Continuing Education Activity
Hand and wrist injuries are prevalent across diverse age groups and activity levels and require prompt and effective intervention. Wrist splinting is a valuable technique for all healthcare providers, providing a versatile alternative to rigid casting. Thumb spica splints have several benefits, as they provide structural support without enclosing the limb fully. Thumb spica splints allow adequate accommodation of swelling in the initial phases of injury. Splint flexibility addresses the challenges posed by the need for multiple examinations and imaging in the acute phase, stabilizing the injured area while allowing access during repeated clinical assessments.
This activity focuses on applying thumb spica splints as an immobilization measure in managing acute hand and wrist injuries. Attendees gain insights into the anatomy, indications, and contraindications of thumb spica splints. A deeper understanding of hands-on techniques for proper thumb spica placement enhances proficiency. The session emphasizes the pivotal role healthcare professionals play in the early immobilization of injuries to the radiocarpal joint, carpal bones, tendons, and ligaments of the lateral hand.
Objectives:
Identify patients with indications for thumb spica splinting.
Implement the proper technique for placing a thumb spica splint.
Identify the thumb spica splint properties that may give rise to postapplication complications.
Implement interprofessional care coordination strategies to improve outcomes for patients with hand injuries managed by thumb spica splinting.
Introduction
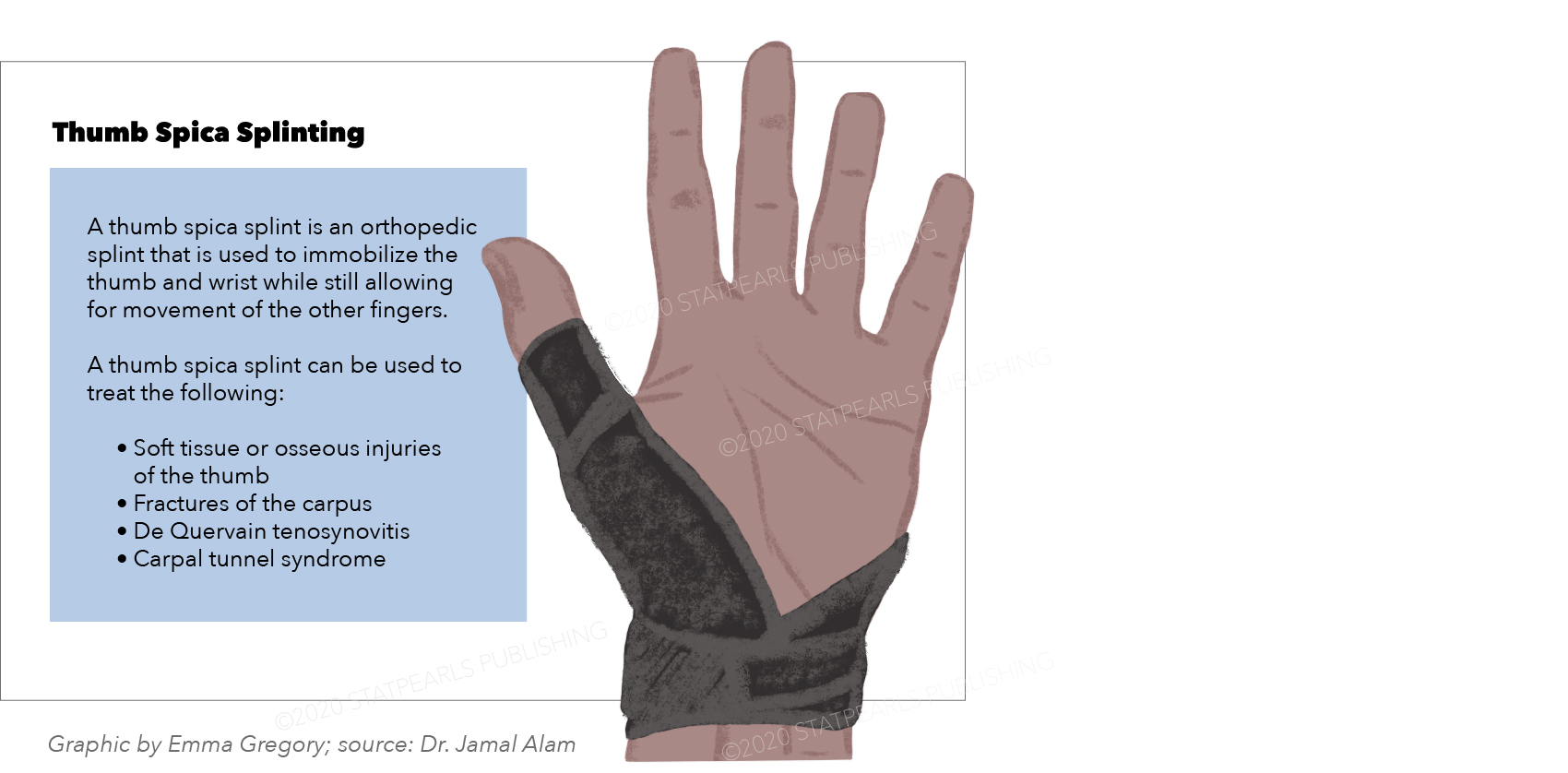
Acute hand and wrist injuries impact patients of all ages and activity levels. These injuries may arise from low-energy trauma during normal daily activities, eg, ground-level falls in older individuals, and recreational and elite-level sporting events. Wrist splinting is an essential component in the treatment arsenal of all healthcare providers (see Image. Thumb Spica Splint). The procedure creates periarticular joint and wrist stability and may be used as a definitive intervention for mild hand and wrist injuries. Additionally, splinting can serve as a temporary presurgical immobilization measure. This technique provides structural support, accommodates swelling, and protects from further soft tissue injuries before a hand or wrist surgery. Splints can be removed for clinical reevaluation or repeat imaging, making them a valuable alternative to rigid fiberglass or plaster casting.[1]
