Continuing Education Activity
Carpal instability resulting from ligamentous injury is a broad and complex topic with several potential etiologies. Acute or repetitive wrist trauma can cause tearing or progressive insufficiency of key intercarpal ligaments, which can lead to static or dynamic carpal instability. Without appropriate treatment, carpal ligament injury may alter the intrinsic mechanics of the wrist and lead to painful and possibly debilitating complications. Carpal instability should be differentiated from carpal misalignment, wherein carpus alignment may show deviation from normal radiographic parameters, but the joints remain stable when loaded under physiologic conditions.
This activity for healthcare professionals discusses the most common carpal instabilities and their sequelae, focusing on dorsal intercalated segment instability characterized by scapholunate dissociation and volar intercalated segment instability due to lunotriquetral dissociation. This activity reviews the anatomy, pathophysiology, clinical characteristics, evaluation, and treatment of these causes of carpal instability while highlighting the role of the interprofessional team in improving outcomes for patients with these potentially debilitating disorders.
Objectives:
Identify the etiology and pathophysiology of carpal ligament instability.
Apply best practices when evaluating a patient with carpal ligament instability.
Differentiate the nonoperative and operative management options for carpal ligament instability.
Collaborate with the interprofessional team for timely diagnosis to enhance care delivery for patients affected by carpal ligament instability.
Introduction
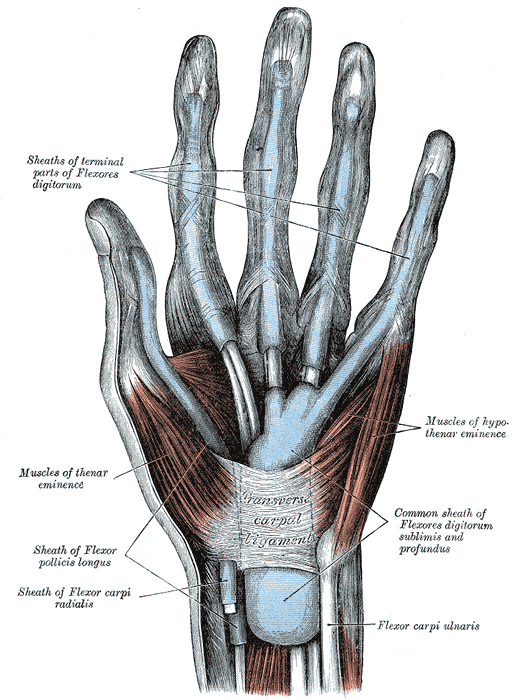
Carpal instability occurs when the carpus cannot maintain normal alignment and mechanics under physiologic loads, most commonly resulting from tearing or progressive insufficiency and laxity of key stabilizing intercarpal ligaments (see Image. Muscles and Fascia of the Hand). Instability, however, should be differentiated from carpal misalignment, wherein the carpus may show deviation from normal radiographic alignment, but the joints remain stable when loaded under physiologic conditions.[1]
The Mayo Clinic Classification is commonly used to stratify and characterize carpal instability, dividing carpal instability into 4 categories.[2]
Carpal instability dissociative (CID) describes carpal dysfunction between bones within the same carpal row. This includes scapholunate dissociation and lunotriquetral dissociation.
Carpal instability nondissociative (CIND) results from instability between the proximal and distal carpal row or proximal row and radius. This includes radiocarpal, mid-carpal, volar intercalated segment instability (CIND-VISI), and dorsal intercalated segment instability (CIND-DISI).[3][4] The direction of the lunate, which is considered the intercalated segment, relative to the axis of the radius determines whether DISI or VISI is present. For example, if the lunate is extended, there is DISI.[3] DISI or VISI deformities can occur due to chronic scapholunate or lunotriquetral dissociation, respectively. In this context, the DISI or VISI represents a dissociative malalignment.
Carpal instability combined (CIC) results from perilunate or axial dislocations. It has features of both CID and CIND.[3] CIC can also be divided into dynamic and static instability. Dynamic instability refers to a deformity that only occurs during motion, while static instability can be seen with the wrist at rest in a neutral position.[2]
Carpal instability adaptive (CIA) is malalignment and instability due to extrinsic deformities such as distal radius malunion, and it may appear similar to mid-carpal CIND.
