Continuing Education Activity
Midshaft humeral fractures usually occur due to a direct blow to the upper arm, which commonly results from falls, motor vehicle accidents, or motorcycle accidents. In the elderly, this fracture can also occur due to a fall on an outstretched arm. This activity outlines the cause of midshaft humeral fractures, reviews their evaluation and management, and highlights the role of the interprofessional team in managing patients with this condition.
Objectives:
- Describe the etiology of humeral shaft fractures.
- Describe the presentation of a patient with a humeral shaft fracture.
- List the treatment and management options available for humeral shaft fractures.
- Employ interprofessional team strategies for improving care coordination and communication to advance the treatment of humeral shaft fractures and improve outcomes.
Introduction
A direct blow commonly causes fractures that occur in the middle third of the shaft of the humerus. Humeral shaft fractures account for about 3% of all fractures. These fractures are classified based on their location, open or closed status and the type of fracture line. The majority of humeral shaft fractures are unstable but non-surgical treatment is the standard of care.
Etiology
The humeral shaft is surrounded by large arm muscles, blood vessels and include the following:
Anterior compartment:
- Brachial artery and vein
- Biceps brachii, brachialis, coracobrachialis
- Musculocutaneous, median and ulnar nerves
Posterior compartment:
A fracture that occurs at the midshaft of the humerus usually occurs due to a direct blow to the upper arm. Most frequently, fractures are a result of trauma, such as a fall, motor vehicle accident, or motorcycle accident. In the elderly, it can also occur from a fall on the outstretched arm, where the humerus takes the brunt of the injury instead of the wrist.[1][2][3]
Epidemiology
Peak incidence occurs in males aged 21 to 30 and females aged 60 to 80, although a humerus fracture could happen in persons of any age or gender with the right mechanism of injury. Sixty percent of all humeral fractures occur in the middle-third of the humerus.[4]
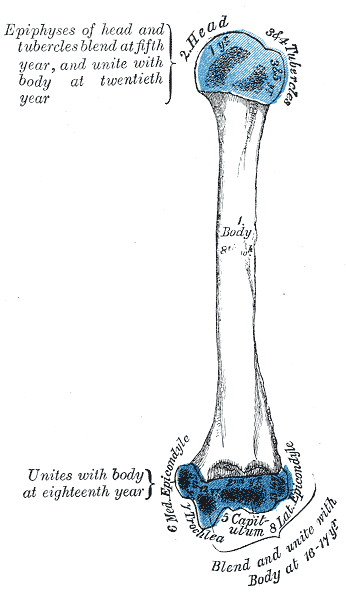
Pathophysiology
The most important clinical pearl associated with midshaft humerus fractures involves injury to the radial nerve. Radial nerve injury occurs in approximately 18% of closed mid-shaft or distal shaft humerus fractures. In closed fractures, radial nerve injury is most commonly an incomplete neuropraxia rather than a complete laceration of the nerve. In open humerus fractures, the incidence of radial nerve laceration is much higher at 60%.[5][6][7]
The radial nerve originates in the brachial plexus and has nerve roots from C5 to T1. It crosses through the spiral groove on the posterior side of the humerus shaft. The spiral groove is located about 14 cm proximal to the lateral epicondyle and 20 cm proximal to the medial epicondyle. The radial nerve is most likely to be damaged in humerus fractures that have a lateral displacement of the distal fracture segment, as the nerve is tethered to the bone and cannot withstand the forces applied to it as a result of the displacement. On physical exam, patients with a radial nerve injury may have wrist drop (loss or weakness of wrist extensors), loss or weakness of finger extension, and decreased or absent sensation to the posterior forearm, digits 1 to 3, and the radial half of the fourth digit. Up to 90% of patients with a closed humeral fracture with radial nerve injury will have a resolution of neuropraxia within three to four months following the injury.
Of note, radial nerve paralysis is rare in children with humeral fractures, though neuropraxia can still occur, also with a resolution of symptoms in three to four months.
It is also very important to confirm that the patient’s distal pulses and capillary refill are intact, as the brachial artery also traverses the humerus in proximity to the radial nerve and the above listed anatomic landmarks.
History and Physical
Patients will present with arm pain after traumatic injury. Also, patients may have a deformity to the upper arm, shortening of the extremity, swelling, and/or bruising. On exam, it is important to evaluate for skin tenting, motor function distal to the injury, sensation distal to the injury, and pulse and/or capillary refill distal to the injury. One should also evaluate the skin integrity; if there is an overlying laceration, it is classified as an open fracture. As with any fracture, one must also confirm that the limb is neurovascularly intact distal to the injury due to the risk of radial nerve and brachial artery injury, as described above.
