Continuing Education Activity
Superficial cervical plexus block is an easy block that can be performed either using a landmark-based technique or using the ultrasound-based technique. This activity outlines the practical use of superficial cervical plexus block as performed by the bedside clinician in improving the care for patients presenting to the operating room or to the emergency department who require regional anesthesia. This activity review the clinical significance, technique, and potential complications of the procedure to enhance the delivery of this procedure and to improve outcomes.
Objectives:
- Summarize the typical surgeries, injuries, and conditions that would require a superficial cervical plexus block.
- Describe the equipment and medications (including the local anesthetic options) required to perform a successful superficial cervical plexus block.
- Outline the technique required to perform a successful superficial cervical plexus block.
- Explain the importance of improving care coordination amongst the interprofessional team to enhance the delivery of care for patients receiving a superficial cervical plexus block.
Introduction
Regional anesthesia can be part of a multi-model treatment plan to mitigate pain for clinical scenarios frequently seen in an emergency department and in the perioperative setting. Preoperatively, these blocks can be employed for a variety of surgical procedures. In the emergency department, it can be utilized for insertion of internal jugular central venous catheters, treatment of clavicular fractures and repairing lacerations, and draining abscesses that involve the earlobe and submandibular areas. The superficial cervical plexus block provides ipsilateral anesthesia to the "cape" region roughly bordered by the posterior tip of the earlobe, the lateral end of the clavicle, the medial aspect of the mandible and the inferior surface of the clavicle.[1] Cervical plexus blocks are easy to perform and provide anesthesia for the surgical procedure in the distribution of C2 to C4, including carotid endarterectomies, lymph node dissection, and plastic surgery.[2][3] The superficial cervical plexus block can also be used in combination with the deep cervical plexus block for regional anesthesia in oral and maxillofacial surgery.[4]
Anatomy and Physiology
The superficial cervical plexus has its origins from the ventral rami of the nerve roots C2 to C4. These nerve roots provide sensation to the skin and superficial structures of the ear auricle, acromioclavicular joint, clavicle, and anterolateral neck.[1] These branches exit at a midpoint along the posterior border of the sternocleidomastoid muscle (SCM) at the same level as the thyroid cartilage notch. These roots combine to form the four terminal branches, namely the lesser occipital, greater auricular, transverse cervical, and supraclavicular nerves. They emerge from behind the posterior border of the SCM. The plexus can be visualized as a small collection of hypoechoic oval structure, deep or lateral to the posterior border of the SCM, but this is not always apparent. The goal of this block is to deposit local anesthetic near the sensory branches of nerve roots C2, C3, and C4. SCM forms a “roof” over the nerve roots of the superficial cervical plexus (C2–4). The advantages of ultrasound guidance include visualization of the spread of local anesthetic and continuous monitoring of needle tip depth. While this paper provides sufficient anatomical information to perform a superficial cervical plexus block, there are other resources available for those interested in pursuing a more detailed review of the sonoanatomy of the cervical region.[5]
Indications
A superficial cervical plexus block is indicated when there is a need for dense anesthesia and/or analgesia to the skin and underlying anatomy of the anterolateral neck. In addition to the anterolateral neck, anesthesia is achieved in the superficial structures of the ear, clavicle and the acromioclavicular joint.[6] Common indications for superficial cervical plexus block include carotid endarterectomies, lymph node dissections, and superficial neck surgeries. In the emergency department, it can be utilized for insertion of internal jugular central venous catheters, treatment of clavicular fractures and repairing lacerations, and draining abscesses that involve the earlobe and submandibular areas. While there are no other published studies available, a single case series showed this block to be successfully used in pediatric patients requiring internal jugular venous placement for emergent dialysis.[7]
Contraindications
Contraindications for superficial cervical plexus block include patient refusal, active infection overlying the injection site, contralateral phrenic nerve paralysis, previous neck surgery, neck radiation, and allergy to both amide and ester local anesthetic agents.[6] Caution must be exercised in patients who suffer from severe chronic obstructive pulmonary disease or an untreated contralateral pneumothorax as this block has the potential for inadvertent phrenic nerve dysfunction. This potential complication, however, has been recently challenged by a recent prospective randomized study.[8]
Equipment
- Sterile towels
- Sterile 4 × 4 inches gauze pads
- High frequency (6 Hz to 13 Hz) linear ultrasound probe, ultrasound gel and sterile probe cover (or other sterile barriers) if using ultrasound guidance
- Skin preparation using chlorhexidine or iodine-based solution
- Local anesthetic with the appropriate duration of action, e.g., shorter-acting agents like lidocaine for laceration repairs and longer-acting agents like ropivacaine for clavicular fractures
- 25 - 27 gauge 1 and 1/2 inch needle
- 10 mL to 20 mL syringe
Personnel
In general, only one operator is required. If a second operator is available, they may assist with patient positioning, equipment, machine location, screen optimization, and image recording.