Due to the many variations of carpal instability, this review focuses on the 2 most common etiologies: scapholunate and lunotriquetral dissociations.
Wrist Anatomy
The osteology of the wrist includes the distal radius, distal ulna/ulnar head, and 8 carpal bones. The distal radial articular surface contains a triangular scaphoid fossa and a rectangular lunate fossa. The articular surface is tilted on the ulnar aspect by approximately 23° (range, 15°-35°) and on the volar aspect by about 11° (range, 0°-20°).[5] The proximal carpal row comprises the scaphoid, lunate, triquetrum, and pisiform. There are no direct tendon attachments to the proximal row. The distal carpal row includes the trapezium, trapezoid, capitate, and hamate. The bones of the distal carpal row have minimal motion between them compared to the proximal carpal row. The flexor and extensor tendons of the forearm are inserted into the distal carpal row.
The carpal bones can also be divided into columns. The radial column consists of the scaphoid, trapezium, and trapezoid. The central column contains the lunate and capitate. The ulnar column comprises the hamate and triquetrum.[6]
The wrist contains a complex organization of ligaments. The ligaments are classified as extrinsic, connecting the distal forearm to the carpus, or intrinsic, originating and inserting between carpal bones. This review focuses on the ligaments of the scapholunate and lunotriquetral joints.[6]
Scapholunate Joint
The scapholunate ligamentous complex stabilizes the scapholunate joint. The scapholunate (intercarpal) ligament is a C-shaped intrinsic ligament consisting of dorsal, palmar, and membranous components. The dorsal component is the thickest (up to 3 mm) and provides the most stability against distraction, torsion, and translation. The thinner palmar component provides restraint against rotational forces.[7] The dorsal component merges with the dorsal intercarpal ligament, which originates on the dorsal ridge of the triquetrum and inserts on the dorsal rim of the scaphoid, trapezium, and trapezoid. The dorsal intercarpal ligament is a secondary stabilizer of the scapholunate joint as it indirectly prevents the proximal pole of the scaphoid from flexing and moving dorsally.[8] Additional secondary stabilizers of the scapholunate joint include the radioscaphocapitate, scaphocapitate, long radiolunate, and scaphotrapeziotrapezoid ligaments, as well as the flexor carpi radialis and ulnaris tendons.[7][9][10]
The radioscaphocapitate ligament originates from the anterolateral distal radius and inserts onto the palmar capitate, forming a sling around the scaphoid waist. The scaphocapitate ligament originates from the volar distal scaphoid and inserts onto the waist of the capitate, just distal to the insertion of the radioscaphocapitate ligament. The scaphotrapeziotrapezoid ligament originates from the distal pole of the scaphoid and has volar and dorsal contributions to the trapezium and trapezoid. The latter 2 ligaments stabilize the distal pole of the scaphoid. In the sagittal plane, the lunate is in relative neutral alignment compared to the axis of the forearm. The proximal lunate is narrower dorsally, resulting in its propensity to move into extension if ligamentous stabilization is disrupted. The scaphoid has an oblique orientation in the sagittal plane at a mean of 45° of flexion (range, 30°-60°) relative to the radius. As a result, the scaphoid tends to move further into flexion if there is a ligamentous compromise.[6]
Lunotriquetral Joint
The lunotriquetral ligamentous complex primarily stabilizes the lunotriquetral joint. Like the scapholunate ligament, the lunotriquetral ligament has 3 components: dorsal, palmar, and membranous. The palmar component is the thickest and strongest, while the dorsal component mainly assists in rotatory stability. However, the triquetrum has more robust ligamentous insertions compared to the scapholunate ligamentous complex insertions.[3] Lunotriquetral dissociation is less common than scapholunate dissociation.