Anatomy and Physiology
Radiocarpal Joint
The radiocarpal (wrist) joint is a condyloid synovial joint of the distal upper limb connecting the forearm and hand. The wrist is a modified ball-and-socket joint formed through articulations between the distal radius' concave surface, the articular disc, and the convex scaphoid, lunate, and triquetrum bones. This joint allows flexion, extension, abduction, and adduction movements.[2] Laterally to medially, the distal row of carpal bones are the trapezium, trapezoid, capitate, and hamate.
The ulna is not part of the wrist joint. However, this forearm bone articulates distally with the radius via the distal radioulnar joint.[3]
The radiocarpal ligament is large. This ligament is present on the dorsal and palmar wrist surfaces and connects the radius to the distal carpal bones.[4] Dense fibrous connective tissue filled with synovial fluid wraps around the entire joint.[5]
Radiocarpal joint fractures
Only 1% of upper extremity fractures in children and adolescents affect carpal bones. The scaphoid is the most commonly fractured carpal among children and adults. Scaphoid fractures often arise from injuries involving falling on outstretched arms (FOOSH). However, many carpal fractures go unreported. The carpus is cartilaginous and late to ossify, making these injuries challenging to detect on radiographs.
Scaphoid considerations
The scaphoid is the most lateral bone in the proximal carpal row. This carpal is covered by articular cartilage, which acts as an osseous bridge connecting the proximal and distal carpals. The scaphoid is the most commonly fractured carpal among adults and children. The radial artery (dorsal carpal branch) provides this bone's blood supply, flowing distally to proximally. Postfracture nonunion leaves the scaphoid's proximal portion susceptible to ischemia and avascular necrosis. Concern for preventing nonunion has made 7-to-8-week thumb spica casting the standard treatment for scaphoid fractures. Consensus on the management of other carpal fractures is currently wanting.[6]
Soft tissue considerations
The abductor pollicis longus and abductor pollicis brevis tendons control thumb abduction. The extensor pollicis longus and extensor pollicis brevis are the 2 muscles significantly controlling thumb extension. Hand function heavily depends on these motions. Traumatic injuries cause sprains and tendon ruptures, while repetitive use and overuse contribute to tendinopathies, such as tendinitis, tendinosis, and tenosynovitis.
