Continuing Education Activity
Accidental hypothermia occurs when the body dissipates more heat than it absorbs or creates, leaving the body unable to generate sufficient heat to maintain homeostasis and proper bodily function. While the underlying cause of accidental hypothermia is excessive cold stress and inadequate heat generation from the body (thermogenesis), other factors increase the risk of developing hypothermia. This activity reviews the evaluation and management of hypothermia and highlights the role of interprofessional team members in collaborating to provide well-coordinated care and enhance patient outcomes.
Objectives:
- Describe the pathophysiology of accidental hypothermia.
- Identify the typical presentations of a patient with accidental hypothermia.
- Summarize the treatment options available for accidental hypothermia.
- Explain the importance of collaboration and communication amongst the interprofessional team to improve outcomes for patients affected by accidental hypothermia.
Introduction
The definition of hypothermia is an involuntary drop in body temperature below 35C. Accidental hypothermia is not limited to regions or times of severe cold and can occur in milder climates.[1] Symptoms will vary depending on the severity of hypothermia. Severity is defined based on core temperature as mild (32 to 35 C), moderate (28 to 32 C), and severe (under 28 C), with some experts also categorizing certain individuals with profound (less than 24 C) hypothermia. More severe symptoms, morbidity, and mortality are associated with worsening degrees of hypothermia.[2]
Etiology
Hypothermia takes place when the body dissipates more heat than it absorbs or creates, leaving the body unable to generate sufficient heat to maintain homeostasis and proper bodily function. While the underlying cause of accidental hypothermia is excessive cold stress and inadequate heat generation from the body (thermogenesis), other factors increase the risk of developing hypothermia. Functional central and peripheral nervous systems, along with proper behavioral adaptation, are important components.[3]
Extremes of age, hypoglycemia, malnutrition, and endocrine disorder are examples of heat production inadequacy. Skin disorders (psoriasis and burns) and improper peripheral vasodilation from peripheral dysfunction (peripheral neuropathies and spinal cord injuries) exacerbate heat loss. Cerebrovascular accidents, neurodegenerative disorders, and drug abuse may disrupt the hypothalamic thermoregulation function. In addition to organic causes, impaired behavioral response to cold stress may result in hypothermia for individuals with dementia, drug abuse disorder, or psychiatric condition. Situational circumstances from lack of shelter or clothing may occur in the homeless.[4][5][3][2]
Hypothermia may also be due to drugs like general anesthetics, beta-blockers, meperidine, clonidine, neuroleptics, and alcohol.
Epidemiology
Each year there are approximately 700 to 1500 patients in the United States who have hypothermia noted on their death certificate.[4] Adults between the ages of 30 to 49 are more likely affected, with men being ten times more likely than women. However, the true incidence of hypothermia is relatively unknown. Even with supportive in-hospital care, the mortality of those with moderate to severe hypothermia still approaches 50 percent.[4]
Pathophysiology
Core temperature is a balance between heat produced by the body and heat loss to the surrounding environment. The normal average temperature of an individual is 37+/-0.5 C. Heat loss occurs through four mechanisms: radiation, conduction, convection, and evaporation. Radiation occurs when electromagnetic energy transfers between each other. Conduction occurs when the heat gets transferred between two objects that are in contact with one another. Convection is heat loss that occurs when air molecules move past an object. Evaporation is an endothermic reaction that causes a liquid to form a gas. While radiation is the most common form of heat loss, the most common mechanism of developing accidental hypothermia is by convective heat loss to cold air and when in cold water or wet clothing via immersion or excessive sweating.[6][2]
Body temperature regulation is by the hypothalamus and gets maintained by a variety of autonomic mechanisms. The hypothalamus receives input from central and peripheral thermal receptors. In response to increased cold stress, the hypothalamus will work to raise its metabolic heat production through a variety of mechanisms. Initial muscle tone and basal metabolic rate increase, which can double heat production. Shivering can also increase the heat production rate 2 to 5 times from baseline. There will also be an increase in thyroid activity, catecholamines, and adrenal response. The body will also try to avoid further heat loss through sympathetically mediated cold-induced vasoconstriction of peripheral vessels where cooling and heat loss are often the greatest. Additional heat production results from behavioral changes such as adding more clothing, seeking shelter, starting a fire, and exercising.[1][3]
The body initially increases metabolism, ventilation, and cardiac output in an effort to maintain bodily function during drops in temperature. Eventually, the heat loss overwhelms the body, and shivering ceases. Multiple organ systems, including neurologic, metabolic, and cardiac, will stop functioning and ultimately lead to death.[7] Arrhythmias can occur with the sinoatrial node being affected, resulting in atrial fibrillation. Ventricular fibrillation is also common.