This difference in ligamentous insertion on the triquetrum may help explain why injury to the lunotriquetral ligamentous complex is more stable than the scapholunate ligamentous complex injury.[3] Secondary stabilizers of the lunotriquetral joint include the dorsal radiocarpal and scaphotriquetral ligaments.[11][12] The dorsal radiocarpal ligament is the only extrinsic ligament that connects the dorsal radius to the dorsal carpus. It originates from the ulnar dorsal rim of the distal radius and inserts on the dorsal triquetrum and lunate to prevent the lunate from moving into flexion.
Carpal Mechanics and Motion
The long axis of the scaphoid runs obliquely to that of the radius.[13] Therefore, with radial deviation, the scaphoid is pushed into flexion by the distal carpal row as the trapezium and triquetrum approximate the distal radius. To a lesser extent, the lunate and triquetrum move into flexion through the intact scapholunate and lunotriquetral ligaments. With ulnar deviation, the scaphoid is pulled into extension by the scaphotrapeziotrapezoid ligament. The lunate and triquetrum then follow the scaphoid into extension.[14][15]
Etiology
Scapholunate Dissociation
Scapholunate ligament injury typically results from trauma due to a fall onto an extended and ulnar-deviated hand.[3][16] Scapholunate dissociation can also result from atraumatic causes such as infection, inflammatory arthritis, neurological disorders including syringohydromyelia, and certain congenital malformations such as a Madelung deformity, that can lead to disruption of the primary and secondary ligamentous stabilizers of the scapholunate joint.[3] Acute intra-articular fractures and radiocarpal fracture dislocations can also cause radiocarpal ligament injury and articular incongruity, leading to nondissociative carpal instability.[17]
Lunotriquetral Dissociation
Isolated injuries to the lunotriquetral ligament can occur from a fall on an outstretched hand with the wrist in extension and radial deviation where force is applied to the hypothenar eminence region.[18] Atraumatic causes of lunotriquetral dissociation include inflammatory arthritis and ulnocarpal abutment.[19]
Epidemiology
The incidence of carpal ligament instability in current literature varies widely. Some studies have demonstrated the incidence of carpal ligament instability after wrist injury without fracture to be between 10% and 19%. Other studies have shown instability in 31% of distal radius fractures.[20] The scapholunate ligamentous complex is the most often injured carpal ligament.[21] The true incidence of scapholunate ligament injuries is unknown. Evidence of scapholunate ligament injury has been observed in 35% of cadaveric wrists, and 29% of the specimens with scapholunate ligament injuries had associated degenerative changes.[22] Injury to the lunotriquetral ligamentous complex is less common than scapholunate ligament injuries. The incidence of lunotriquetral ligamentous complex injury is also unknown; it is evident that degenerative tears of the proximal membranous component of the lunotriquetral ligament are common.
Pathophysiology
Scapholunate Dissociation
Injury to the scapholunate ligament complex most commonly occurs after a fall onto an extended and ulnar-deviated hand. When the carpus is axially loaded in extension, the proximal pole of the scaphoid shifts dorsally.[3] The lunate is held in place by the radiolunate ligaments. This increases strain on the dorsal scapholunate ligament, which may rupture depending upon the force of the injury. In high-energy trauma, such as motorcycle accidents, scapholunate dissociation may be the result of bony avulsions, most commonly of the scaphoid, rather than a mid-substance ligamentous failure. This is attributed to the scapholunate ligament's greater stiffness at higher strain rates.[5]
Complete injury to all 3 components of the scapholunate ligament may not cause radiographically significant scapholunate diastasis.[23] However, alterations to wrist biomechanics and kinematics can occur with isolated scapholunate ligament rupture.[24] These changes gradually weaken the secondary stabilizers of the scapholunate joint—the palmar radioscaphocapitate, scaphocapitate, and scaphotrapeziotrapezoid ligaments. Once these fail, radiographic evidence of scapholunate dissociation becomes more apparent.[7][25] Degenerative changes associated with scapholunate dissociation with resultant rotational deformity in the scapholunate joint are further discussed in the "Complications" section.