Preparation
This is carried out by using many of the same standard precautions undertaken for nerve blocks. The procedure should be explained to the patient, and, depending on institutional policy, verbal/written consent should be obtained. The clinician, primary nurse, and pharmacist should all be familiar with the recognition and treatment of local anesthetic systemic toxicity.[9] Ensure the injection site does not have signs of infection and prepare it with an antiseptic solution. Don sterile gloves, cover the probe surface with a sterile cover and place sterile ultrasound gel over the probe contact site.
Technique or Treatment
Patient Positioning
Supine, semi-sitting (with head turned to the contralateral side), or lateral decubitus. Lateral decubitus position allows the ultrasound to be placed across from the patient for optimal ergonomics and viewing of the display screen. The patient's comfort and limitations must be taken into consideration during positioning. In obese patients, the posterior border of the SCM can be difficult to identify. Ask the patient to lift his/her head off the bed to facilitate palpation of the posterior border of the SCM.
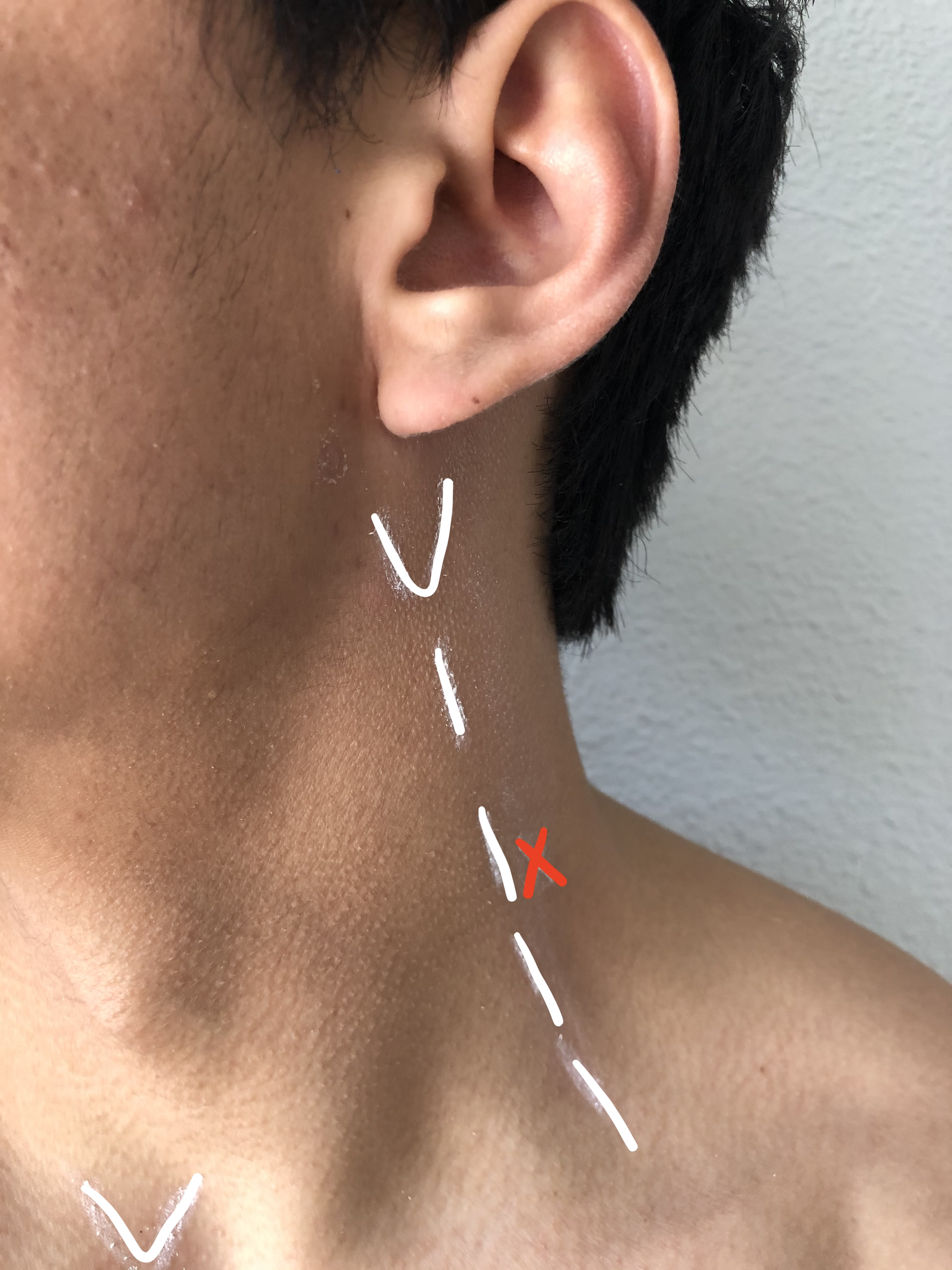
Landmark-based Technique
A line extending from C6 to the mastoid process is drawn (along the posterior border of the SCM). The needle insertion is at the midpoint of this line. The branches of the superficial cervical plexus emerge behind the posterior border of the sternocleidomastoid muscle at this point. Skin is prepped and draped in the usual fashion. Using a "needle fanning" technique with repeated needle redirections, the local anesthetic is injected alongside the posterior border of the sternocleidomastoid muscle 2 cm to 3 cm below and above the needle insertion site. Avoid deep needle insertion (greater than 1 cm to 2 cm).