Newborns lack the shivering mechanism. The lack of shivering is due to an immature nervous system. Brown fat helps create heat in the newborns. Brown fat makes the inner membrane of the electron transport chain permeable. The permeability is produced by the thermogenin in the brown fat. The permeability causes the leakage of hydrogen ions. The leakage of hydrogen ions from the electron transport chain will dissipate as heat instead of producing ATP.
History and Physical
Those suffering from accidental hypothermia will typically have a history of cold exposure. Obtaining a core temperature is essential to diagnose and manage hypothermia effectively. Oral temperature is only useful to rule out hypothermia as most commercially available thermometers cannot read under 35 C. Tympanic thermometers are also unreliable. Epitympanic thermometers, when used correctly, reflect the carotid artery temperature and can be reasonably reliable. Both rectal and bladder temperature measurements are reasonable in conscious individuals with mild to moderate hypothermia but may not be appropriate for critical patients during rewarming as they lag behind true core temperature. Neither are they appropriate in the pre-hospital setting as they may further expose the patient and cause a further drop in temperature. Esophageal temperature measurement is the most accurate when done correctly with the probe in the lower third of the esophagus; this should only be performed in patients with an advanced airway in place.[1] Given the difficulty of getting an immediate, reliable temperature in a pre-hospital setting, it is crucial to know the clinical findings associated with the stages of hypothermia so that appropriate treatment can initiate immediately.[6]
Mild Hypothermia 32 to 35 C: Presentation can often be subtle with vague symptoms such as hunger, nausea, fatigue, shivering, and pale-dry skin. Often, they will have increased muscle tone, increased blood pressure, tachycardia, and tachypnea from the body’s attempts to promote thermogenesis. Patients are frequently shivering, but if energy stores have been depleted, they may not be shivering, meaning you cannot rely on this finding. They will often have a decline in cognitive abilities, memory, and judgment, with some experiencing ataxia and dysarthria. The patient may experience “cold diuresis” due to peripheral vasoconstriction leading to increased diuresis and volume depletion.[1]
Moderate Hypothermia 28 to 32 C: The patient will continue to have cognitive decline and be lethargic. Increased CNS depression may lead to hyporeflexia with pupils less responsive and dilated. They may become hypotensive with bradycardia and bradypnea. Shivering typically ceases between 30 to 32 C, and paradoxical undressing may be observed. Susceptibility to dysrhythmias increases, with atrial fibrillation being the most common.[7]
Severe Hypothermia, less than 28 C: Cerebral blood flow continues to decline until patients become unresponsive. Blood pressure, heart rate, and cardiac output continue to decrease. Increased susceptibility to atrial and junctional dysrhythmias is present. Pulmonary congestion, extreme oliguria, and areflexia may occur. Ultimately, cardiorespiratory failure results.[8]
All patients with suspected hypothermia should have a complete history and physical exam to exclude local cold-induced injuries and assess for signs of trauma or other illness that may have caused their exposure to the cold. Also, be aware of vital signs inconsistent with the degree of hypothermia as this may be the only clue to an alternate diagnosis such as hypothyroidism, adrenal insufficiency, sepsis, hypoglycemia, carbon monoxide poisoning, alcohol abuse, malnutrition, unintentional/intentional overdose.[4]
Hypothermia may be related to medications including beta-blockers, clonidine, neuroleptics, meperidine, and general anesthetic agents. Ethanol, sedative-hypnotics, and phenothiazines also reduce the body's ability to respond to low ambient temperatures. Beta-blockers may blunt the effects of the catecholamine surge.