Lunotriquetral Dissociation
Injury to the lunotriquetral ligamentous complex commonly occurs after a fall onto an extended hand with the wrist in radial deviation, causing a concentration of force through the hypothenar eminence. The pisiform is driven into the triquetrum, causing the triquetrum to translate dorsally while the lunate remains constrained by the radiolunate ligaments within the lunate fossa. Failure of the lunotriquetral ligamentous complex may occur.[11] Disruption of all 3 components of the lunotriquetral ligament may cause slight gapping between the lunate and triquetrum. Over time, the secondary stabilizers of the lunotriquetral joint weaken, which can result in a rotational deformity.
History and Physical
Scapholunate Dissociation
Scapholunate dissociation may occur as an isolated injury, or it may be associated with distal radius or carpal bone fractures. Injury to the scapholunate ligamentous complex should be suspected in patients with persistent dorsal wrist pain following a fall onto an outstretched hand. During the acute phase following injury, the patient may demonstrate decreased grip strength and present with popping or clicking sensations during activities that axially load the wrist. Pain to the dorsoradial wrist may be exacerbated when the wrist is placed into extension and radial deviation. The wrist's range of motion may be limited secondary to pain. In chronic cases, the wrist range of motion may be within normal limits until significant degenerative changes occur. Scapholunate dissociation presents in various ways depending on the extent of degeneration within the joint. Presentations are described using the Watson classification, where stage 1 is predynamic, stage 2 is dynamic, stage 3 is static, and stage 4 is osteoarthritic.[2]
The physical examination of a patient with scapholunate dissociation typically reveals tenderness to palpation dorsally over the scapholunate interval. Localized swelling is observed in acute cases. Scapulolunate dissociation is diagnosed using the scaphoid shift test, also called the Watson shift test. This examination maneuver involves deviating the wrist from ulnar to radial while applying pressure volarly over the scaphoid tubercle. A palpable clunk or the presence of dorsal wrist pain is considered a positive test. Pathophysiologically, the clunk or pain occurs as the proximal pole is subluxated over the dorsal ridge of the radius. The scapholunate ballottement and scaphoid lift tests may also be positive.
Lunotriquetral Dissociation
An isolated injury to the lunotriquetral ligament can be subtle and potentially asymptomatic. Symptomatic lunotriquetral dissociation is typically observed in the presence of other extrinsic ligament injuries and is often associated with injuries to the triangular fibrocartilage complex. The lunotriquetral ligamentous complex is most commonly injured by falling on the wrist and landing on the hypothenar eminence. The patient may complain of persistent ulnar-sided wrist pain and decreased grip strength.[2]
Pain can be elicited by palpation over the dorsal lunotriquetral interval. Ulnar deviation with pronation and axial compression of the wrist can result in a painful snap.[12] The lunotriquetral ballottement test is used to test for lunotriquentral dissociation. This test is performed with the forearm in neutral rotation with the elbow supported on the examination table. The lunate is stabilized by the examiner's thumb and index fingers. The other thumb is placed over the triquetrum dorsally, with the examiner's index finger placed volarly on the triquetrum/pisiform. The triquetrum is translated volarly and dorsally while the lunate is stabilized. The test is positive if there is pain or increased motion compared to the contralateral, uninjured wrist.[1] The lunotriquetral shear and shuck tests can be performed, but their specificity is poor.