De Quervain tenosynovitis is a tendinopathy involving the abductor pollicis longus and extensor pollicis brevis tendons as they pass through the 1st dorsal wrist compartment. The etiology was initially thought to be inflammatory. However, the condition now appears related to tissue and vascular changes. De Quervain tenosynovitis' pathophysiology is somewhat unclear. The tendon sheaths often thicken through a canal along the radial styloid, causing entrapment.[7] Tenosynovitis is associated with repetitive motion and acute trauma. Treatment includes thumb spica bracing, which may offer temporary pain relief, though success partly depends upon consistent use.[7]
The ulnar collateral ligament (UCL) stabilizes against varus and valgus stress on the 1st metacarpophalangeal (MCP) joint. UCL injuries, such as "gamekeeper's thumb" and "skier's thumb," often result from repetitive valgus motions when grasping objects between the 1st and 2nd digits. Traumatic thumb hyperabduction during falls and thumb contact during sporting events are other potential causes.[8] Thumb spica braces stabilize UCL injuries and prevent reinjury. These orthotic devices are also helpful when treating early-stage thumb base osteoarthritis with intraarticular steroid injection. However, splints have not demonstrated effectiveness in treating more advanced cases.[9]
Indications
The thumb spica splint is indicated in radial hand and wrist injuries, which include but are not limited to the following:
- Fractures and cartilage injuries
- Scaphoid
- Triquetrum [10]
- Hamate hook [11]
- Lunate [12]
- 1st metacarpal
- Soft-tissue injuries
- UCL
- De Quervain tenosynovitis [13][14]
- Closed thumb extensor and abductor tendon injuries [15]
- Degenerative conditions of the thumb
- Carpometacarpal thumb osteoarthritis (basal joint arthritis)
- Post-surgical stabilization
Notably, thumb spica splints are not indicated for carpal tunnel syndrome.
Contraindications
Thumb spica splinting has no specific contraindications. However, edema and tissue changes can give rise to pressure sores, tissue strangulation, and compartment syndrome.
Equipment
Thumb spica splints are available as malleable prefabricated and fiberglass types. Prefabricated splints may be used immediately and adjusted to the patient's hand size via movable straps. These splints are typically available in medical supply, sporting goods, and large chain grocery stores.
For fiberglass splints, the required equipment and materials include the following:
- Plaster or padded fiberglass
- Plaster wool
- Bucket of water
- Scissors
- Crepe bandage or stockinette
- Roll padding
- Nonsterile gloves
This list covers the equipment and materials required for creating fiberglass splints, ensuring proper immobilization and comfort for patients with hand or wrist injuries.
Personnel
Thumb spica splinting can be done in any traumatic, primary care, or emergency setting by a physician, nurse, or technician. A single individual can perform the process.
Preparation
Thumb spica splints can extend from the thumb to the mid-forearm or above the elbow. In the setting of a scaphoid fracture, using a long-arm thumb spica splint may lead to reduced union times in the first 4 to 6 weeks and diminish the radius and ulna's shearing forces on the scaphoid. However, by the end of the splinting period, both long and short-thumb spica splints will have equal efficacy in treating a scaphoid fracture.[16] A simple short-arm thumb spica splint is appropriate and effective for patients with 1st metacarpal fractures, such as Bennet and Rolando fractures.[17] However, controversy exists regarding the effectiveness of thumb spica splinting in treating De Quervain tenosynovitis with or without corticosteroid injection.
The splint must allow for balanced function and maximal mobility of the unaffected areas, including the fingers, upper arm, and shoulder. The orthotic device should also allow for maximal sensory perception. The splint's pressure should be distributed equally and not challenge the hand and forearm's normal contours. The patient should have adequate analgesia before and during splinting.
Technique or Treatment
The steps in applying a thumb spica splint are as follows:
- Perform a comprehensive physical examination before splinting.
- Have the patient rest their elbow on a table with the forearm in the neutral position.
- The thumb should be in the normal resting anatomic position.
- Put on nonsterile gloves.
- Apply a stockinette to the thumb.
- Place a second stockinette or crepe bandage over the affected arm from the MCPs to the forearm's middle or distal third, depending on the specific injury and desired splint length. Apply to the mid-forearm for a short splint and just distal to the elbow for a long splint.