Evaluation
As with all potentially unstable patients, the initial focus of the clinician should remain on assessing the patient's ABCs. Once the ABCs have been evaluated and managed, the patient should be exposed to remove all clothing. Warm blankets should then be placed over the patient once he/she is fully exposed. Standard laboratory evaluation should include finger-stick glucose, complete blood count, a metabolic panel with basic serum electrolytes, BUN, and creatinine. One may expect increased hemoglobin and hematocrit in hypothermic patients due to cold diuresis from impaired secretion of antidiuretic hormone. Electrolyte reassessment approximately every 4 hours is the recommended procedure when resuscitating the moderate to severely hypothermic patient. Glucose also does not follow a specific pattern but maybe the earliest clue for a patient in DKA.[4]
In moderate to severely hypothermic patients in whom invasive procedures may be necessary, it is reasonable to obtain a coagulation panel to rule out coagulopathy. However, coagulation studies generally require blood warmed to 37 C, so it does not accurately reflect actual function. Fibrinogen should also be checked to rule out disseminated intravascular coagulation. Serum lactate, creatinine kinase, troponin, TSH, cortisol, toxicology screen, fibrinogen, lipase, magnesium, and any other labs deemed necessary may be necessary under the right clinical settings.[3][8]
Imaging should be dictated by clinical scenarios as some patients may have experienced trauma, cerebrovascular accident, or other events that led to prolonged cold exposure. If obtaining a chest X-ray, it is not uncommon for severely hypothermic patients to show signs of pulmonary edema. Bedside ultrasound can be used to confirm cardiac activity and volume status. Head CT may be beneficial for individuals whose mental status is not consistent with measured core temperature or if there is a concern for trauma.[8]
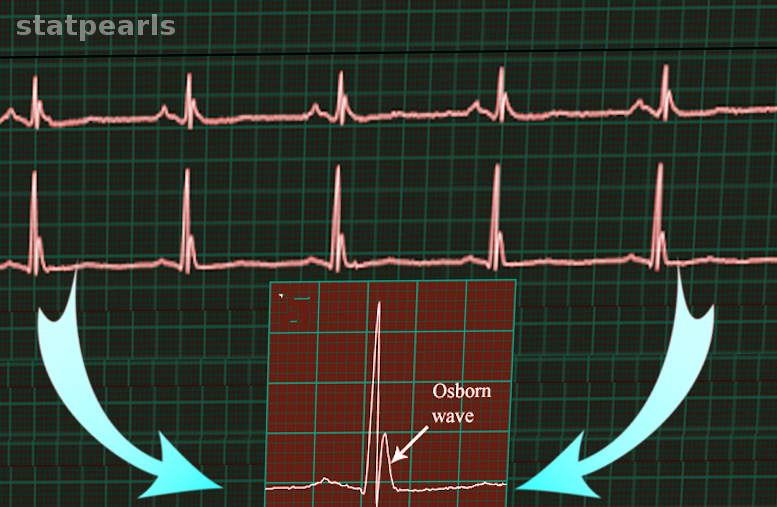
Due to the different dysthymias that often present in hypothermic patients, an ECG is necessary. Hypothermia can cause slowed impulse conduction through potassium channels resulting in prolonged ECG intervals. There may also be an elevated J point that can produce an Osborne or J wave. The height of this wave is proportional to the degree of hypothermia and is most common in the precordial leads. Any dysrhythmia is possible, with atrial fibrillation being the most common. Those with more moderate to severe hypothermia will likely exhibit bradycardia and are at increased risk for ventricular arrhythmias.[4][5]
Treatment / Management
The management and treatment of accidental hypothermia revolve around the prevention of further heat loss and the initiation of rewarming. However, the initial steps are always to evaluate and support airway, breathing, and circulation. Wet clothing should be removed and replaced with dry clothing or insulation as soon as possible to prevent further heat loss.[9]
Once able, one should then attempt to determine the degree of hypothermia based on history, mental status, physical exam, and core temperature measurement. If there is suspicion for moderate or severe hypothermia, especially in those with a decreased level of consciousness or in those who have an irregular or faint pulse, extra care should be taken not to move or jostle the patient too much as it may precipitate cardiac collapse from a fatal arrhythmia due to increased cardiac irritability. Comorbid medical conditions and trauma that may also have occurred merit considerations and appropriate treatment.[10] Ventricular fibrillation is a common arrhythmia in hypothermia with a very favorable neurological outcome if ACLS protocol is followed immediately. Asystole as a result of hypothermia is generally refractory to normal ACLS protocol treatment. The patient may require warming to 35°C before normal cardiac arrhythmia is achieved. Patients with severe hypothermia have a poor prognosis. If a patient is in asystole and not responding to treatment, electrolytes should be drawn. Potassium greater than 12 mEq/L is an indication of irreversible tissue death and cell lysis.
