec:5(4):274-6 [PubMed PMID: 17716243]
Town G, Bjerring P. Is paradoxical hair growth caused by low-level radiant exposure by home-use laser and intense pulsed light devices? Journal of cosmetic and laser therapy : official publication of the European Society for Laser Dermatology. 2016 Oct:18(6):355-62. doi: 10.3109/14764172.2016.1157373. Epub 2016 May 9 [PubMed PMID: 26983796]
Taub AF. Treatment of rosacea with intense pulsed light. Journal of drugs in dermatology : JDD. 2003 Jun:2(3):254-9 [PubMed PMID: 12848109]
Kontoes PP, Vlachos SP, Marayiannis KV. Intense pulsed light for the treatment of lentigines in LEOPARD syndrome. British journal of plastic surgery. 2003 Sep:56(6):607-10 [PubMed PMID: 12946381]
Level 3 (low-level) evidence