Ultrasound-based Technique
Place the high-frequency linear probe in a transverse orientation for an in-plane approach (parallel to the probe axis). This should be done at a location over the midpoint of the posterior border of the sternocleidomastoid muscle. This also approximates the level of C4 and the notch of the thyroid process. The probe marker should be pointed medially towards the thyroid cartilage. Skin is prepped and draped in the usual fashion. Insert the needle in lateral to medial direction 1 cm to 2 cm directly under the posterior border of the sternocleidomastoid muscle. The needle should enter at the level of the thyroid cartilage (located halfway between the clavicle and mastoid bone). Place the needle tip in a position to inject the local anesthetic just deep to the posterolateral tapering sternocleidomastoid muscle and superior to the levator scapula as this thick fascial layer is the location of the cervical plexus. The needle tip should not be further than 2 cm deep to prevent inadvertent injection into underlying structures. While directly visualizing the needle tip to prevent inadvertent intravascular injection, inject approximately 5 mL to 10 mL of local anesthetic.[1][6]
Of note, experienced operators have been found to have a similar success rate when using the landmark-based technique only vs. an ultrasound-guided technique.[10]
Complications
Local anesthetic systemic toxicity from the inadvertent intravascular injection is possible. Familiarity with treating local anesthetic systemic toxicity is required before performing the superficial cervical plexus block.[9] Inadvertent deep injection or excessive local anesthetic volume can cause dysfunction/blockade of the recurrent laryngeal nerve, deep cervical plexus, and brachial plexus.[1] It is also thought to cause dysfunction of the phrenic nerve, though a recent prospective randomized study found this to not be the case.[8] Accidentally blocking the accessory nerve can cause sternocleidomastoid and trapezius muscle weakness. Puncture of the internal jugular vein and carotid artery is also possible.[6] This can be minimized with the use of ultrasound.
Clinical Significance
Superficial cervical plexus block provides dense anesthesia for procedures like carotid endarterectomies, lymph node dissection, plastic surgery, laceration repairs, and incision and drainage of abscesses. It avoids the potential for under- or overdosing when using oral or parenteral analgesics. It can be done expeditiously, using minimal resources, and is safe. It can be done prior to placing an internal jugular central venous catheter to allow for pain-free line placement. An ultrasound-guided superficial cervical plexus block using a longer-acting local anesthetic like ropivacaine can provide sufficient analgesia for a clavicle fracture to the point where over the counter medications can manage the residual pain.
Enhancing Healthcare Team Outcomes
Patients frequently present to the emergency department with a pain associated symptom. It is clinicians' responsibility to possess the skills that allow them to optimally manage their patients' pain. This includes a sound knowledge of ultrasound and its utility in safely allowing the performance of nerve blocks, including the superficial cervical plexus block.
Good interprofessional communication between physicians, nurses, and pharmacists will ensure the right patient is appropriately prepared and given the correct dose of the appropriate medicine for the procedure. All local anesthetic agents have the potential for adverse effects progressing to local anesthetic systemic toxicity, so shared communication among the health care team is vital. Outcomes are improved, and patient safety is enhanced when medication doses are cross-checked by the patient's primary nurse and pharmacy prior to administration. [Level 5]