Rewarming of hypothermic patients involves passive external rewarming, active external rewarming, active internal rewarming, or a combination of these techniques. The treatment of choice for mild hypothermia is passive external rewarming. After the removal of wet clothing, additional layers of insulation are placed on the patient with the goal to prevent heat loss and promote retention of heat produced by patients. Shivering allows the body to spontaneously produce up to a 5-fold increase of heat as compared to baseline. However, the success of this method requires adequate glucose stores so that a patient can produce heat. Given that at this point, many will have depleted energy reserves (more so in elderly, young, and malnourished), it is appropriate to supply glucose to these individuals orally when possible. In individuals with mild hypothermia, it is recommended to warm them at 0.5 to 2 C per hour. Vigorous shivering, however, can be problematic in people with limited cardiopulmonary reserve as it requires an increase in the consumption of oxygen. Furthermore, patients with more severe hypothermia may fail to respond to passive techniques, so it is appropriate to progress to active external rewarming techniques.[8]
Active external rewarming is necessary for moderate to severe hypothermia and, in some cases of mild hypothermia, not responding to standard measures. A heated air unit can decrease heat loss and transfer heat through convection. Water immersion is an alternative, but it is more cumbersome and harder to monitor. Immersion of extremities in warm water (44 to 45 C) requires great care and attention, as efforts to rewarm patients may precipitate increases CV load and collapse as peripheral vasodilation may lead to an after-drop cooling of core temperature from sudden return of cold blood from the extremities.[8]
Despite active external rewarming, some patients may require more invasive methods ranging from airway rewarming with humidified air to full cardiopulmonary bypass. Most patients will be started on warm intravenous fluids of 40 to 42 C as they are readily available and safe, as well as humidified air. Lavage of body cavities such as stomach, bladder, colon, peritoneal and pleura with warm fluid, though invasive, can be considered. Pleural and peritoneal lavages are preferable due to the larger mucosal surface area. Pleural lavage involves placing one thoracostomy tube between the second and third anterior intercostal space in the midclavicular line and the second thoracostomy tube between the fifth and sixth intercostal space at the posterior axillary line. Warm fluid infusion will begin at the anterior tube and drain through the more posterior tube. Peritoneal lavage involves the placement of two or more catheters in the peritoneal cavity, which allows for the diagnostic of occult abdominal trauma and rewarming peritoneal cavity. Extracorporeal rewarming techniques allow for even faster rewarming.[5][7]
Extracorporeal methods, including hemodialysis, continuous arteriovenous rewarming, cardiopulmonary bypass, and extracorporeal membrane oxygenation (ECMO). Hemodialysis is the most accessible and can raise the core temperature 2 to 3 C per hour. In arteriovenous rewarming, the patient’s blood pressure creates movements of blood from the femoral artery through a countercurrent fluid rewarmer and into the contralateral femoral vein. It is capable of raising the temperature by 4.5 C per hour. However, hemodialysis and AV rewarming require the patient to have adequate blood pressure. Cardiopulmonary bypass surgery and venoarterial ECMO is the most effective but highly invasive method of rewarming a patient. These methods are only for hypothermic patients in cardiac arrest, those patients refractory to other rewarming techniques, and hemodynamically unstable patients. It is capable of raising core temperature by 7 to 10 C per hour. It is an ideal option for cardiac arrest, as it simultaneously provides rewarming, oxygenation, and circulatory support. However, it is not readily available and requires systemic anticoagulation.[1][4][8]
Differential Diagnosis
Primary hypothermia
Secondary Hypothermia
- Central failure
- Cerebrovascular accident
- CNS trauma
- Hypothalamic dysfunction
- Metabolic failure
- Toxins
- Pharmacologic effects
- Peripheral failure
- Acute spinal cord transection
- Neuropathy
- Endocrinologic failure
- Alcoholic or diabetic ketoacidosis
- Hypoadrenalism
- Hypopituitarism
- Lactic acidosis
- Insufficient energy
- Hypoglycemia
- Malnutrition
- Neuromuscular compromise
- Extreme ages with inactivity
- Impaired shivering
- Dermatologic
- Burns
- Medication and toxins
- Iatrogenic cause
- Emergency childbirth
- Cold infusion
- Heat-stroke treatment
- Other[11]
- Carcinomatosis
- Cardiopulmonary disease
- Major infection
- Multisystem trauma
- Shock
Prognosis
Severe hypothermia can be lethal; however, the prognosis may be favorable depending on the scenario. Patients with primary hypothermia and cardiac stability that receive proper treatment with active external and minimal invasive rewarming techniques have a survival rate of approximately 100% with full neurological recovery. For those patients that suffer cardiac arrest who then receive extracorporeal rewarming, the survival rate approaches 50%. Full recovery might be possible in cardiac arrest with extracorporeal rewarming if there were no preceding hypoxia, serious underlying disease, or trauma. Full neurological recovery has been witnessed in accidental hypothermia of up to 14 C.[11]
Frostbite is a complication of hypothermia. It is a form of dry gangrene. When gangrene becomes infected, it becomes wet gangrene. Wet gangrene that has crepitus indicates a gas-producing organism. Clostridium perfringens classically cause superinfections with crepitus.