Evaluation
Scapholunate Dissociation
Standard wrist radiographs (posteroanterior, lateral, and oblique) should be performed routinely on any patient with a clinical history and physical examination suggestive of a scapholunate ligament injury. The standard views should be obtained by focusing the beam over the radiocarpal joint with the wrist in a neutral position, between supination and pronation.[6][26] Three Gilula lines (carpal arcs) should be evident within the carpal bones. Several radiographic findings and parameters have been described for scapholunate ligament injury, including:
Scapholunate interval widening
- Posteroanterior view
- Interval is normally ≤2 mm
- Interval of greater than 3 mm to 5 mm is suggestive of scapholunate dissociation [16]
- Interval widening can be accentuated with a clenched-fist view
Scaphoid cortical ring sign
- Posteroanterior view
- Occurs with excessive scaphoid flexion, causing interposition of the distal and proximal poles [16]
Scapholunate angle
- Lateral view
- Normal angle is between 45° and 60°
- Angle greater than 70° is indicative of scapholunate dissociation and a DISI deformity [3]
Capitolunate angle
- Lateral view
- Angle greater than 20° suggestive of scapholunate dissociation
Occasionally, the standard wrist radiographs can be normal after severe injury. In such cases of suspected wrist instability, the wrist should be subjected to maximum loading while performing the radiographs.[27] Four stress x-ray views are described: posteroanterior view with the wrist in radial deviation, ulnar deviation, and lateral views with the wrist in flexion and extension. High-resolution magnetic resonance imaging (MRI) is sensitive and specific for evaluating scapholunate ligament injuries. MRI should be considered when the radiographs and the physical examination are equivocal or for preoperative planning purposes.[27][28][29] Wrist arthrography can also be performed as it is highly sensitive and detects the presence of communication defects. Following wrist arthrography with MRI and computed tomography (CT) of the wrist is recommended. If further evaluation is needed, diagnostic wrist arthroscopy can be considered.[30][31]
Lunotriquetral Dissociation
The diagnostic evaluation for lunotriquetral dissociation includes radiography, arthrogram, MRI, and diagnostic arthroscopy. Radiographs should be performed first. Isolated injury to the lunotriquetral ligament typically appears normal on static radiographs. Therefore, radiographic evidence for instability may only be present on stress radiographs, as evidenced by the following findings:
- Disruption in the proximal Gilula arc
- Posteroanterior view
- Due to the proximal translation of the triquetrum or lunotriquetral overlap
- Lunotriquetral interval narrowing/subchondral cyst formation
- Posteroanterior view
- Suggestive of chronic injury
- Lunotriquetral angle
- Lateral view
- Normal angle is between -3° and 31°
- Angle becomes more negative (mean, -16°) with lunotriquetral dissociation
- Radial deviation stress view
- Lateral view
- Increased flexion of the scaphoid and lunate without a change in triquetrum position (VISI) [12][32]
An arthrogram can be performed using fluoroscopy, CT, or MRI. These studies should be interpreted cautiously, as normal wrists can have "abnormal" findings, especially in patients with ulnar-positive variance wrists. Up to 13% of normal wrists can show communication of the radiocarpal and mid-carpal joints, which can also occur after a lunotriquetral ligament injury. A study revealed that 59% of patients with unilateral ulnar-sided pain and a suspected tear of the lunotriquetral ligament based on arthrography had similar findings in the contralateral, asymptomatic wrist.[33] A wrist MRI may be inconclusive, and a negative MRI does not exclude a lunotriquetral ligament tear.[19] Lunotriquetral dissociation is difficult to diagnose based on radiography, arthrogram, and MRI alone. As a result, the gold standard for diagnosing lunotriquetral dissociation is wrist arthroscopy.[12][19]
Treatment / Management
Scapholunate Dissociation
Primary healing of the scapholunate ligamentous complex offers the patient the best opportunity to maintain normal wrist mechanics; surgical repair or reconstruction may be required. The chronicity of the injury and the presence of carpal arthrosis need special consideration, as this alters the viable treatment options.
Acute injury treatment aims to promote healing of the scapholunate dorsal component, reduce the scapholunate interval, maintain normal carpal alignment, prevent abnormal carpal mechanics that can result in degenerative changes, and limit damage to uninjured wrist structures.[34] The injury is considered acute if it has occurred within 6 weeks of presentation.[34][35][36] Once advanced degeneration of the carpal or distal radius articular surfaces has occurred, salvage procedures are indicated.
Multiple classifications exist to determine which treatment option is indicated for the patient's stage of instability.
