Continuing Education Activity
Central retinal artery occlusion (CRAO) is a relatively rare but potentially devastating ocular emergency. Patients present with sudden, painless monocular vision loss. The prognosis for visual recovery is poor, and up until fairly recently, there was no treatment that could restore any degree of functional vision to the affected eye. Central retinal artery occlusion leads to hypoxia, and the retinal tissue is especially intolerant of hypoxia. In 2006, hyperbaric oxygen therapy was approved for the treatment of central retinal artery occlusion, though it remains a vastly underutilized modality, partially due to lack of availability and lack of awareness in the ophthalmology community. This activity describes the pathophysiology, evaluation, and management of central retinal artery occlusion and highlights the role of the interprofessional team in caring for affected patients.
Objectives:
- Identify the etiology of central retinal artery occlusion.
- Desrcibe the presentation of a patient with central retinal artery occlusion.
- Review the treatment and management options available central retinal artery occlusion.
- Summarize a well-coordinated interprofessional team approach to provide effective care to patients affected by central retinal artery occlusion.
Introduction
Central retinal artery occlusion (CRAO) is a relatively rare emergency and potentially devastating condition of the eye. Patients present with sudden, painless monocular vision loss. The prognosis for visual recovery is poor, and up until recently, no treatment could be offered to restore at least some functional vision to the affected eye. The retina has the highest oxygen consumption rate of any organ in the body at 13 mL/100 gm per min. Retinal tissue is not tolerant of hypoxia. Until 2006 when hyperbaric oxygen therapy was approved for treatment of central retinal artery occlusion, ophthalmologists had no treatment options for these patients. It is still a vastly underutilized modality, partially due to lack of availability and lack of knowledge in the ophthalmology community.[1][2][3][4]
Etiology
Patients at increased risk for developing central retinal artery occlusion are those with:
- Giant cell arteritis
- Atherosclerosis
- Thromboembolic disease
Arterial supply to the eye is via the ophthalmic artery which is a branch of the cavernous portion of the internal carotid artery. The central retinal artery enters the globe along with the optic nerve and serves the inner layers of the retina through its many branches. Fifteen percent to 30% of the population have a cilioretinal artery which is part of the choroidal arterial supply. This supplies the area of the retina around the macula which is the central vision area. Patients who have a cilioretinal artery may still have preserved central vision because this portion of the retina is still being perfused.
In central retinal artery occlusion, the inner retinal layers which are normally served by the retinal circulation will die. This is what causes the vision loss. However, these layers may receive enough oxygen via diffusion from the choroidal circulation to maintain viability if the patient is exposed to increased FiO2. Normally the choroidal circulation supplies most of the oxygen to the retina.[5][6][7]
Epidemiology
Central retinal artery occlusion is a rare, emergent eye condition that should be suspected in any patient who presents with unilateral sudden painless vision loss. These patients usually present with vision loss in the range of finger counting to light perception. Patients who present with no light perception in the affected eye may have occluded the ophthalmic artery close to where it enters the eye which causes permanent and debilitating vision loss.
Pathophysiology
If the level of occlusion is at the ophthalmic artery, there may be no treatment options available to the patient. This is because posterior ciliary circulation is blocked, and there is no collateral circulation to the inner layers of the retina.[8][9][10]
Therapy must be started before the tissue is irreparably damaged.
The degree and location of occlusion will affect the response to treatment.
The adequate partial pressure of oxygen must be maintained long enough for the retinal vessels to recanalize. This usually occurs within 72 hours.
The largest published case series (Hayreh) showed the natural progression of disease without treatment with hyperbaric oxygen.
- Some patients had transient symptoms for minutes to hours that resolved without treatment, and they were left with minimal visual impairment.
- ABout 80% of patients without cilioretinal arteries had the final visual outcome of finger counting or less, and only 1.5% had a final vision of 20/40 or better in the affected eye.
- Patients with cilioretinal arteries had much better outcomes the those who did not.
History and Physical
The classic presentation is a sudden, painless loss of vision in the range of light perception to finger counting. Visual acuity may be in the range of 20/200 but is often worse.
If a patient has no light perception, this may indicate an ophthalmic artery occlusion, and therefore, no blood is flowing to choroidal vessels.
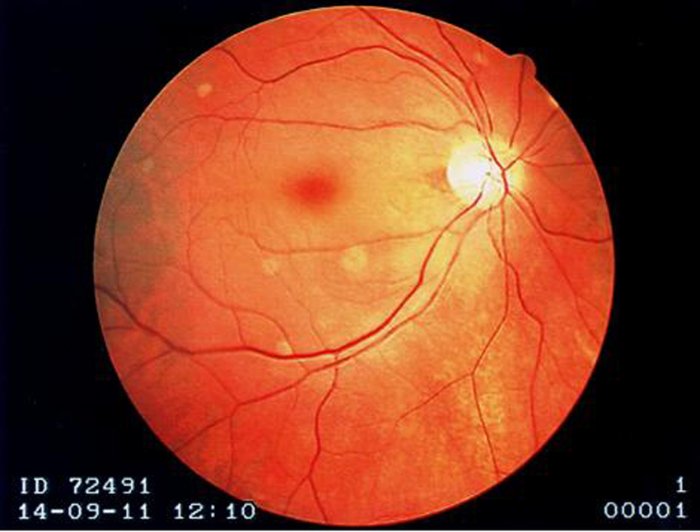
If central visual acuity is spared and fundoscopy is consistent with central retinal artery occlusion, then the patient probably has a cilioretinal artery blood supply. The fundoscopy may show a pale yellow ischemic retina. A cherry-red spot may be present where the macula is, but this is not a consistent or reliable finding. The presence of a cherry red spot is an indicator of poor prognosis.