Complications
Depending on the severity of hypothermia, the following may result[7]:
- Cold diuresis
- Rhabdomyolysis
- Aspiration
- Hyperkalemia
- Frostbite
- Acute kidney injury
- Pulmonary edema
- Ataxia
- Arrhythmia (A. fibrillation, ventricular arrhythmia, PEA)
- Coma
- Pancreatitis
- Death
Deterrence and Patient Education
Hypothermia occurs when your body can no longer produce enough heat to overcome cold exposure. Hypothermia is an extremely dangerous entity that has the potential to lead to death if not treated quickly. Luckily, hypothermia is avoidable. Individuals should not stay outside for too long if the weather is cold, and if outside during such an arduous climate, proper clothing is critical. If your clothes are wet, quickly change out of them.
Certain patient populations are at a higher risk of developing hypothermia. Infants and young children are at increased risk due to their underdeveloped bodies and their inability to communicate reliably. On the other end of the age spectrum, the elderly are also at higher risk, as they tend to have multiple comorbidities. Physical and cognitive limitations could prevent them from seeking warmer environments in certain situations.
Pearls and Other Issues
- Most commercial thermometers are only able to read down to 34 C, so a special low-reading thermometer is required to assess the exact level of hypothermia.
- The esophageal thermometer is the most accurate way to determine a patient’s temperature.
- Rectal temperatures take up to 1 hour to adjust for changes in core temperature.
- The pulse oximeter may be inaccurate if placed on the fingers due to peripheral vasoconstriction during hypothermia.
- Patients with hyperkalemia may not show normal ECG changes associated with elevated potassium.
- The coagulation panel performed in the lab may not accurately represent actual coagulopathy in a hypothermic patient as it is normally warmed to 37C before being run.
- J waves are associated with hypothermia, subarachnoid hemorrhage, ACS, and normal variant.
- ECMO and cardiopulmonary bypass are the most invasive but effective ways to rewarming an unstable patient.
- If central access is necessary, a femoral CVL is preferred due to less irritation of the myocardium and risk of dysrhythmia.
- If the patient fails to rewarm despite appropriate rewarming techniques, secondary hypothermia such as hypoglycemia, infection, hypothyroidism, and adrenal insufficiency merit investigation.
Enhancing Healthcare Team Outcomes
Hypothermia is potentially lethal if not quickly recognized and treated. The majority of patients first present to the emergency department, and the triage nurse should promptly accept the patient and inform the emergency department physicians. In general, treating patients with hypothermia requires an interprofessional team of healthcare professionals.
EMS personnel provide the initial encounter and resuscitation effort. They will remove wet clothing and initiate external passive rewarming. After reaching the hospital, nurses and emergency room physicians will work together to further warm the patient with external and internal invasive rewarming methods.
Hypothermic patients are prone to many complications and require admission to the ICU, where there will be continuous monitoring by the nurses. The pulmonologist and cardiologist should be involved if the patient has pulmonary edema or aspiration pneumonia. Since frostbite is a common outcome, wound care must take part in therapy. Regular debridement of the wound may be necessary. Blood work requires monitoring for rhabdomyolysis. Nursing must remain in attendance constantly and report any deterioration in condition to the physician staff, as well as administering fluids and any medications.
Nephrologists, surgeons, and cardiology may be required if ECMO, hemodialysis, or cardiopulmonary bypass is needed.[8]
Hypothermia is a medical emergency and requires an interprofessional team approach, including physicians, specialists, specialty-trained nurses, and pharmacists, all collaborating across disciplines to achieve optimal patient results. [Level V]
For those who survive, education is necessary to prevent a repeat episode. These individuals should avoid alcohol, dress appropriately, and carry a survival bag with the essential equipment and material to protect the body. Only through an interprofessional team approach can be morbidity of hypothermia be lowered.
Outcomes
Patients who receive rapid resuscitation usually have good results, but residual frostbite and muscle injury may be present. Outcomes are worst for the very young and elderly.