- Wrap padding from the MCP joints to the forearm, covering an area slightly larger than the splinting target. Padding material should be torn intermittently to decrease the risk of compressing tissue.
- Wrap padding around the thumb over the top of the stockinette. Smooth the padding to remove folds.
- Take a 4-inch wide, 8-layer thick plaster large enough to cover the area from the tip of the thumb to the forearm.
- Soak the plaster in lukewarm water.
- Apply the plaster to the forearm and thumb's radial side. This plaster protects the area spanning from the thumb tip to the desired level on the forearm.[18][19]
- Ensure no ridges or indentations are created.
- Cover the plaster with a one-layer soft wrap material to interpose between the plaster and the most superficial wrap (eg, ace wrap).
- Repeat and document the neurovascular exam on the splinted area.
The patient should be instructed to keep the splint and treated extremity dry. Patients should also be informed of the possibility of complications, such as increasing pain, paresthesias, and skin color changes in the fingers. These symptoms may indicate compartment syndrome, a condition requiring immediate medical care. Patients should also be given clear follow-up instructions.
Complications
Compartment syndrome is the most consequential splinting complication. Patients should be educated regarding this condition's symptoms, such as worsening pain, numbness, tingling, and skin color changes. Less serious complications, including joint stiffness, thermal injuries, pressure sores, bacterial or fungal infections, and dermatitis, must also be explained during counseling. Splints should only be worn during the prescribed period or replaced if complications arise. Signs such as skin pallor, poor capillary refill, and pain on splinting may indicate that the orthotic device compromises the patient's normal anatomy.[20][21]
Clinical Significance
Thumb spica splinting has proven effective in treating bony and soft-tissue injuries of the lateral hand's thumb, carpal, and metacarpal. Splinting is cost-effective, easy to learn, and permissive to patients' often busy lifestyles. Splints are simple to manipulate for both the provider and the patient. Additionally, these orthotic devices are easy to remove when reassessing the injury's improvement throughout the treatment process.
At the end of the procedure, the provider should educate the patient on basic splint maintenance. The splint and hand must be kept clean and dry. The patient should be instructed to rest, ice, and elevate the affected area immediately postinjury to avoid swelling.[6] Follow-up is generally scheduled within 1 or 2 weeks from splinting, but this period can vary based on the treated injury's severity and type.
Enhancing Healthcare Team Outcomes
Hand and wrist injuries requiring thumb spica splinting are best managed with an interprofessional approach. Emergency medicine or primary care physicians are often the first to assess the condition, provide initial treatment, and refer for orthopedic care. Orthopedic or hand surgeons diagnose conditions requiring splinting and may perform surgical interventions if necessary.
Occupational, physical, or hand therapists specialize in upper extremity rehabilitation. These health professionals are responsible for assessing the patient's needs and providing guidance on splint wear and hand exercises. Cooperation with physical and occupational therapy has been shown to help prevent reinjury and significantly increase wrist strength 3 to 4 months postfracture.[22]
Orthotists may assist in fabricating or customizing splints based on the therapist's recommendations. Nurses may assist in splint application, patient education on splint care, and monitoring for splinting-related complications.
Managing a wrist or hand injury is not always straightforward. Extrinsic factors are often involved in the healing process, making it essential to view the patient holistically.
For example, hand and wrist injuries often keep patients out of work or prevent them from engaging in hobbies. Disability after an upper extremity injury has been reported to highly correlate with depression.[23] Patients must thus be monitored for signs of depression or emotional distress throughout the healing process. The patient may need to see a counselor or their primary care provider to assess their coping strategies and address their needs as appropriate. Early psychological intervention may improve healing and decrease disability in patients with orthopedic trauma.[24]
Collaboration among various team members ensures that the patient receives comprehensive care throughout the treatment process. Each member contributes their expertise to optimize outcomes and improve the patient's overall function and quality of life.
Patients should be reminded that good nutrition and adequate rest help optimize healing and reduce stress and the injury's mental health impacts. The importance of follow-up examinations must be emphasized, as progress can be better described after a second evaluation with or without imaging. Cultural and socioeconomic circumstances must be considered when creating follow-up plans.