Stage I: Partial ligament injury
- Immobilization with a thumb spica brace or cast and hand therapy with re-education of wrist proprioception [37]
- Arthroscopic ligament debridement with or without thermal shrinkage (if immobilization/therapy does not resolve symptoms)
- Percutaneous K-wire fixation of the scapholunate joint for stability while the partial tear heals
Stage II: Complete ligament injury with normal scapholunate alignment on static radiographs
- Repairable ligament
- Open dorsal scapholunate ligament primary repair (volar ligament repair not necessary)[16]
- Non-repairable ligament
- Dorsal ligament reconstruction
- Dorsal scapholunate capsulodesis
Stage III: Complete ligament injury with static scapholunate interval widening
- Repairable ligament
- Open dorsal scapholunate ligament repair with reduction of interval
- Non-repairable ligament
- Dorsal ligament reconstruction
- Dorsal scapholunate capsulodesis
Stage IV: Complete ligament injury with static scapholunate interval widening and increased scapholunate angle (DISI deformity)
- Reducible deformity: Ligament reconstruction
- Fixed deformity: Partial carpal arthrodesis, such as scaphotrapezialtrapezoidal or scapholunocapitate fusion
Stage V: Complete ligament injury with arthritic changes (scapholunate advanced collapse (SLAC) wrist)
- Treatment is dependent on the location of degeneration [38][39]
- Treatment may include a proximal row carpectomy or scaphoidectomy with 4-corner arthrodesis [40][41]
Lunotriquetral Dissociation
Effective treatment of lunotriquetral ligamentous complex injury is dependent on chronicity and the presence of carpal instability.[12][42] In patients with acute (typically less than 6 weeks) injuries without findings of instability on static radiographs, nonoperative management can be attempted initially.[12] If the patient fails to respond to conservative treatment, arthroscopy is indicated to determine the extent of the lunotriquetral injury. The arthroscopic classification of the injury can assist in determining the next step in operative management.[12] Managing chronic lunotriquetral ligament injuries depends upon whether the carpal alignment is reducible or fixed (VISI).
Acute injury less than 6 weeks from injury, no malalignment on static radiographs: Immobilization with or without mid-carpal corticosteroid injection
Acute injury with failed nonoperative management arthroscopy and injury classification
- Grade I: ligament attenuation, no gap between lunate and triquetrum
- Grade II: ligament attenuation, <2 mm gap
- Ligament debridement with K-wire fixation
- Grade III: ligament disruption, >2 mm gap
- Ligament debridement with K-wire fixation
- Grade IV: complete ligament disruption, able to pass arthroscope between lunate and triquetrum
- Open ligament repair [12]
Chronic injury with reducible carpal instability
- Ligament reconstruction
- Lunotriquetral arthrodesis
Chronic injury with fixed malignment (VISI deformity)
- Triquetrum-hamate arthrodesis
- Lunotriquetral arthrodesis and radiolunate arthrodesis [43][44]
An ulnar shortening osteotomy may benefit a patient with lunotriquetral dissociation, positive ulnar variance, and resultant ulnar abutment.[12][45]
Differential Diagnosis
The differential diagnosis for scapholunate ligament injury includes:
- Scaphoid fracture
- Kienbock disease (lunate avascular necrosis)
- Ganglion cyst
- Flexor carpi radialis tendinopathy
- Extensor carpi radialis brevis/longus tendinopathies
- CIND-DISI [5][2]
The differential diagnosis for lunotriquetral ligament injury includes:
- Ulnar impaction syndrome
- Triangular fibrocartilage complex tears
- Kienbock disease (lunate avascular necrosis)
- Triquetral avulsion fracture
- Pisotriquetral arthrosis
- Extensor carpi ulnaris tendon subluxation/tenosynovitis
- Distal radioulnar joint arthrosis
- CIND-VISI [12]
Prognosis
Scapholunate Dissociation
Patients with scapholunate dissociation have a better prognosis if treated before the onset of degenerative changes. One study revealed that 83% of patients who received treatment within 3 months of a scapholunate ligament tear remained asymptomatic and maintained scapholunate joint reduction over a 7-year follow-up period.[39][46] Similar results were found in another study that demonstrated lower failure rates and improved functional outcomes in patients receiving operative treatment for acute injuries compared to chronic injuries.[35] Ligament reconstruction has been shown to offer satisfactory pain relief and functional outcomes; however, residual wrist stiffness and decreased grip strength remain challenges.