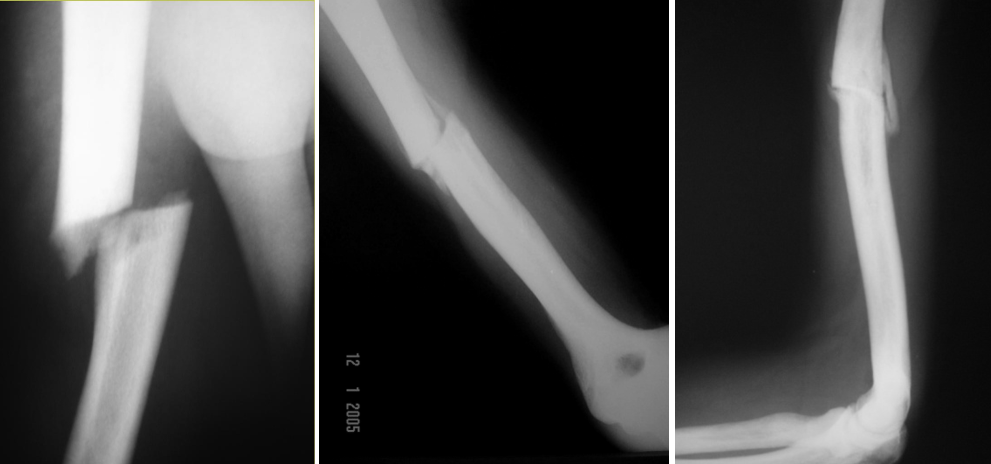
Evaluation
Radiographic imaging of the affected upper arm with a minimum of two views should be obtained if the humeral fracture is suspected. Also, one should have a high suspicion of forearm, wrist, or clavicle fracture when a patient has a humeral fracture due to the mechanism of injury; thus, imaging of these areas should be considered as well. If the patient has evidence of vascular injury or a large hematoma, hemoglobin should be obtained to ensure there is no significant blood loss due to the injury. Of note, there can be significant blood loss associated with any long bone injury. Also, if urgent or emergent surgery is anticipated, basic screening labs, such as complete blood count (CBC) and complete metabolic panel or basic metabolic panel (CMP/BMP) may be obtained in the preparation of the patient going to the operating room and undergoing anesthesia. A prothrombin time or INR should be obtained on patients who are anticoagulated on warfarin.
Vascular imaging is rarely indicated. Treatment for vascular compromise is a definitive reduction of the joint. Angiography only delays definitive management and does not add any additional information nor alter management.
With radial nerve injury, electromyography (EMG) may be used in the subacute or long-term phase to assess the extent of nerve damage.
Treatment / Management
Management of midshaft humerus fractures is historically conservative, meaning reduction and splint. There is an approximately 90% rate of appropriate alignment and union with conservative management.[8][9][10]
A reduction should be performed more urgently if there is a loss of pulse distal to the injury or skin tenting. The reduction should not be performed without adequate pain control and/or sedation. Any overlying breaks in the skin (lacerations, abrasions, or skin tears) should be addressed before splinting of any kind. Splinting of a humerus fracture presents challenges to immobilization due to its location. As with any splint, the joint above and below the fractured bone should be immobilized, so for humerus fractures, this includes the elbow and shoulder. Appropriate splinting options for a humerus fracture would include a coaptation splint with a sling, a hanging arm cast, a long arm splint, or a shoulder immobilizer. If one is going to be performing procedural/conscious sedation, reduction, and splinting, all splinting material should be prepared and readily available in the patient’s treatment room before sedation.
Upon follow-up with an orthopedic specialist after the initial injury, a more long-term cast may be applied to immobilize the fractured extremity if conservative management is the approach of choice. This is done ten to 12 days following the date of injury.
Some indications for operative management include neurovascular injury, open fractures, comminuted fractures, inability to tolerate a splint/cast for a prolonged period, trauma with multiple fractures, other fractures to the same arm, or failed conservative treatment with nonunion of the fracture site. Conservative treatment is associated with a healing time of up to ten to 12 weeks with transverse or comminuted fractures taking longer to heal than spiral or oblique fractures. Operative management, however, is becoming increasingly popular outside of these indications due to more prompt healing times and the better promise of appropriate alignment and union.
Humeral shaft fractures take at least 4 months to heal and have a nonunion rate of 1-12%. Higher rates of nonunion are associated with transverse fractures, inadequate shoulder mobilization, and soft tissue interposition.
Differential Diagnosis
Staging
Classification
- Type A: Simple fractures that may be spiral, oblique or transverse
- Type B: Wedge fractures may be intact of fragmentary.
- Type 3: Multifragmentary fractures
Prognosis
The prognosis for humeral shaft fracture is good with nearly 90% achieving a satisfactory union. However, with conservative treatment, the time to union may vary from 3-5 months. Hospitalization is sometimes needed for elderly patients.
Complications
Complications after humeral shaft fracture include the following:
- Non-union
- Angulation
- Limited range of motion
- Infection
- Nerve injury
Radial nerve injury occurs in close to 20% of patients with humeral shaft fractures. The majority of these nerve injuries are neurapraxic or axonotmetic and resolve within 6 months. Brachial artery injuries are rare but can occur. Rates of nonunion are increased in patients with advanced age, obesity, diabetes, poor nutrition, and prior radiation exposure
Enhancing Healthcare Team Outcomes
Midshaft humeral fractures are best managed by an interprofessional team that includes an orthopedic surgeon, emergency department physician, nurse practitioner, radiologist, and therapist. The majority of these fractures are managed non-surgically and hence clinicians should know the follow-up protocol. Once the cast is removed, physical therapy is required to restore muscle strength and range of motion. The pharmacist should educate the patient on pain management. The key is to ensure that there is no injury to the radial nerve. The majority of these fractures are managed non-surgically with casting. Extensive rehabilitation is required to regain muscle mass and strength once the fracture has healed. Serial x-rays are necessary and all patients with non-union should be referred to an orthopedic surgeon for more definitive management. Open communication between the team is essential to enhance patient outcomes.