Evaluation
Triage this condition as emergent. This is a "stroke of the eye" and should be treated with the same urgency as an evolving stroke or myocardial infarction. Fundoscopy should be performed and documented immediately. An ophthalmologist should be consulted, preferably a vitreoretinal specialist. The presence of pain, a history of trauma, findings of flashers or floaters, and age younger than 40 years are more common with ocular trauma, retinal detachment, or vitreal hemorrhage and make central retinal artery occlusion less likely.
Treatment / Management
General Treatment
- Provide immediate supplemental oxygen at highest normobaric FiO2 available.
- Consult ophthalmology but do not delay treatment if readily available.
- Baseline complete blood count (CBC), ESR, C-reactive protein (CRP), prothrombin time (PT), partial thromboplastin time (PTT), INR if on coumadin
- ECG
- Carotid ultrasound, MRI, and echocardiogram can be done later. These are not urgent studies for these patients but are part of the complete assessment for risk factor modification, just as in stroke.
- If the onset of symptoms is within 24 hours of presentation, and the patient has no response to normobaric hyperoxia after 15 minutes, refer for emergency hyperbaric medicine consultation.
Hyperbaric Oxygen Treatment Protocol
Indicated for central retinal artery occlusion (UHMS Hyperbaric Oxygen Indications, 13th Ed., Weaver)
Initial treatment:
- Compress to 2 atmosphere absolute (ATA).
- If vision improves significantly at 2 ATA, then remain at this depth for 90 minutes.
- If vision fails to improve after 30 minutes at 2 ATA, then compress to 2.4 ATA, and if vision improves at this depth, treat at this depth for 90 minutes. If there is no improvement at 2.4 ATA, compress to 2.8 ATA and perform the US Navy Treatment Table No. 6.
If no improvement after initial US Navy Table No. 6, options are:
- Discontinue treatment
- Continue with normobaric oxygen therapy
- Give 2 additional treatments at 2.8 ATA for 90 minutes with 5-minute air breaks every 30 minutes 2 times per day and reassess after 4 to 6 days. Most patients will reach a plateau after which they will not experience any further improvement in visual acuity and treatment can then be discontinued. Some patients require 8 treatments before having an improvement in visual acuity, but few if any patients will respond beyond this point.
Differential Diagnosis
The differential for acute painless vision loss includes central retinal vein occlusion, vitreous hemorrhage, retinal detachment, posterior circulation stroke, ischemic optic neuropathy, and amaurosis fugax.
Prognosis
Patients treated with hyperbaric oxygen within 8 hours of symptom onset have an 83% chance of an improvement in visual acuity of 3 lines or better on the Snellen chart.
Pearls and Other Issues
Recovery or improvement of visual acuity during the initial treatment of central retinal artery occlusion with Hyperbaric Oxygen (HBO2) indicates retinal viability and the potential for return of vision despite the ischemic period suffered before treatment.
The retina may not survive after ischemia lasting longer than 90 minutes.
Animal models of retinal injury have shown a reduction in apoptosis from 58% cell loss to 30% in animals treated with HBO2 after experimental central retinal artery occlusion.
Acute obstruction of the central retinal artery even when treated promptly, typically results in severe, permanent vision loss.
Recent studies are looking at using thrombolytics and surgical removal of clots, and while this is promising, outcomes have been disappointing.
Supplemental O2 is a mainstay in the treatment of central retinal artery occlusion. Retinal blood flow may be reestablished in 72 hours via recanalization. However, if ischemia and hypoxia have resulted in cell death and necrosis of the inner retinal layers usually supplied by the retinal artery, vision may not return with recanalization. Tissue that is ischemic but capable of recovery within a certain timeframe is the ischemic penumbra.
Central retinal artery occlusion should be treated as a stroke of the eye and admitted to the hospital for close monitoring, testing, and risk factor modification.
Hyperbaric oxygen for central retinal artery occlusion is an American Heart Association level IIB recommendation. It is one of the only treatments we can offer to patients who suffer this debilitating condition.
Enhancing Healthcare Team Outcomes
CRAO is best managed by an interprofessional team that includes ER triage nurses. Clinicians need to know that CRAO is a medical emergency. In the past, there were no treatments for this condition but now numerous series indicate that HBO therapy may help. Thus, triage and rapid transfer of these patients to an HBO chamber is paramount, if vision is to be saved. Fundoscopy should be performed and documented immediately. An ophthalmologist should be consulted, preferably a vitreoretinal specialist.
Patients with CRAO with symptom duration of less than 6 to 8 hours have the best outcomes after HBO therapy.[4]