Lunotriquetral Dissociation
Patients with acute lunotriquetral ligament injuries who undergo arthroscopic debridement can expect symptomatic improvement, especially if there is only a partial tear. Patients with chronic injuries are more likely to require a procedure. A study demonstrated that only 25% of patients with chronic injuries had symptom improvement with immobilization.[47] Lunotriquetral arthrodesis is associated with higher complication and re-operation rates than ligament reconstruction.[48] Complications include non-union and ulnocarpal impaction.
Complications
Scapholunate Dissociation
Dorsal intercalated segment instability (DISI)
A DISI deformity is 1 complication of chronic scapholunate dissociation.[49] Over time, rotational instability develops as the secondary stabilizers of the scapholunate joint, particularly the radioscaphocapitate ligament, weaken and fail. The scaphoid subsequently moves into flexion and pronation. The lunate moves into extension as its proximal portion is wider dorsally. The capitate then begins to subluxate dorsally and proximally as the lunate is oriented in extension. On lateral radiographs, the scapholunate angle is greater than 70°. DISI from scapholunate ligament injury is a dissociative carpal instability as the dysfunction occurs between bones within the same carpal row. CIND occurs if the dysfunction exists between the proximal and distal row or proximal row and radius.[4][3]
Scapholunate advanced collapse (SLAC) wrist
A SLAC wrist is a complication of chronic scapholunate dissociation and resulting DISI deformity.[50] The alteration in scaphoid and lunate alignment results in abnormal force distribution throughout the wrist.[51] SLAC wrist consists of 3 stages based on the location of degenerative changes initially described by Watson (with a fourth stage subsequently proposed). The radiolunate joint is spared in the SLAC wrist because the lunate fossa remains concentric.
- Stage I: Arthritis between the scaphoid and radial styloid
- Stage II: Arthritis between the scaphoid, radial styloid, and entire scaphoid fossa of the radius
- Stage III: Arthritis between the scaphoid, radial styloid, scaphoid fossa, and capitolunate joint
- Stage IV: Pan-carpal arthritis
Lunotriquetral Dissociation
Ventral intercalated segment instability (VISI)
VISI malignment is a complication of chronic lunotriquetral dissociation.[52][53][54][53] VISI occurs with gradual weakening of the lunotriquetral joint secondary stabilizers, which results in lunate flexion. The contact point between the capitate and lunate moves volarly, contributing to lunate flexion. Due to increased lunate flexion, the scapholunate angle decreases to less than 40° on static radiographs. As the lunate flexes, the capitate migrates proximally. Lateral radiographs demonstrate a capitolunate angle greater than 10°.[12] In lunotriquetral dissociation, the VISI malalignment is dissociative as dysfunction exists between bones of the same carpal row. VISI can also occur in a nondissociative carpal instability pattern where dysfunction occurs between the proximal and distal row or proximal row and radius. The complications of both scapholunate and lunotriquetral dissociation and instability often result in persistent pain, stiffness, and decreased grip strength.
Deterrence and Patient Education
Carpal ligament injury and instability can occur after a simple fall onto an extended hand. Patients with persistent wrist pain following a fall should seek consultation with a physician trained in hand and wrist injuries. Treatment of these injuries is ideally performed in the acute phase before chronic carpal changes occur. If these injuries are neglected, damage to articular cartilage can occur, resulting in wrist arthritis.[55]
Enhancing Healthcare Team Outcomes
Carpal ligament instability requires coordination among the interprofessional healthcare team, which includes primary care physicians, emergency medicine providers, orthopedic hand/wrist surgeons, nurses, and hand therapists. Carpal instability can easily go unrecognized, especially in the early stages. This type of injury must be considered in any patient with wrist pain following a fall onto an extended hand. A thorough physical examination and appropriate radiographs can assist providers in their medical decision-making. If there is clinical suspicion of carpal ligament injury, advanced imaging and a possible referral to a hand specialist should be considered. Acute treatment of these injuries can prevent the patient from experiencing chronic wrist pain and visibility. Hand therapists are essential in the management of such injuries. All interprofessional team members must communicate openly if they have concerns or note patient status changes to promote the best possible patient outcomes.